Treatment for long-standing edema in the eyelid is challenging. Here, a case of eyelid edema caused by immunosuppressant was treated by lymphaticovenular anastomosis (LVA), a treatment procedure established by Koshima, which required supermicrosurgical techniques. A preauricular lymphatic vessel with a diameter of about 0.2 mm was anastomosed to a vein (0.8 mm) using supermicrosurgery. The outcome of this case suggests that LVA is applicable for treatment of persistent eyelid edema related to immunosuppressant therapy.
Eyelid edema is a common postoperative finding that occurs after midface or calvarial craniofacial surgery and soft tissue surgery involving eyelids or removal of head and neck cancers. However, persistent eyelid edema is very rare as almost all cases are temporary with swelling subsiding over time. In contrast, the postoperative lower limb edema can be more persistent after significant trauma or surgery, likely due in part to the position of the region, in a dependent position compared to the upright position of the eyelids. Nonetheless, there are cases of long-standing eyelid edema related to rosacea and cancer treatments, specifically immunosuppressants.
Treatment for long-standing facial and eyelid edema is challenging. Standard physio-compression therapy is difficult due to the form and function of the affected area, which lends the conservative therapy to be ineffective. The face – lips, eyes, and nose – is difficult to create consistent compression even for the most-skilled physiotherapist. Furthermore, the face should be uncovered and kept open for communication and function during daily life activities, unlike the limbs, which can more easily be compressed during regular activities of daily life. Simple resection of eyelid edema is relatively easy, but there is a possibility of recurrence of the edema after surgery. Complete resection of the affected eyelid tissue is difficult because of functional and aesthetic problems.
As an important surgical treatment for lymphedema, the classic lymphaticovenous anastomosis (LVA) was established by Yamada [1] and O’Brien [2-4]. Unfortunately, it was ineffective due to poor technique and the insufficient materials, instruments, and microscopes in 1960-70’s. Recent development of LVA with the supermicrosurgical technique was established by Isao Koshima in 1994 [5]. So far, over 2,000 cases of limb edema have been treated by this surgical method, of which many reports conclude with excellent results, providing support for LVA as the firstline treatment for lymphedema [6,7]. We previously reported an effective LVA for persistent facial edema after removal of head and neck cancer [8]. However, the effectiveness of LVA has not yet been established for long-standing eyelid edema with or without previous surgery.
In this report, we present a case with persistent eyelid edema caused by immunosuppressant and treated with successful LVA and lymph node-vein bypass surgery.
A 62-year-old man presented with a complex renal history beginning with severe pyelonephritis at the age of 14, resulting in renal failure and need for hemodialysis at the age of 21, eventual renal transplantation from his father at the age of 31, and subsequent continuous immunosuppressant therapy. After decades of immunosuppressant therapy with drugs, he developed bilateral upper and lower eyelid edema. He presented with bloody bullous edema affecting the right side more severely than the left side (Figure 1). The patient suffered from disturbed visual fields bilaterally, which required drainage by a puncture from his ophthalmologist every 3 days. The patient’s quality of life and facial function were significantly impacted as he was concerned that the upper eyelid edema was impairing eyelid opening in addition to the overall aesthetic deformity. Despite 6 months of conservative treatment, the right-side eyelids continued to be significantly affected by the edema.
On August 29, 2017, the preoperative indocyanine green (ICG) injection study showed no lymphatic channels or lymph nodes. Under a local anesthesia, LVA was performed in the right preauricular region and a small lymph channel (0.2 mm) in the subdermal layer and vein (0.8 mm) was anastomosed with a 50-micron needle. In addition, a right preauricular lymph node was detected in the same area. The superficial membrane of the node was resected to make a small hole, namely lymphostomy, and the lymphatic fluid was expelled from the lymph node. A transected proximal end of the concomitant vein of the transverse facial artery was anastomosed to the lymphostomy, the hole in the lymph node (Figure 2). There was an excellent flow from both the lymphatic to the vein and the lymph node to the vein.
Immediately after surgery, the right eyelid edema was decreased and continued to progressively improve over 6 weeks on both sides. At 5 months after surgery (Figure 3), there was no recurrence of edema in either set of eyelids. There were no noted serious complications.

Figure 1. Preoperative appearance.
