Reconstruction of the lateral plantar forefoot defect remains a challenge. With the advent of microsurgical techniques, free flaps have gained popularity in plantar forefoot reconstruction. However, the choices of recipient vessels are limited in this area. Therefore, we report two cases with lateral plantar forefoot defects using the lateral plantar artery as recipient vessel for free flap reconstruction. Flaps (medial plantar flap and peroneal artery perforator flap) survived completely. The postoperative course was uneventful and the patients were able to resume normal ambulation. The dissection of lateral plantar artery was simple and straightforward. Its vascular caliber was adequate for microvascular anastomosis. These advantages might make it a valuable option as the recipient vessel choice for lateral plantar forefoot reconstruction.
Video Abstract
Reconstruction of the plantar forefoot area remains a challenging problem due to the limited alternatives. With the advent of microsurgical techniques, free flaps become more and more popularly employed in plantar forefoot reconstruction [1-7]. Although the choice of an optimal flap is very important, the selection of appropriate recipient vessels is also equally crucial. Failure to identify appropriate recipient vessels may result in size discrepancy, unnecessary use of vein graft, and eventually flap loss. The lateral plantar artery, one of the dominant vessels contributing plantar foot circulation, is rarely reported to be used as recipient vessel for free flap reconstruction. Here, we report two cases with lateral plantar forefoot defects where the lateral plantar artery was used as recipient vessel for free flap reconstruction. The case reports describe the relevant surgical anatomy and discuss the role in the plantar forefoot reconstruction.
Anatomy and landmark of lateral plantar artery
The lateral plantar artery originating from the posterior tibial artery runs in the posterior compartment of the tarsal tunnel and continues obliquely under the tarsus in the direction to the base of the fifth metatarsal bone. It travels downward obliquely between the flexor digitorum brevis muscle and the quadratus plantae after bifurcation with medial plantar artery in the second plantar layer. It then proceeds superficially between the flexor digitorum brevis and the abductor digiti minimi muscle under the plantar aponeurosis. At approximately 1.2 cm distal to the tuberosity of the fifth metatarsal bone, the lateral plantar artery divides into superficial (the little toe fibular artery) and deep (deep plantar arch) branches [8]. To locate the direction of the lateral plantar artery, a reference line is drawn from the base of the fifth toe base to the heel. The middle third of the line indicates the part of the lateral plantar artery that potentially can be used as recipient vessel (Figure 1).
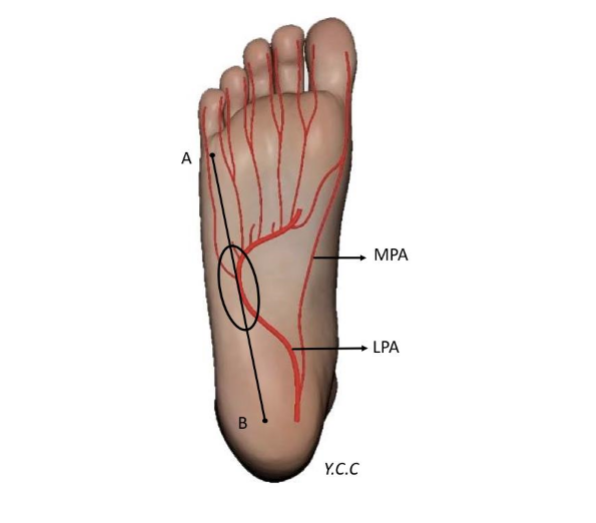
Figure 1. A reference line is drawn from point A (base of fifth toe) to point B (heel). The middle third of the reference line (circle) represents the portion of lateral plantar artery that could be used as recipient vessel. MPA, medial plantar artery; LPA, lateral plantar artery.
