Objective: Compare birth outcomes after implementation of an evidence-based guideline for managing the second stage of labor in women with epidural anesthesia.
Methods: This is a pre-post retrospective cohort study of birth outcomes (vacuum assisted delivery, cesarean delivery, pushing time, and total length of the second stage) at a community hospital after modifying and implementing an evidence-based guideline for delayed pushing in the management of second stage labor.
Results: 403 records of women giving birth during a three-month period prior to guideline implementation were compared with those of 429 women after the guideline was adopted. The post-guideline implementation group had lower odds of vacuum assisted births than the pre-guideline implementation group (aOR 0.47 [0.29-0.75], P < 0.001). The difference in median length of the second stage was not found to be statistically significantly different (P = 0.053), and active median pushing time was shorter (31 minutes) post-guideline compared to pre-guideline implementation (39 minutes) and even shorter with documented adherence to the guideline (25 minutes). No differences were identified in 5 minute Apgar, episiotomy, 3rd degree laceration or cesarean birth rates. Among the 429 women in the post-guideline group 217 (51%) delayed pushing compared with 22/403 (6%) in the pre-guideline group (P < 0.001). Use of the guideline was explicitly documented for 247/429 (58%) women, of whom 192/247 (78%) delayed pushing. Only 25 (14%) of the 182/429 (42%) women with partial or no documented adherence delayed pushing. Possible reasons for lack of adherence documentation were not collected.
Conclusions: Implementation of an evidence-based guideline for delayed pushing was associated with fewer vacuum assisted deliveries and reduced active pushing time without concurrent increase in overall length of second stage. Using a specific guideline for delayed pushing may improve outcomes and provide a model to standardize care during second stage labor for women with epidural anesthesia.
Managing the second stage of labor continues to be a topic of debate in maternity care. Preventing unnecessary cesareans and reducing maternal and neonatal morbidity remain important goals [1-4]. Labor management decisions are commonly made based on the length of time a woman has been completely dilated [5]. One method to reduce cesareans is to re-evaluate the management of second stage, specifically delayed pushing. A consensus recommendation in 2014 from the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal Fetal Medicine (SMFM) recommends that women with epidural anesthesia be allowed more time in second stage labor before diagnosing arrest of labor. This recommendation prompted a careful review of the literature, specifically regarding maternal and neonatal outcomes and the use of a guideline to standardize second stage management [1].
The notion that complete cervical dilation heralds the initiation of immediate pushing regardless of fetal station, position, maternal urge or the presence of epidural anesthesia, has come under repeated challenge [6-16]. A number of reports have indicated that delayed pushing for properly selected women may improve outcomes and patient satisfaction, especially in second stage labor for women with epidural anesthesia [12-16]. Multiple studies, including one meta-analysis comparing delayed with immediate pushing, have demonstrated significant positive effects, including: less fatigue [11,17], decreased active pushing time [7,11,13- 14,17-19], increased vaginal birth rates [12-13,20], and decreased operative delivery [12,13]. In contrast, other studies have found no decrease in operative delivery [11] or even an increase in odds of operative or cesarean delivery and a decreased chance of spontaneous vaginal delivery with a longer second stage with delayed pushing [6,21]. A recent secondary analysis concluded that delayed pushing was associated with a longer second stage, increased odds of cesarean birth and postpartum hemorrhage but no increase in neonatal morbidity [21]. Regardless of findings that delaying pushing may be associated with longer second stage, women with prolonged labor give birth vaginally in 78-82% of cases [4].
Studies have demonstrated that delayed pushing does not negatively affect neonatal umbilical cord pH [11,22,23], Apgar score [11] or increase other neonatal adverse outcomes [11,24-27]. Others have indicated an increased rate of neonates with abnormal umbilical artery gas [12,24] and lower Apgar score at birth [25,28,29] with delayed pushing compared to immediate pushing. A large retrospective study of 42,268 women who had vaginal births reported that epidural use among nulliparous and mulitparous women led to a longer median length of second stage and the 95th percentile is longer than reported in previous studies [27]. However, the increased length of labor did not significantly increase neonatal morbidity [27].
