Objective: Cholesteatoma is a locally invasive condition; however, a comorbidity of depression could be a risk factor of systemic morbidity and mortality. A relationship between cholesteatoma and depression has been observed in clinical practice; however this link has not been firmly established in the literature. This study sought to estimate the risk of developing depressive disorder (DD) following diagnosis with cholesteatoma.
Methods: In the study, we analyzed data from the Longitudinal Health Insurance Database of Taiwan. A total of 1820 patients newly diagnosed with cholesteatoma between 1997 and 2007 were included with a comparison cohort of 9100 matched non-cholesteatoma enrollees. Each patient was followed for 3 years to identify the subsequent development of DD. Cox proportional hazard regression analysis was performed to compute adjusted 3-year hazard ratios.
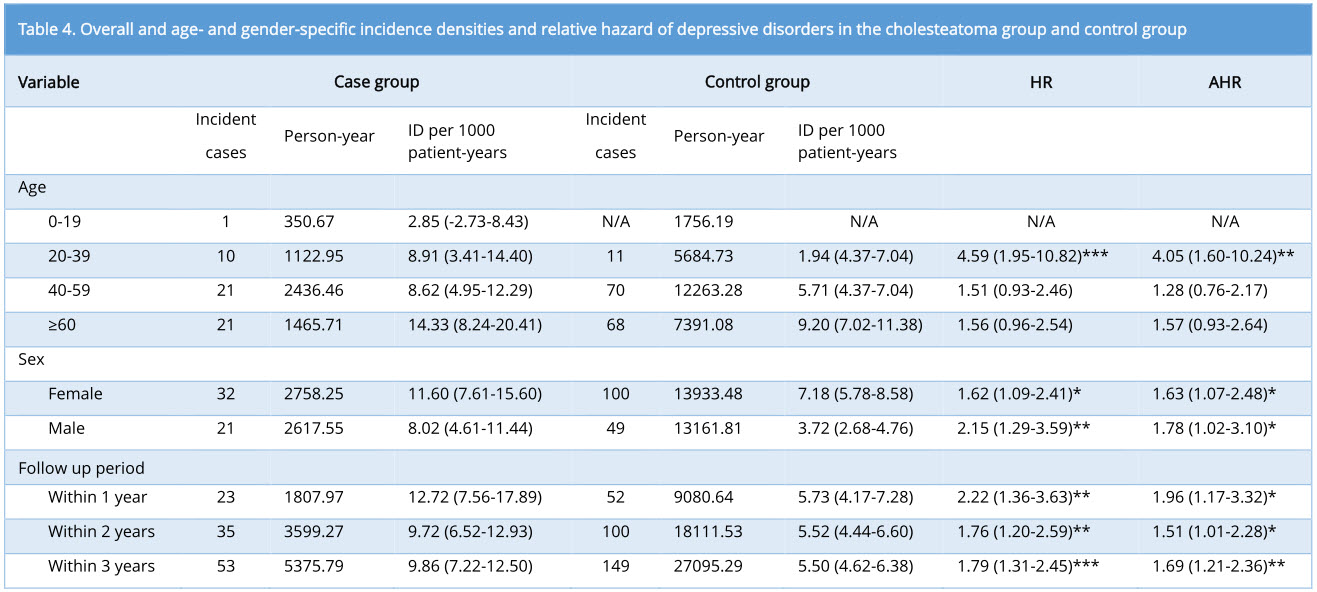
Results: Of the 10,920 patients in the sample, 53 individuals (2.9%) from the cholesteatoma cohort, and 149 (1.6%) from the comparison cohort were subsequently diagnosed with DD during the 3-year follow-up. The incidence of DD per thousand person-years was approximately twice as high among patients with cholesteatoma (9.86) as among those without cholesteatoma (5.50). After adjusting for potential confounders, patients with cholesteatoma were 1.69 times (95% CI = 1.21-2.36, P = 0.002) more likely to suffer from DD within 3 years compared to those without cholesteatoma.
Conclusion: This is the first study to demonstrate a prospective link between cholesteatoma and subsequent DD within a three-year follow-up. Routine psychiatric screening among cholesteatoma patients is essential for the early detection and timely treatment of depression.