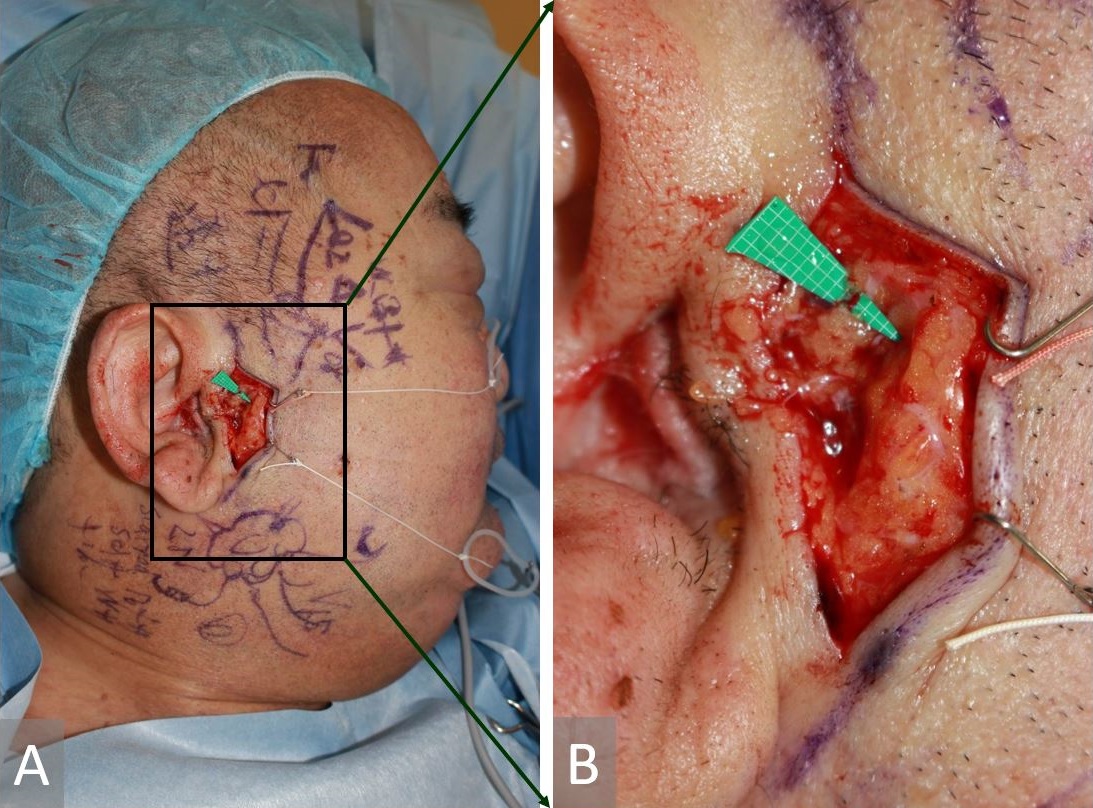
Figure 2. Intraoperative images. (A) The lymphatic channel was anastomosed to the vein, and lymphnodal-venous shunt was established. (B) Close-up view. Square on the green background indicates 1 mm.

Figure 3. Facial appearance five months after lymphaticovenular anastomosis. Marked improvement of edema is observed.
Etiology of Chronic Localized Non-Inflamed Eyelid Edema
Etiology of chronic localized non-inflamed eyelid edema includes trauma or disruptive causes involving surgery, radiation therapy for head and neck cancer [8], periocular hyaluronic acid filler injection for aesthetic treatment [9], and post-vitrectomy silicone leaks [10]. There are also syndromic complexes characterized by chronic eyelid edema. One is a rare form of acne rosacea referred to as Morbihan syndrome [11-14]. Another is Melkersson-Rosenthal syndrome [15,16], which is characterized by a triad of orofacial edema, facial nerve palsy, and furrowing of the tongue. Furthermore, a few immunosuppressants including pemetrexed [17], sirolimus [18], and everolimus [19] also share a link with chronic eyelid edema. Pemetrexed is an antimetabolite agent used for the treatment of mesothelioma and non-small-cell lung cancer. Both sirolimus and everolimus are inhibitors of mammalian target of rapamycin (mTOR) after solid organ transplantation.
Immunosuppressant-related lower eyelid edema was reported on persistent eyelid edema following solid organ transplantation. In these cases, the edema persists despite discontinuation of the medication and the surgical excision of the edematous eyelid achieves good results. In this case, it is assumed that the chronic immunosuppressant use is the cause of the chronic eyelid edema by likely injury and dysfunction of the periauricular nodes and/or lymphatic channels around the eyelids. The resulting damage of lymphatics was present, but milder on the left side; however, the persistent nature of the edema on the right necessitated intervention.
Why LVA is Feasible?
Similar to limb lymphedema, LVA is a curative treatment in which a new drainage pathway is created by constructing a lymphatic–vein bypass [6,7]. In this patient, lymph drainage was established by anastomosis of a subdermal venule with a congested lymphatic channel in the preauricular region. In addition, the right preauricular lymph node demonstrated high intra-nodal pressure, which was shunted using a nodal-venous anastomosis to the facial venous system. Both techniques increased the outflow of lymph drainage from the eyelid anatomic region.
Based on this case, anatomic visualization of obstruction was witnessed within the preauricular lymph node, indicating disruption or dysfunction of lymphatic damage proximal to the lymph node. This case also further supports the previous reports of chronic eyelid edema associated with immunosuppressant use.
Sites for Bypassing
We believed that the possible sites for bypass might be distal (preauricular) and proximal (submental) regions. Based on our previous electron microscopic study, smooth muscle cell degeneration of the lymphatic channel usually occurred from the proximal to the distal site. In addition, under local anesthesia, we needed a less invasive bypass in either site, not on both sides. Therefore, we tried preauricular area for bypassing, rather than submandibular region.