The National Institute of Child Health and Human Development (NICHD) Consortium for Safe Labor (CSL) works to reduce the primary cesarean delivery rate and has defined second-stage arrest for nulliparous women as no progress for 3 or more hours without an epidural or 4 or more hours with an epidural. For multiparous woman, second-stage arrest is defined as no descent or rotation for 3 or more hours with an epidural or 2 or more hours without an epidural [10]. Interpreting valuable data from this consortium, ACOG and SMFM jointly released a consensus document concluding that epidurals may be associated with a longer second stage and recommended the diagnosis of arrest should not be made until at least 2 hours of pushing in multiparous and 3 hours in nulliparous women [1]. They also concluded that the ideal length of the second stage is not able to be determined and that the absolute risks of adverse fetal and neonatal outcomes after a longer duration in the second stage are low [1].
Since the consensus document in 2014, many recent studies examined second stage labor, specifically maternal and neonatal outcomes related to allowing more time in the second stage. Most importantly, in 2015 Cheng and Caughey stated that “historic, time-based thresholds for the management of second stage of labor appear to have been misguided; in modern obstetric practice with continuous fetal monitoring, greater patience in the second stage appears to be merited” [5].
The objective of this pre- and post-retrospective cohort study was to assess the birth outcomes following implementation of an evidence-based guideline for managing delayed pushing in the second stage of labor in women with epidural anesthesia.
This was a retrospective cohort study at a community hospital located in suburban Minneapolis that was part of a larger not-for-profit health care organization (HCO). This HCO launched the Zero Birth Injury (ZBI) initiative while implementing the strategies of the Premier Safety Initiative, a 19 Hospital, nationwide quality and safety initiative that began in 2008 [30,31]. From 2008-2010 the ZBI team sought to eliminate preventable birth injuries by implementing standardized guidelines for first stage labor using a multidisciplinary team approach [30,31]. The next natural step was to create a guideline for second stage of labor [30]. The rate of epidural use during the time period of this study was 87% at the community hospital. The operative vaginal delivery (all vacuum assisted) rate was 21%. The hospital where the guideline was implemented averaged 250 births per month attended by obstetricians in nearly all cases. This study was approved by the Institutional Review Board at the University of Minnesota (HCO) (Study Number 1012M93392).