Cholesteatoma is a well-demarcated lesion which develops from an abnormal growth of keratinizing squamous epithelium in the temporal bone [1]. The annual incidence of cholesteatoma is between 9.2 and 12.6 cases per 100,000 adults, with predominance in Caucasian populations [2]. Cholesteatoma is histologically benign but behaviorally malignant [3]. The dysregulation of cell growth control with local invasive characteristics is the major mechanism underlying widespread structural destruction in the middle ear cleft. The goal of treatment is typically complete disease eradication. Given the fatal capacity of intracranial complications, cholesteatoma remains a risk factor of morbidity and mortality in areas where access to appropriate medical care may be limited [4]. Patients with cholesteatoma are susceptible to frequent recurrence of foul-smelling otorrhea, hearing impairment, and tinnitus [4]. Depression commonly occurs in the context of medical conditions, with a prolonged impact on patients' quality of life [5]. Thus, it is reasonable to assume that the psychological burden associated with cholesteatoma could cause a patient to become socially withdrawn and potentially lead to the development of depressive disorder (DD).
Investigating the potential link between physical and mental illnesses may provide clues to enable the early detection of DD. Medical comorbidity with DD is a major public health concern [6]. Clinicians dealing with cholesteatoma have tended to place primary focus on hearing outcomes and disease control, such that the relationship between cholesteatoma and depression remains unclear. However, it is worth noting that one previous case report did address this topic [7].
In this current study, we sought evidence to support our hypothesis that patients with cholesteatoma may face an elevated risk of developing DD. To the best of our knowledge, this is the first population-based study to investigate a link between depression and cholesteatoma.
Ethics statements
The Institutional Review Board of Taipei Veterans General Hospital exempted this study from review because it used existing, deidentified public use data (VGHIRB No. 2015-04-002AC).
Data source
The National Health Insurance (NHI) program was implemented in 1995 and currently covers 99% of the Taiwanese population [8]. Claims data are maintained in the National Health Insurance Research Database (NHIRD), which is managed and audited by the National Health Research Institutes (NHRI). The NHIRD includes data related to demographics, clinical visits, diagnostic codes, prescriptions, and expenditures. To validate the completeness and accuracy of the claims data, the NHRI conducts random patient interviews, annually reviews medical records, and employs random sampling of claims from every hospital. Hundreds of researchers have previously employed NHI data in peer-reviewed research [8,9].
This retrospective study used a subset of the NHIRD, the Longitudinal Health Insurance Database (LHID2005), which enables researchers to follow-up on all medical service utilization by 1 million enrollees randomly selected from the NHIRD in 2005. The NHRI has stated that there are no statistically significant differences related to age, sex, or health-care costs between the LHID 2005 and the NHIRD [8].
We examined ambulatory and inpatient care data for patients in the LHID2005 from 1997 to 2007. To ensure privacy, the original identification number of each patient in the LHID2005 is encrypted before it is linked to personal health-care information.
Participants
A study group and a comparison group were assembled for a retrospective cohort examination of the relationship between cholesteatoma and depression. Patients newly diagnosed with cholesteatoma between January 1, 1997 and December 31, 2007 were identified according to diagnostic criteria from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM code 385.3, 385.30, 385.31, 385.32, 385.33). The date of the first diagnosis with cholesteatoma was assigned as the index date for each patient in the study. To ensure the accuracy of data, only patients with ≥2 ambulatory visits or ≥1 inpatient visits for cholesteatoma were included in the case cohort. Five patients without cholesteatoma were randomly matched to each patient in the cholesteatoma cohort based on age, sex, and index year. Patients with a history of depression (ICD-9-CM code 296.2, 296.3, 300.4, 311) were excluded from this study, and hypertension, hyperlipidemia, diabetes, and obesity were treated as potential confounders for the risk of depression. Finally, we adopted similar criteria for depression as we did for cholesteatoma, including in the cohort only cases with ≥2 ambulatory visits or ≥1 inpatient visit. In addition, depression diagnostic codes had to have been assigned by a psychiatrist.
Level of urbanization
We matched the levels of urbanization to avoid potential confounders, such as unmeasured neighborhood socioeconomic characteristics between the study cohort and comparison cohort. In the LHID 2005, the 359 towns/cities in Taiwan are stratified into 8 urbanization categories according to criteria established by the NHRI, with 1 indicating the highest level of urbanization and 8 indicating the lowest. The criteria includes population density (persons per km2), the percentage of people with a college-level education or higher, the percentage of people aged 65 years or older, the percentage of agricultural workers in the local population, and the number of physicians per 100 000 people. However, the number of cholesteatoma cases in levels 4, 5, 6, 7, and 8 were low; therefore, these levels were combined into a single urbanization group, level 4.
Statistical analysis
Pearson chi-square tests were performed to examine differences in categorical data between cholesteatoma and comparison cohorts, including level of urbanization, monthly income, geographic region, and potential confounders (i.e. hypertension, hyperlipidemia, diabetes, or obesity). Parametric continuous data for the two cohorts, including follow-up time, were compared using the Students t-test.