Other Surgical Reconstructions
Simple resection would not be effective for this patient due to the functional and aesthetic impact. In contrast, a partial resection with the risk of recurrence of the edema exists or even potentially worsening of edema is possible. Another option may include a lymph node or lymphatic channel transfer using groin or axillary tissue as a donor to the preauricular region [20-23]. Submandibular and supraclavicular lymph nodes should be avoided as these donor sites might be affected by the mechanism of damage related to the immunosuppressant. Also, these head and neck donor sites are too invasive to perform under local anesthesia. This is compared to performing an LVA or groin lymphatic transfer, which is easily performed under local anesthesia.
A case of long-standing eyelid edema related to immunosuppressant is reported here. A novel treatment involving a successful LVA and lymph node-venous bypass surgery under local anesthesia was introduced. These supermicrosurgery techniques are less invasive with lower potential for eyelid malposition compared to eyelid resection. We believe that all persistent eyelid edema could be indicated for LV bypass. It is assumed that the site of bypass is very important in each case. Wide facial and lid edema could be by auricular and submental bypasses. Mild localized lid edema could be an intra-auricular bypass in future.
Received date: August 13, 2018
Accepted date: October 12, 2018
Published date: November 13, 2018
None
None
This paper was presented at the American Society of Reconstructive Microsurgery on January 12, 2018 in Arizona, USA, the Chicago Breast & Lymphedema Symposium on April 26, 2018 in Chicago, USA, the European Federation of Societies for Microsurgery on May 8, 2018 in Belgrade, Serbia, and the Asia Pacific Federation of Societies for Reconstructive Microsurgery on May 12, 2018 in Antalya, Turkey.
Informed consent was obtained from the patient for publication of this case report and any accompanying images.
© 2018 The Author (s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Combining intraoperative ICG lymphography with NIR vein visualization can aid supermicrosurgeons in identifying lymphatic vessels and superficial venules to guide LVA incision placement. This guided approach significantly improves successful creation of LVAs when compared to the blind (anatomic) approach. In addition, the absence of linear ICG lymphographic patterns does not prevent formation of successful LVAs.
Immediate limb compression following the LVA procedure facilitates lymphatic drainage and increases the surgical efficacy by increasing the number of functioning anastomoses, and is a recommended postoperative practice.
Authors report a case of lower extremity lymphedema treated by LVA that preoperatively mapped not only lymphatic vessels by PDE, but also veins and venules using Veinsite™ .
Immediate limb compression following the LVA procedure facilitates lymphatic drainage and increases the surgical efficacy by increasing the number of functioning anastomoses, and is a recommended postoperative practice.
ICG lymphography is an invaluable tool in lymphedema management. Both immediate and delayed scans are needed when performing the study. The delayed scan needs to be performed at the time of the lymphographic plateau to appreciate the full extent of the pathology. Using a recumbent cross trainer, the lymphographic plateau can be achieved in 15 minutes following ICG injection. We have found this exercise enhanced ICG lymphography protocol worthwhile of adoption by high volume lymphedema centers to raise diagnostic accuracy and efficiency.
This article holds critical relevance for healthcare professionals, particularly in the fields of microsurgery, oncology, and vascular medicine. It thoroughly examines the diagnostic challenges faced in distinguishing between recurrent lymphedema and deep vein thrombosis in elderly cancer patients following lymphovenous anastomosis surgery. It highlights the significant risk of misdiagnosing deep vein thrombosis as lymphedema, a mistake that can delay critical treatment due to their clinical similarities. The case study of a 79-year-old patient emphasizes the importance of a comprehensive reassessment, considering the patient's entire medical history, including the effects of cancer treatments like immunotherapy. The article stresses the need for a holistic approach to patient management and the utilization of advanced diagnostic tools for accurate diagnosis and treatment. It is essential reading for its insights into the complex dynamics of postoperative care and the critical importance of accurate diagnosis in treating elderly cancer patients effectively.
Combining intraoperative ICG lymphography with NIR vein visualization can aid supermicrosurgeons in identifying lymphatic vessels and superficial venules to guide LVA incision placement. This guided approach significantly improves successful creation of LVAs when compared to the blind (anatomic) approach. In addition, the absence of linear ICG lymphographic patterns does not prevent formation of successful LVAs.
Immediate limb compression following the LVA procedure facilitates lymphatic drainage and increases the surgical efficacy by increasing the number of functioning anastomoses, and is a recommended postoperative practice.
The authors proposed a new less invasive island flap, namely the first metatarsal artery capillary perforator flap. The advantages of this flap include the preservation of the first metatarsal artery and the adiposal tissue in the web space, thereby preventing compression around the remaining deep peroneal nerve.
LVA and vascularized lymph node transfer VLNT are established lymphedema treatments. However, LVA is only effective for early disease and VLNT can cause donor-site lymphedema and contour deformity. VLVT is free of these limitations. The authors described their experience of a new VLVT technique.
Osteoarthritic finger joints are often repaired with joint implants, arthrodesis, or a vascularized interphalangeal joint graft. However, grafts can damage the donor toe. Based on the results of this study, the authors suggest that vascularized distal interphalangeal joint transfers from the second toe may be suitable for reconstructing these defects through microsurgery.
The article is accepted for publication.
The revised manuscript is accepted for publication.