The guideline was derived from an evidence-based set of parameters, identified in the literature [32-34] and modified with permission from the author [33,34] to meet the needs of both nulliparous and parous women in labor with epidural anesthesia [30] (See Figure 1). An algorithm demonstrating guideline use was created for physician and nurse education [30] (See Figure 2). All labor and delivery unit nurses completed mandatory education about the use of the standardized second stage labor guideline. A computer-based education program was developed that included a step-by-step discussion of the guideline, using a decision tree format to communicate hourly care requirements during second stage. Obstetricians received education on the associated guideline through presentations at department meetings, circulation of the guideline to all obstetricians by email, as well as some personal visits to practices’ provider meetings by one of the physician authors (CH). Additionally, laminated copies of both the guideline and algorithm were placed on the labor unit for reference. Members of the quality team and nurse educators conducted extensive outreach on the labor unit with staff nurses during all shifts to ensure that all nurses were familiar with implementation strategies [30].
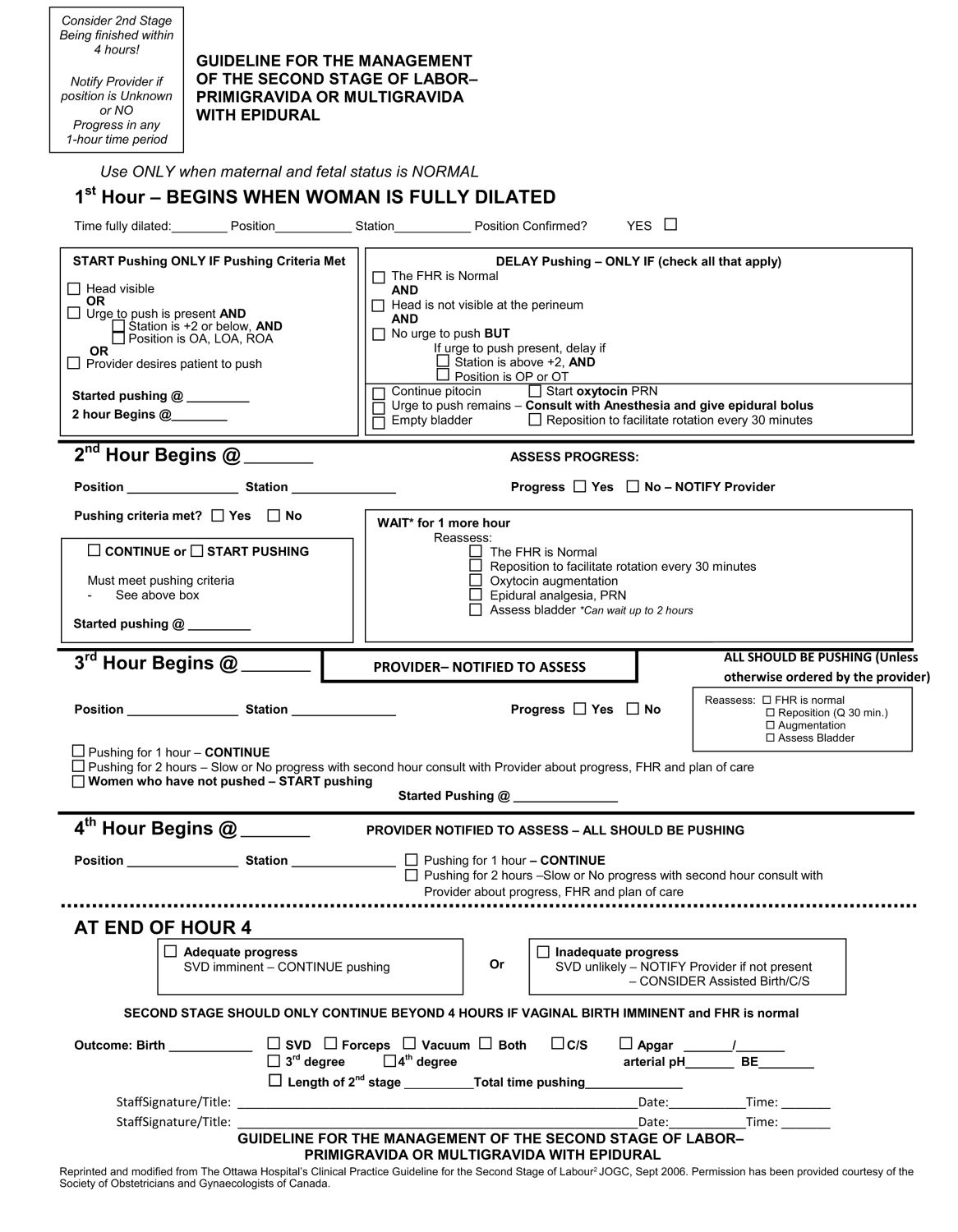
Figure 1. Guideline for the management of the second stage of labor—primigravida or multigravida with epidural use. Reprinted and modified from “The Ottawa Hospital’s Clinical Practice Guideline for the Second Stage of Labour,” originally published in the Journal of Obstetrics and Gynaecology Canada in September 2006. Used with permissions from the Journal of Obstetrics and Gynaecology Canada as well as Journal of Perinatal and Neonatal Nurses. LOA, left occitput anterior; OA, occitput anterior; OP, occiput posterior; OT, occitput transverse; PRN, pro re nata (“as needed”); Q, every; ROA, right occiput anterior; SVD, spontaneous vaginal delivery.
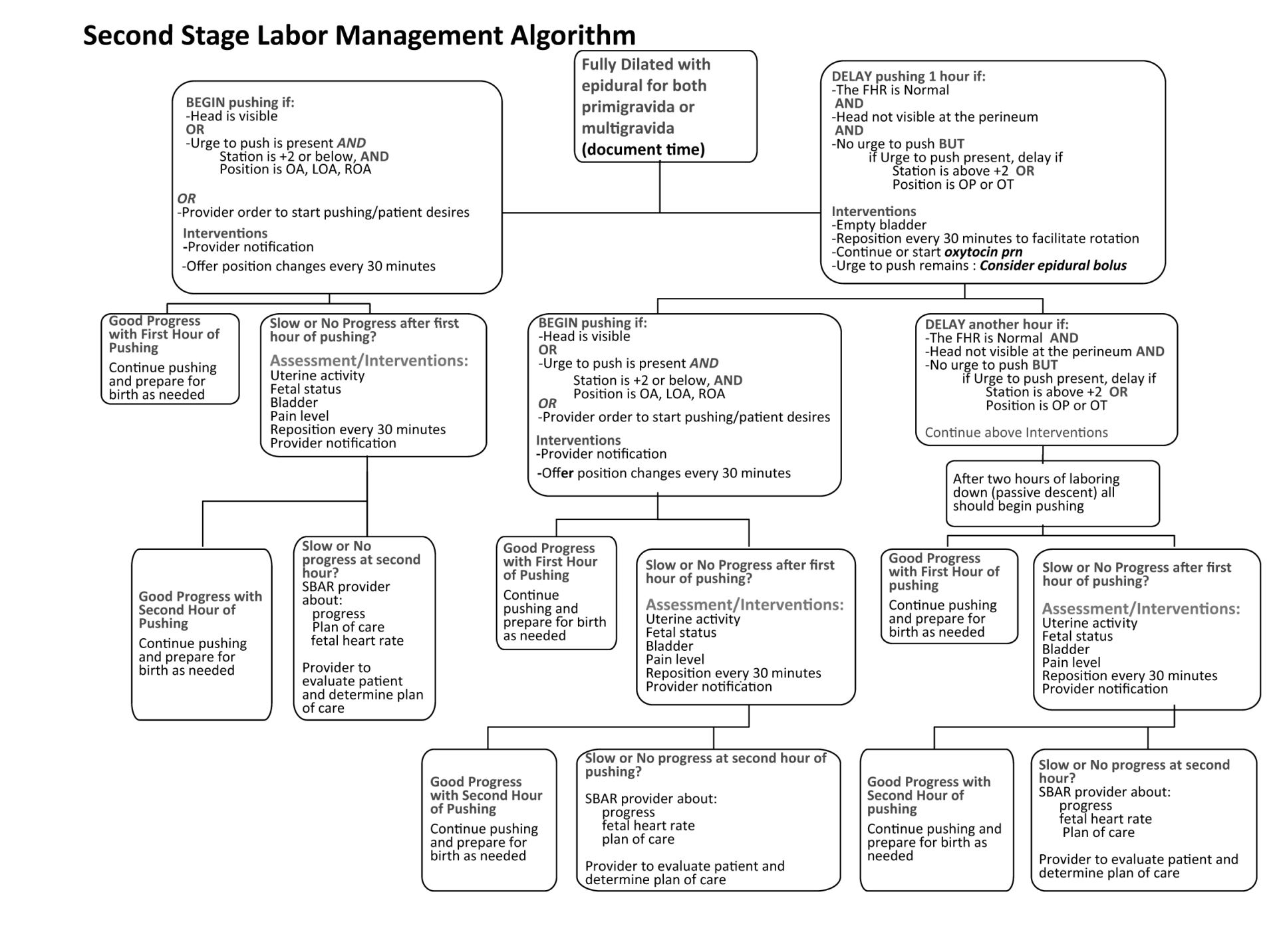
Figure 2. Second Stage Labor Management Algorithm, created for education purposes from the modification of Figure 1. Used with permissions from the Journal of Perinatal and Neonatal Nurses.