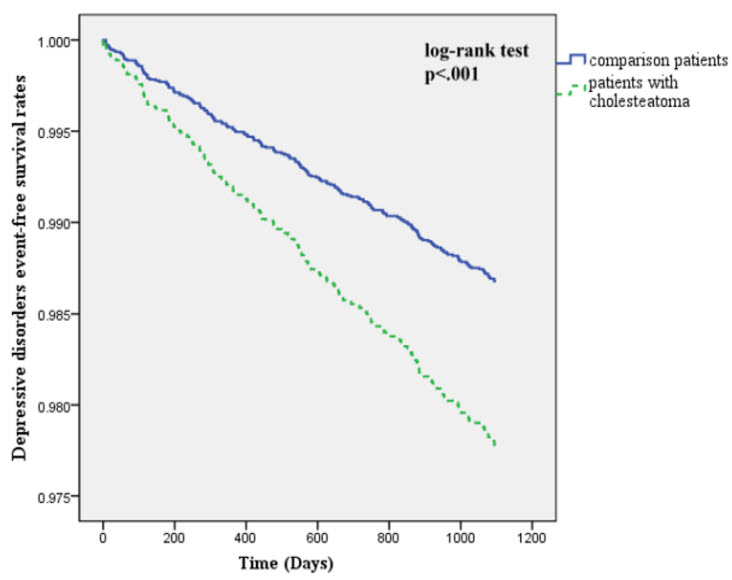
DD-free survival was calculated for all patients diagnosed with depression between the date of the first hospitalization or ambulatory visit for cholesteatoma and the end of the study period (December 31, 2010) or death, whichever came first. We calculated the three-year DD-free survival rates using the Kaplan-Meier method. We also applied the log-rank test to examine differences in DD-free survival rates between cohorts. Cox proportional-hazard regression analysis stratified by sex, age group, index year, and relative confounders was used to examine the risk of DD in cholesteatoma and comparison cohorts during the 3-year follow-up period. We also examined the effects of sex, age, hypertension, hyperlipidemia, diabetes, and obesity on the relationship between cholesteatoma and depression events. For the stratified Cox regression analysis, patients were divided into four categories: 0-19, 20-39, 40-59, and ≥ 60 years. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated to represent the risk of depression in the cohorts before and after stratification based on age or sex. Comparison results had to have a 2-sided P value of < 0.05 to be considered statistically significant.
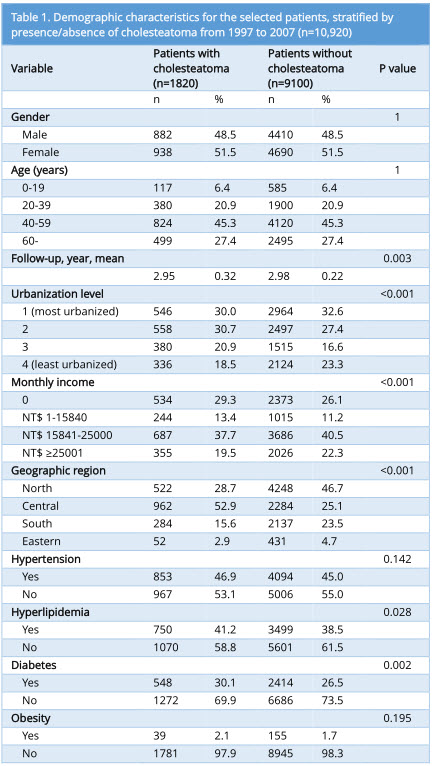
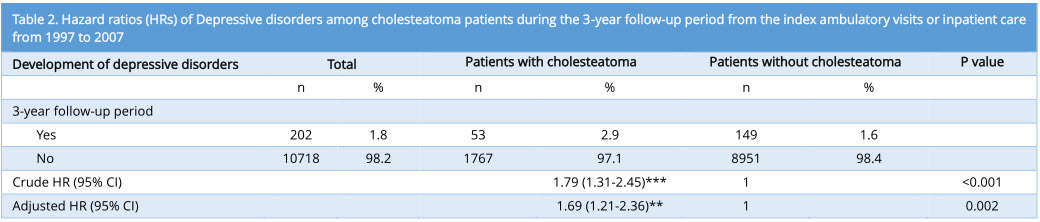
A total of 1820 and 9100 patients were included in the cholesteatoma and comparison cohorts, respectively. Sociodemographic and comorbidity data for both the cholesteatoma and comparison cohorts are listed in Table 1. Cholesteatoma patients presented higher rates of hyperlipidemia (P = 0.028) and diabetes (P = 0.002) than did the comparison cohort. Cholesteatoma patients were also more likely to have a lower monthly income (P < 0.001) or reside in central Taiwan (P < 0.001). No statistically significant differences in hypertension (P =0.142) or obesity (P =0.195) were observed. During the 3-year follow-up, 53 (2.9%) of the cholesteatoma patients and 149 (1.6%) of the patients in the comparison group developed DD. Cox regression analysis revealed that the crude HR of DD was 1.79 times higher (95% CI = 1.31–2.45; P <0.001) among cholesteatoma patients than among the comparison cohort. The risk of DD remained significant even after adjusting for potential confounders (adjusted HR: 1.69, 95% CI: 1.21–2.36; P=0.002; Table 2), and cholesteatoma patients presented a significantly lower 3-year DD-free survival rate (P < 0.001; Figure 1).
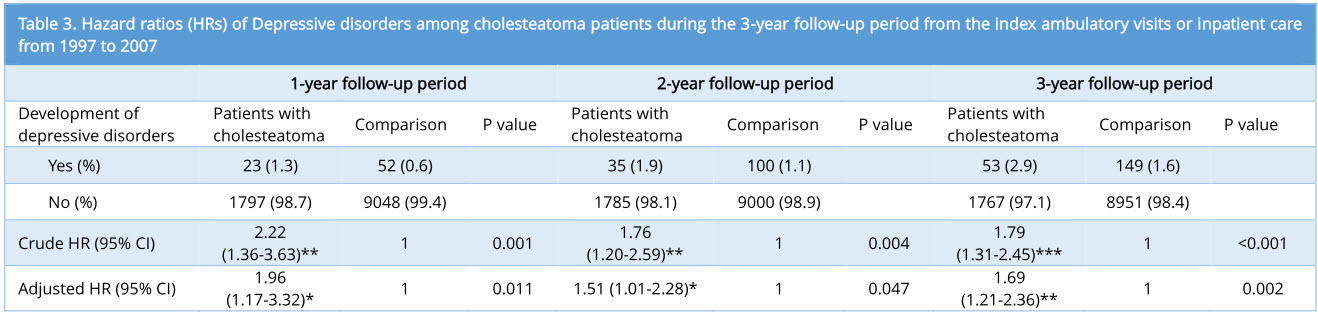
To investigate whether cholesteatoma is a time-dependent risk factor for DD, patients were divided into three subgroups according to the duration of follow-up (i.e. 1, 2, or 3 years). In all three follow-up periods, the risk of developing DD remained significantly higher in the cholesteatoma group than in the comparison cohort both before and after adjusting for potential confounders (Table 3).
In the three-year follow-up period, the overall DD incidence density was higher among patients with cholesteatoma (9.86 per 1000 person-years) than in the comparison cohort (5.50 per 1000 person-years) (Table 4). Gender and age stratified analysis of incidence revealed that women had a higher incidence of DD than men (11.60 vs. 8.02 per 1000 person-years) and that patients aged over 60 years had a higher incidence of DD (14.33 per 1000 person-years) than all other age groups (Table 4).
Cox regression analysis revealed that the difference in the risk of DD between male patients and the male control group (adjusted HR 1.78, 95% CI =1.02–3.10; P < 0.05) was more pronounced than was the difference in risk of DD between female patients and the female control group (adjusted HR 1.63, 95% CI =1.07–2.48; P < 0.05) (Table 4). In addition, the difference in the risk of DD among patients aged 20 to 39 years and the control group of patients of the same age (adjusted HR 4.05, 95% CI =1.60–10.24; P < 0.01) was higher than the difference in the risk of DD between patients and controls in other age groups. With regard to follow-up period, it was found that patients with cholesteatoma had the highest risk of developing DD within one year of diagnosis (adjusted HR 1.96, 95% CI =1.12–3.23; P < 0.05) (Table 4).