Consistent with the guideline [30], nulliparous and parous women with epidural anesthesia, a normal fetal tracing, and complete dilation without an urge to push, including those with a fetus in the occiput posterior position, were encouraged to delay pushing for up to two hours followed by active pushing. Women with an urge to push at complete dilation were encouraged to follow their instincts and begin actively pushing. The guideline [30] was implemented by the RN initiating a pre-checked order set specifying the use of the guideline if the patient met the criteria. If guideline use was not documented, lack of documentation was indicated in the medical record. The guideline was not implemented for women with multi-fetal pregnancies, those having a trial of labor after cesarean (TOLAC), those without epidural anesthesia as well as patients with an urge to push at a station of +2 or below (-3 to +3 system) and in the left occiput anterior, occiput anterior or right occiput anterior position, who began pushing without delay [30].
All data were compiled through retrospective review of health records by two study authors. The pre-guideline implementation (pre-GLI) group included records of women who gave birth during the threemonth period between January 1 and March 31, 2010. These women gave birth prior to guideline development, discussion or education, but their characteristics would have made them eligible for guideline use. The post-guideline implementation (post-GLI) group included women who gave birth between April 24 and July 24, 2011 and met criteria for guideline use.
The following maternal descriptive variables and those related to the labor management were recorded: gravidity, parity, gestational age, maternal age, oxytocin and epidural anesthesia use, and time of complete cervical dilatation. Second stage of labor variables included length of second stage from complete dilatation to birth of the newborn in minutes, duration of active maternal pushing effort in minutes, presence or absence of delayed pushing (no maternal pushing encouraged unless involuntary urge or guideline criteria met) and duration of delayed pushing in minutes, if yes. Birth outcomes from the maternal birth record were reviewed and then compared to the delivery note to verify the presence or absence of episiotomy, use of vacuum extractor and reason (maternal or fetal), 3rd or 4th degree laceration, and cesarean birth. Neonatal outcomes were recorded from the newborn birth record and included 5-minute Apgar score and birth weight in grams.