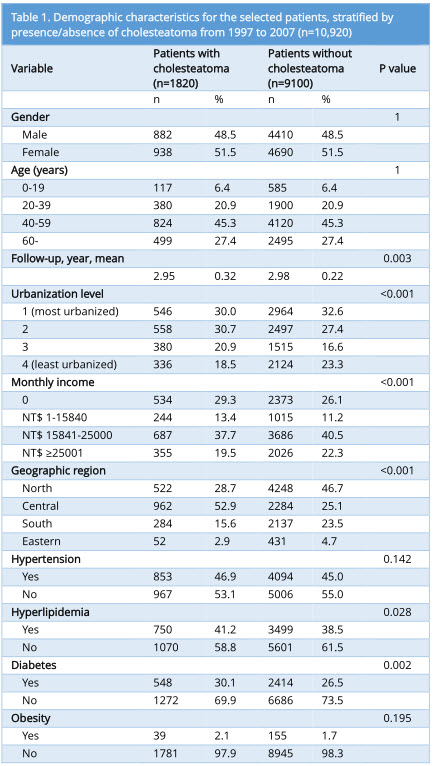
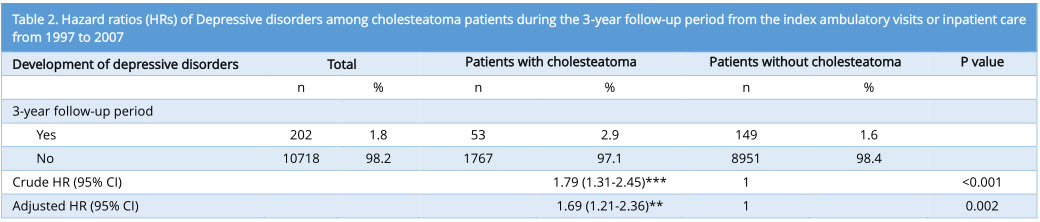
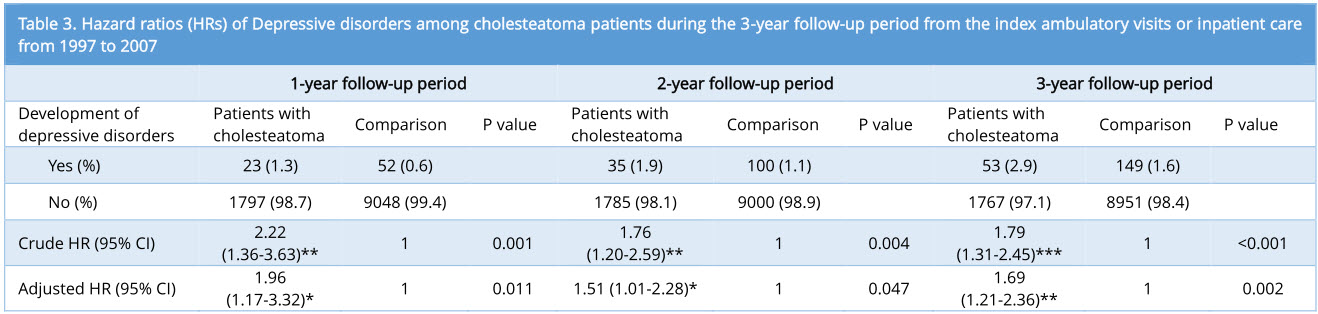
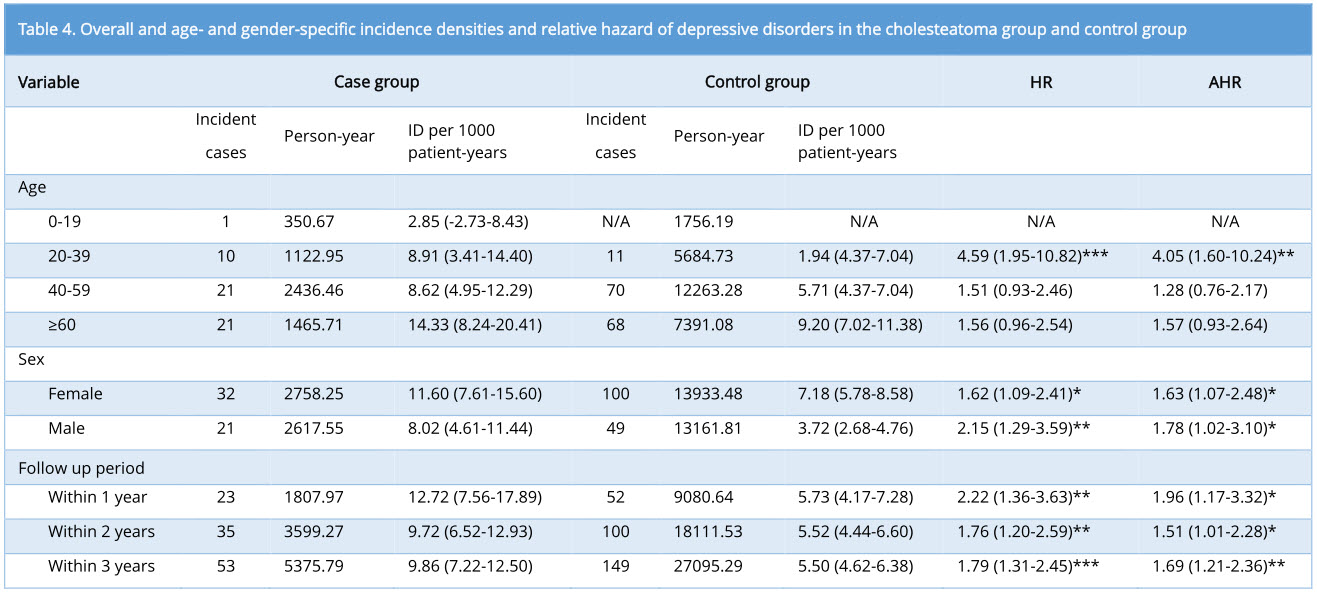
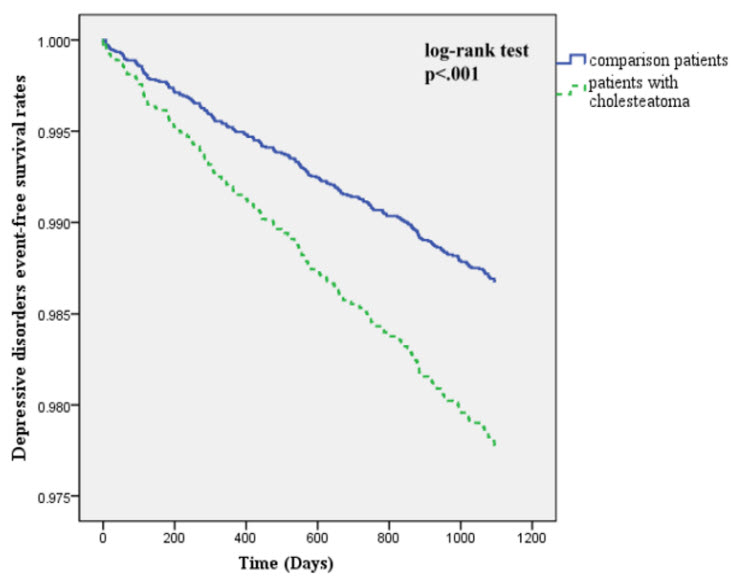
Figure 1. Depression-free survival rates in the cholesteatoma and control groups from 1997 to 2007.
Despite a lack of research into the potential relationship between cholesteatoma and DD, changes in psychological status have been observed in patients with cholesteatoma [7]. A lack of evidence supporting a link between the two disease entities reflects the priority of surgeons, which leads them to treat the disease according to the rate of recidivism and hearing outcomes [10,11]. To the best of our knowledge, this is the first large-scale epidemiologic study to investigate the risk of developing DD following cholesteatoma diagnosis.
In this 10-year cohort study on 10,920 patients, we identified a prospective link between cholesteatoma diagnosis and the development of DD. Compared to those without cholesteatoma, the risk of developing depression increased by 1.90-, 1.51-, and 1.69-times in 1-, 2-, and 3-year follow-up periods, respectively, following adjustment for co-variables (Table 3). We also determined that the younger cohort (aged 20 to 39 years), male patients, and patients that had been diagnosed within one year had the greatest risk of developing DD (Table 4).
The underlying mechanisms linking depression to cholesteatoma are not yet clear; however, a number of plausible biological and psychosocial factors could play a role. First, invasive cholesteatoma is associated with poor functional prognosis [12,13]. Second, cholesteatoma can have profound and far-reaching consequences for daily life, such as the frequent occurrence of foul-smelling otorrhea, hearing loss, tinnitus, vertigo, and even the possibility of facial paralysis or intracranial fatal complications [4]. Patients who are not candidates for surgery (e.g. immunocompromised and the elderly) require frequent visits to the clinic for ear cleaning, which can be highly inconvenient, particularly for busy patients and those who live in rural or remote areas. Patients with problems associated with a post-operative cavity may also face the need for lifelong aural toilet, limitations in their exposure to water, caloric stimulation vertigo when cold air or water enters the cavity, delayed recovery, a cosmetically unpleasing appearance, or difficulties in fitting hearing aids [4]. The threat of recidivism (5-17% for canal wall down technique; 9-70% for canal wall up technique) [14] may also raise fears among patients regarding the need for repeated surgeries, which imposes an additional economic burden on patients [4]. Given the aforementioned difficulties, patients may become psychologically inhibited and socially withdrawn, such that DD would be a possible consequence of the physical impairments brought about by cholesteatoma.
Our study found previously unrecognized evidence linking DD to cholesteatoma, and these findings could have strong clinical implications. First, DD has been implicated in poor adherence to medical treatment [6,9,15]. Poor follow-up compliance is a major concern of surgeons, even in cases where cholesteatoma has been entirely eradicated, due to the difficulties associated with post-operative recidivism, particularly the need for repeated revision surgeries [16]. Second, research has revealed that depression can increase the morbidity of existing medical conditions [5,6,17]. The medical costs of comorbid depression have also been shown to exceed those of medical illness alone. Moreover, functional impairments associated with depression may further increase the economic burden faced by patients [6,17]. These issues underline the importance of raising awareness among clinicians with regard to the possibility of comorbid depression in patients suffering from cholesteatoma.
Researchers have demonstrated the significant effects that depression can have on adverse health behaviors (e.g. unhealthy diet, smoking, and sedentary lifestyle) [17], which are now seen as being important risk factors for heart disease, stroke, and other conditions [18]. Functional impairments including occupational disability, reduced productivity, and increased healthcare utilization are common among patients with major depression [17]. The World Health Organization has predicted that depression will continue to be a leading cause of disability, second only to cardiovascular disease by 2020 [19]. A continued increase in disabilities associated with depression implies that many cryptic cases will remain undetected [5,6]. Our discovery of a prospective link between cholesteatoma and depression may serve as an early warning sign for potentially unrecognized DD.
One major concern regarding our observations that must be addressed is the true incidence of DD following cholesteatoma diagnosis. In Taiwan, the perceived social stigma of a psychiatric diagnosis often raises fear among patients. Few patients voluntarily report depressive symptoms during physical examinations, and many patients with depression are unwilling to seek psychiatric care. Moreover, some patients fail to meet the diagnosis criteria for clinical depression, despite the presentation of depressive symptoms. Thus, the true incidence of DD following cholesteatoma diagnosis may have been underestimated. This issue warrants further attention.
Depression among children with cholesteatoma should also be given further consideration in future research. The rate of cholesteatoma recidivism among children is reported to be 2 to 10 times higher than among adults, which ultimately leads to a higher incidence of revision surgeries [4]. In addition, hearing loss can have a profound effect on language development, learning, and academic performance. Children who suffer from cholesteatoma are prone to social isolation, which can lead to depression and hinder the development of social skills [11]. Nonetheless, in this study, the incidence density of DD among children with cholesteatoma was only 2.85 per 1000 person-years, which is far lower than incidence rates observed in other age groups (Table 4). This paradoxical observation between children and adults may be explained by the fact that children are more susceptible to social stigma or psychological scarring. Thus, it is highly likely that the true rate of depression among children with cholesteatoma has been underestimated, which suggests the need for routine screening of depressive symptoms among children.
The strength of this study lies primarily in the application of the nationwide NHI dataset. No previous studies have sought to link cholesteatoma to DD, which may be partly due to low cholesteatoma incidence, the small sample size typical of individual institutes, and high rates of individuals lost to follow-up [11,16,20]. This current population-based survey provides strong evidence to validate the newly discovered link between cholesteatoma and DD thanks to a large sample size, minimal selection bias, and the complete follow-up of cohort members, given that NHI program is a compulsory universal healthcare system. The accuracy of diagnosis in this study is considered acceptable, based on the following: (1) the healthcare system provides complete medical coverage to nearly all residents in Taiwan (99%) and (2) very low copayment requirements (3 to 15 US dollars) lead to high utilization of medical services, which reduces the possibility of underestimating the number of cases [20]. In addition, patients with otologic symptoms (e.g. otorrhea and hearing loss) are generally referred for further otolaryngologic examination, such that cholesteatoma is theoretically diagnosed or confirmed by an otolaryngologist. Furthermore, in Taiwan, only psychiatrists are permitted to make a diagnosis of DD [9].
Despite these strengths, findings in this study should be interpreted with caution. First, an epidemiological association does not necessarily imply biological causation. In this study, we analyzed newly diagnosed cholesteatoma patients to avoid the potential effects of chronicity [9]. It should be noted however, that some of these cases may not have been newly developed. A possible time lag between development and diagnosis may impede estimations about the effects of disease duration on the occurrence of comorbidities. Furthermore, the findings of this study can be generalized to the Taiwanese population; however, applicability to other individuals of other ethnicities requires further validation. Finally, the results obtained in this population-based study require additional confirmation in comparable, longitudinal prospective studies.
Newly discovered epidemiological evidence linking cholesteatoma to depression suggests that routine screening and monitoring of psychological status among cholesteatoma patients is warranted. Policies aimed at the early detection and timely treatment of comorbid depression following diagnosis with cholesteatoma could enhance health promotion and disease prevention.
Received date: August 16, 2017
Accepted date: September 16, 2017
Published date: October 03, 2017
© 2017 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
The present study demonstrated that TEES could be a satisfying alternative to traditional microscopic surgery for the management of congenital cholesteatoma, even in pediatric patients. However, one-handed surgery demands greater skill and requires more practice to achieve a good outcome.
Authors reported a case of cholesteatoma that mimicked facial neurinoma. To avoid confusion in such cases, diffusion-weighted MRI may be useful in preoper-ative differential diagnosis.