Women’s demographic and baseline characteristics were summarized and compared between the two study periods (pre- and post-GLI) using Chi-Square and Fisher’s Exact tests for categorical data and t-tests for continuous data. A woman was considered to have delayed pushing if there was any difference between pushing time and overall length of second stage.
The association between the guideline implementation (GLI) and the outcomes of vacuum assisted delivery, cesarean birth, pushing time > 30 minutes, and total length of the second stage > 30 minutes were first considered using Chi-square tests, then using multivariable logistic regression. Models were adjusted for parity, time delayed pushing, maternal age, and gestational age; interactions with GLI were considered. and any variables found to be associated with GLI or the outcome. Odds ratios and 95% confidence intervals were estimated. An interaction term between GLI and parity was also considered, and if found to be significant, odds ratios were reported separately. As a sensitivity analysis, the associations between the GLI with continuous pushing time and total length of the second stage were also considered using Wilcoxon rank sum tests.
Secondary outcomes (episiotomy, laceration, and 5-minute Apgar) were described and compared between implementation periods using Chi-Square, Fisher’s Exact tests, and t-tests. To account for the deliveries post-GLI for which the guideline use was not documented, patient characteristics and outcomes were compared between those whose guideline use was documented and those without documentation of guideline use. The proportions of outcomes by hours delayed pushing were reported and compared with chi-square tests.
Results were considered statistically significant if p-values were less than 0.05 and have not been adjusted for false discovery rate. All analyses were conducted using SAS version 9.4 (Cary, NC).
There were 832 women included in this study: 403 pre-GLI and 429 postGLI. Demographic and clinical characteristics are displayed in Table 1. Women who delivered post-GLI were slightly older (P = 0.021) and the gestational age of their infants was slightly shorter (P = 0.036). Women who delivered post-GLI were more likely to delay pushing than women who delivered pre-GLI (51% vs 6%, P < 0.0001). Among the 429 women who delivered post-GLI, 247 (58%) had documented use of the guideline in the record while 182 (42%) records did not include documentation of guideline use. Patient characteristics were not significantly different between guideline documentation groups post-GLI, although women with documented use of the guideline were more likely to delay pushing than those whose record did not include documentation of use of the guideline (78% vs 14%, P < 0.0001).
Outcomes are presented in Table 2. Women who delivered post-GLI were less than half as likely to have experienced a vacuum assist for delivery compared to women who delivered pre-GLI, even when adjusting for time delayed pushing, parity, gestational age and maternal age (aOR 0.47 [0.29, 0.75], P = 0.002). This effect was not different between nulliparous and multiparous women. In the post-GLI era, adjusted for time delayed pushing, the odds of a vacuum assisted delivery were lower among women with documented use of the guideline (aOR 0.47 [0.21, 1.05], P = 0.065), with the result approaching significance. The primary reason for births experiencing a vacuum assist in both eras was fetal heart tracing abnormalities (57% in the pre-era and 76% in the post-era). Among women who delivered with a vacuum assist for birth, pre-GLI, 41% of women experienced vacuum assist for maternal exhaustion compared with 22% post-GLI (P = 0.054).
Among nulliparous women, the odds of pushing time > 30 minutes were lower among women who delivered post-GLI compared to women who delivered pre-GLI (aOR 0.58 [0.32, 1.06]). For multiparous women, the odds of pushing time < 30 minutes was no different between GLI eras (aOR 1.18 [0.73, 1.90]). When considering a continuous pushing outcome, pushing times were notably longer for nulliparous women than for multiparous women but pushing times were significantly decreased for both parity groups post-GLI vs pre-GLI (Nulliparous: median pre-GLI 69 [41- 110] minutes vs post-GLI 58 [33-97] minutes, P = 0.01; Multiparous: median pre-GLI 20 [10-31] minutes vs post-GLI 15 [7-29] minutes, P = 0.01). However, the decrease in continuous pushing time from pre-GLI to postGLI was not significant in adjusted analyses. Post-GLI, the pushing time was significantly decreased among those whose providers documented use of the guideline compared to those whose did not (median 25 [10-60] vs 35 [17-61] minutes, P = 0.025).
Odds of overall length of the second stage > 30 minutes was similar post- and pre-GLI (aOR 0.90 [0.59-1.36], P = 0.61). Considering a continuous length of the second stage outcome, times were slightly longer post-GLI (median 47 [19-103] minutes vs 40 [20-80] minutes, P = 0.052). Post-GLI, the length of 2nd stage was statistically significantly increased among those whose providers documented use of the guideline compared to those who did not (median 55 [20-122] vs 40 [18-78] minutes, P = 0.011). Cesarean birth, episiotomies, lacerations, and low 5-minute Apgar scores did not differ significantly by GLI era or documented use of the guideline.
As displayed in Table 3, delayed pushing time was not associated with vacuum use, episiotomy, laceration, or low 5-minute Apgar score. As expected, delayed pushing was associated with a longer length of the second stage (P < 0.01). A similar trend was seen across cesarean births and longer pushing time: women who delayed pushing for less than 1 hour tended to experience improved outcomes compared to those who did not delay at all, while women who delayed pushing for more than 1 hour tended to experience similar or worse outcomes compared to those who did not delay at all. Of women who delayed pushing, delay times were generally shorter post-GLI than pre-GLI: 45% (10/22) of women who delayed pre-GLI delayed less than 1 hour (41% delayed 1 - 2 hours, 14% delayed > 2 hours) while 64% (138/217) of women who delayed pushing post-GLI delayed less than 1 hour (30% delayed 1 - 2 hours, 6% delayed > 2 hours) (P = 0.07). Those who delivered post-GLI whose providers did not document guideline use were similarly distributed among the time-delayed groups as those pre-GLI: most women did not delay pushing, and among those who did, the delays were significantly longer than for those whose provider documented use of the guideline.
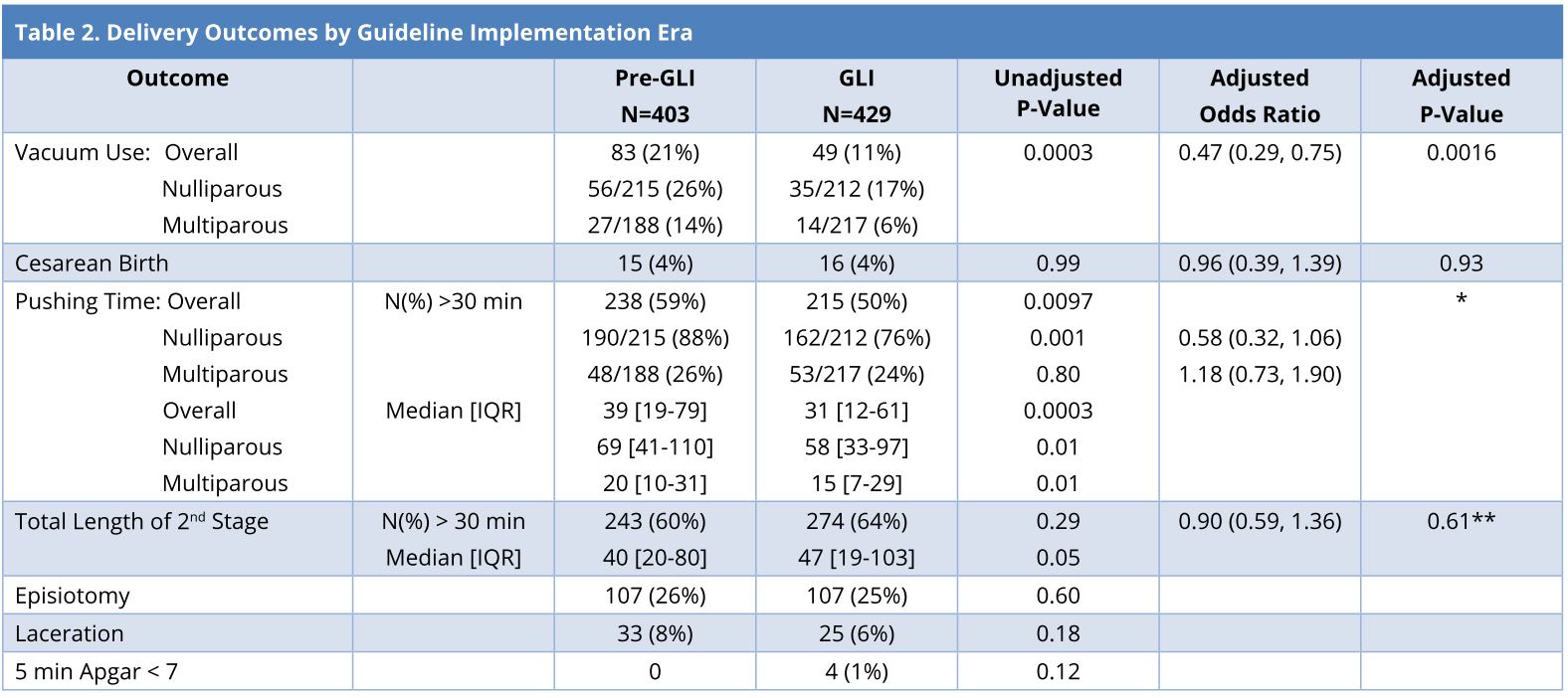
Times measured in minutes. The associations between GLI era and categorical outcomes were first considered using Chi-square tests, then using multivariable logistic regression. The associations between the GLI with continuous pushing time and total length of the second stage were also considered using Wilcoxon rank sum tests.