The author reports a case involving a 59-year-old man with delayed presentation of a huge mastoid cholesteatoma complicated by skull base erosion and cerebrospinal fluid leakage. Delayed presentation of this disease entity can have negative health consequences for patients. Regular otologic examinations, audiologic follow-up, and imaging examinations are viewed as the most effective strategies for the prevention of this type of situation. Early recognition of cholesteatomas is essential, as appropriate and timely treatment can prevent this rare comorbid condition from becoming fatal.
The authors report a case of otogenic Lemierre's syndrome in a male patient who presented with atypical symptoms and was subsequently treated aggressively with antibiotics and surgery. In this article, the authors demonstrate how they could have avoided serious complications by diagnosing and treating the patient earlier. The authors suggest key points that should be noted in clinical practice in order to prevent misdiagnosis or delayed diagnosis of Lemierre's syndrome.
The authors describe a 41-year-old man who suffered retraction-related complications that may have been missed or delayed. The present case illustrates the potential dangers associated with tympanic retraction pockets, despite the fact that their bottoms are clear and clean. The article discusses the reasons for the lack of consensus among otologists regarding the appropriate way to treat tympanic membrane retractions. There is further discussion regarding the challenges associated with early surgical intervention.
This study investigates the efficacy of conservative management using 5-fluorouracil (5-FU) for treating cholesteatoma in ambulatory care settings, offering an alternative for patients who prefer to avoid surgery. Over 13 years, 15 ears of 14 patients were treated with a 5% 5-FU cream and assessed using Takahashi's efficacy criteria. The results revealed positive outcomes, with 87% of cases deemed good and 13% as fair, with no poor evaluations. This approach may be suitable for specific populations, such as older adults and individuals in remote areas with limited access to specialized healthcare services.
This current review addresses the topic of therapeutic strategies for idiopathic SSNHL from the perspective of neuroplasticity. Assertions pertaining to the plausibility of this approach are based on a large body of evidence from animal experiments and recent studies on humans.
The clinical significance of otitis media with effusion (OME), a complication associated with cleft lip/palate (CLP), is often overlooked in children. The author reviews the pathogenesis, clinical manifestations, and diagnoses of OME in children with CLP as well as the controversies surrounding treatment. He also provides a flowchart to guide the management of OME in children with CLP.
Constraint-induced music therapy (CIMT) has been shown to enhance hearing recovery in patients with sudden sensorineural hearing loss (SSNHL) by preventing maladaptive reorganization of the auditory cortex. This study was the second research to provide scientific evidence related to the neuroplasticity of the central auditory nervous system in response to constraint-induced acoustic rehabilitation.
According to this article, Meniere's disease might actually be a generic term referring to an inner ear disorder that causes vertigo and hearing loss. The author suggests that physicians should pay more attention to discussing any pathological changes associated with hearing loss and vertigo with patients rather than narrowly focusing on confirming the diagnosis of diseases.
The terminology for describing the study type is a bit unclear in my point of view. In my understanding the study is a retrospective cohort study with a cohort of patients with cholesteatoma and matched controls that was followed for occurrence of depression. Thus it is one cohort of people with and without the exposure, not separate cohorts as implied by the wording used by the authors.
ResponseThank you for this helpful suggestion. Our research is a retrospective cohort study. To avoid ambiguity in the definition, we have revised the title of the manuscript to read “Increased Risk of Depression in Patients with Cholesteatoma: A 3-year Nationwide Population-Based retrospective cohort study.” We have also added the following statement in the “Participants” section of the revised manuscript: “A study group and a comparison group were assembled for a retrospective cohort examination of the relationship between cholesteatoma and depression”.
The idea of exploring the relationship between cholesteatoma and depression is interesting. To ensure the accuracy of newly diagnosed cases, a wash-out period should be applied.
ResponsePatients with a history of depression (ICD-9-CM codes 296.2, 296.3, 300.4, and 311) or cholesteatoma surgery were excluded from this study. We re-processed original data using the revised inclusion criteria and found that, for the majority of patients with DD(18/20, 90%), at least six months passed between the diagnosis of cholesteatoma and the diagnosis of depressive disorder. The remaining 10% of cases should only have a minor effect on risk estimates.
The risk of developing depression following diagnosis with cholesteatoma may not be sufficiently high to justify a routine psychological screening of patients, from the perspective of public health policy. However, depression can nonetheless be viewed as a cause of increased morbidity and mortality in patients suffering from a chronic disease, and this leads to increased health care utilization as well as higher health care costs.
In particular, the link between the two entities with statistical significance is a new concept for surgeons dealing with cholesteatoma, providing clues to enable the early detection of depressive disorder. We hope this new finding in the field of cholesteatoma surgery may arouse clinicians' attention regarding the importance of evaluation for depressive disorder in patients with cholesteatomas.
Checked the revised article. It can be accepted for publication.
Accepted for publication.
Accepted for publication.