Covariates included in adjusted models: GLI era, parity, age, gestational age, time delayed pushing.
*The interaction between GLI and parity was found to be nearly significant and was included in the final model for pushing time > 30 minutes. Thus odds ratios are reported separately by parity.
**Due to the nature of the relationship between time delayed pushing and long length of the 2nd stage, the adjusted model for this outcome included delayed yes/no.
We studied a very specific population of women laboring in a suburban community hospital where most women chose epidural anesthesia in labor. Our intent was to assess the relationship between the implementation of a guideline for delayed pushing in second stage labor and birth outcomes among this population. All providers were obstetricians; the obstetricians and nursing staff had been trained in use of the guideline; therefore, it is likely the approach to second stage was similar whether the provider used the guideline (invoked by the order set) or not.
We found no significant difference in the median length of the second stage from pre- to post- implementation of the guideline. Although there was a significant increase in the median length of the second stage post guideline implementation among those provider who documented guideline use, the increase of 15 minutes may not be clinically meaningful. We did find a statistically significant reduction in active pushing time in nulliparous women, suggesting an advantage to appropriately selecting women to delay pushing is possibly reducing fatigue.
To assess the risks and potential benefits of delayed pushing in second stage, we used criteria to select women who would benefit the most as well as those who would not likely benefit or would be at higher risk for complications. Additionally, if the rate of operative vaginal or cesarean birth is to be determined accurately, use of specific, consistent criteria, such as a guideline is important.
“Evidence-based” and “best practice” guidelines have become commonplace, often generated or endorsed by professional medical societies or other national organizations and adopted by individual providers, group practices, hospitals and/or health care systems. The degree to which guidelines are adopted and the extent to which they have led to changes in practice patterns in hospitals and communities is not always clear [31]. While guidelines, checklists and protocols have resulted in improved maternal outcomes [35], there is a paucity of information regarding successful approaches to introducing changes in practice.
Our exploratory analyses of outcomes by time delayed pushing showed that delayed pushing for less than one hour resulted in similar or improved outcomes compared to no delay while delayed pushing for more than one hour resulted in similar or worse outcomes than no delay. Women who gave birth after the guideline was implemented, especially when guideline use was documented, were more likely to delay pushing and, of those with documented use of the guideline, the delay time was shorter. These findings support use of a guideline that assists providers in selecting women for delayed pushing and guiding when the delay should end.
Review of the literature shows considerable variation in the effect of delayed pushing on duration of the second stage, total active pushing time, and spontaneous vaginal birth [7,8,12,13,16,18,36,37]. More time allowed for descent of the fetus prior to active pushing may reduce the need for operative intervention. Some studies, including a meta-analysis, have reported no significant effect or even lower rates of spontaneous vaginal birth with delayed pushing [7,8]. Interestingly, a standard guideline for when and how delayed pushing should be employed has not been utilized in previous studies, making this a strength of our study.
Some reports show longer second stage with delayed pushing [12,36] while others show no difference [18]. In a similar fashion, some studies have reported reduced active pushing time [7,8,13] while others show no significant change or an increase in active pushing time [16,37]. The lack of a standardized method for instituting delayed pushing as well as unpredictable sample sizes affecting statistical power may account for variable results seen among published reports. Authors of a large secondary analysis of 21,034 women found that among 3,870 nulliparous women in whom pushing was delayed by an hour or more, the mean duration of second stage and active pushing time were increased compared with women with no delay or delay less than 30 minutes [21]. The authors found increased rates of cesarean delivery, operative vaginal delivery, postpartum hemorrhage and blood transfusions but no increase in adverse neonatal outcomes [21]. While this study represents the largest on delayed pushing, the authors did not account for the use of epidural anesthesia, nor specify how candidates for delayed pushing were selected, and no specific criteria or guideline was used for determining who should delay pushing. The criterion used in the analysis was a duration of 60 minutes or more as the determinant of assumed delay pushing [21]. These potential confounders may leave any benefit of properly selecting candidates for delayed pushing undetectable. A guideline such as ours would be valuable to help manage second stage labor in women who choose epidural for pain management.
Recently, ACOG Committee Opinion Number 687 [38] stated that: “In the absence of an indication for expeditious delivery, women (particularly those who are nulliparous with epidural anesthesia) may be offered a period of rest of 1-2 hours (unless the woman has an urge to bear down sooner) at the onset of the second stage of labor (page 6)” [38]. In allowing a period of rest (delayed pushing), some papers cited an increase in the duration of second stage (mean of 1 hour), less active pushing time, and a significantly increased vaginal birth rate [7,19,38]. However, when only high-quality RCT’s were included, the difference in rate of vaginal delivery with and without delayed pushing was no longer significant [7,19,38].
Our study population was women with epidural anesthesia, which has been associated with a longer second stage [21]. Data from two meta-analyses of randomized controlled trials in patients with epidural anesthesia have also shown a significant decrease in active pushing time [11,13]. In the first study parous and nulliparous women with epidural anesthesia had a significant decrease in active pushing time [11]. The same project found that delayed pushing increased the chance of a vaginal birth and decreased the risk of an instrument-assisted delivery [11]. The second meta-analysis of women with epidural anesthesia also demonstrated that women in delayed pushing groups spent less time actively pushing and had both an overall increase in spontaneous vaginal births and a decrease in instrumental deliveries [13]. Grobman and colleagues [4] reviewed 53,286 records and concluded that a majority of both nulliparous and parous women gave birth vaginally after a greater than 2 hour second stage and few infants experienced adverse outcomes [4]. These authors concluded that while longer pushing duration is statistically associated with a rise in the frequency of maternal and neonatal adverse outcomes, even when nulliparous women exceed 4 hours of pushing or parous women exceed 2 hours of pushing, they continue to have a relatively high chance of vaginal delivery and low chance of neonatal adverse outcomes [4]. Our guideline further specified that all women be assessed every 30 minutes and upon each hour of delayed pushing to assess progress and determine if both the mother and fetus should continue to delay or begin pushing.
There is no widely agreed-upon “risk-free solution” for labor management or national guidelines to help select women who might benefit the most from delayed pushing [4]. Most studies have not used a guideline for management of the second stage of labor nor controlled for potentially confounding variables. These issues may lead to erroneous conclusions regarding risks and benefits or mask effects that may exist in specific populations or circumstances.
Our study was limited by being retrospective, which always has a risk of introducing bias. We were unable to assure strict documentation of the guideline in all women for whom it was used. While the main objective of introducing the guideline was to determine whether a change in practice could be achieved, the improvement in outcomes may be weakened by the size and retrospective nature of the study. Lack of documentation of guideline use may reflect a desire by the clinician to initiate immediate pushing, a partial use of the guideline, incomplete understanding of guideline use, or incomplete documentation. Further clarification of clinician intent is recommended in future studies of guideline implementation.
In summary, there is no single risk-free solution regarding labor management or route of delivery, and maternal and neonatal risks are sometimes in conflict. Our study demonstrated that combining an evidence-based guideline with physician, nurse and administration support was successful in changing obstetrician practice and possibly improving outcomes. Most importantly, despite recent recommendations by the consensus agreement, no clear mechanisms to carry out these recommendations have emerged. This study offers a standardized guideline approach to manage the second stage supporting the recent ACOG and SMFM recommendations that aim to standardize care during the second stage of labor for women with epidural anesthesia. Our guideline-based approach may also be helpful in implementing recent recommendations by CSL, ACOG, and SMFM to allow a longer second stage among women with epidurals as a strategy to reduce cesarean births [1].
Received date: November 14, 2017
Accepted date: December 16, 2017
Published date: April 23, 2018
None
None
© 2018 The Author (s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
It is a very interesting and well written article.
A very well documented manuscript addressing a common clinical issue.
The paper is well written, and the authors have made a good effort to improve the labour outcome.
This a well-written article, and it is suitable for publication after minor revisions.