A 60-year-old female patient was presented due to malignant melanoma measuring 2.0 cm × 1.2 cm on her right lateral plantar forefoot. Wide excision with sentinel lymph node dissection was scheduled (Figure 2A). Wide excision of the tumor with 2 cm safety margin was done with clear margin proven by frozen section. A 5 cm × 5 cm full-thickness defect was created and medial plantar flap was designed according to the defect size on the same foot. The flap was elevated in conventional manner (Figure 2B). The location of lateral plantar artery was confirmed cial branch of lateral plantar artery was dissected out along with one concomitant vein. The diameters of the artery and the vein were 1.8 mm and 2.2 mm respectively. The fifth toe circulation was tested before ligation of the artery. The medial plantar flap was then divided and transferred to reconstruct the defect. The medial plantar artery was anastomosed to the superficial branch of lateral plantar artery (Figure 2C). The deep branch of lateral plantar artery was preserved. Venous outflow was ensured by repairing one concomitant vein. The instep donor site was covered with thin full-thickness skin graft. The viability of flap was good without complications in the postoperative course. The patient was able to achieve full-weight bearing on right foot, 2 months after the surgery. The contour of the flap was excellent (Figure 2D).
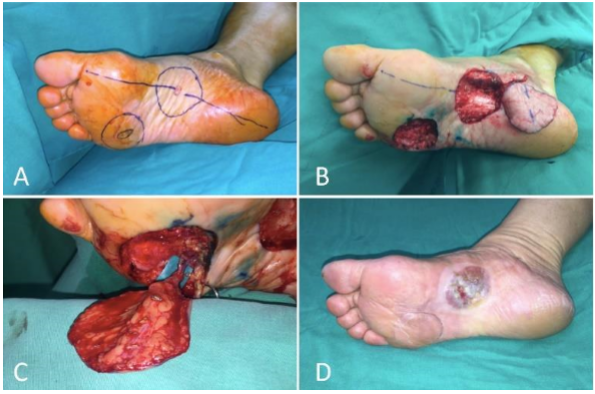
Figure 2. (A) Malignant melanoma over right lateral plantar forefoot and design of the ipsilateral medial plantar flap. (B) After wide excision, a 5x5 cm soft tissue defect was left. The medial plantar flap was elevated. (C) The pedicle of medial plantar flap was anastomosed to the superficial branch of lateral plantar artery and one concomitant vein. (D) The flap healed well with satisfactory contour in 3 months after the surgery.
A 57-year-old female patient suffered from crushing injury on the right foot during a traffic accident and resulted in a full-thickness soft tissue defect measuring 18.0 cm in length and 5.0 cm in width (Figure 3A). An 18 cm × 6 cm peroneal artery perforator (PAP) flap was designed on the ipsilateral lateral leg (Figure 3B). The flap dissection technique was the same as described in our previous publication [4]. The location of lateral plantar artery was checked by hand-held Doppler probe. After dividing the plantar fascia and separating the junction between the flexor digitorum brevis muscle and the abductor digiti minimi, the lateral plantar artery along with one accompanying vein was dissected out. The diameters of the artery and the vein were 2.2 mm and 3.0 mm respectively. The artery was temporarily clamped to ensure the distal foot circulation. The flap was then transferred and microvascular anastomosis was performed (Figure 3C). The flap perfusion was satisfactory at the time of finishing the anastomosis (Figure 3D). The postoperative course was uneventful. Partial weight bearing was allowed one month after the surgery. Patient was able to achieve full weight bearing and normal ambulation 3 months later without difficulty in wearing the shoe.
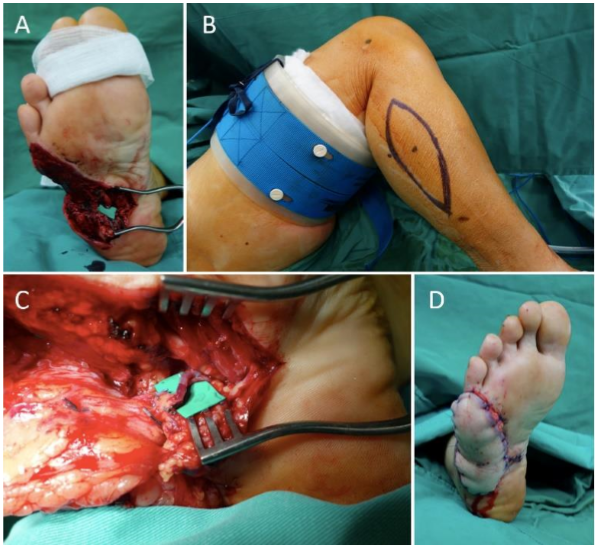
Figure 3. (A) A traumatic soft tissue defect from lateral plantar forefoot extending to middle plantar foot. The lateral plantar artery was dissected and prepared as recipient vessel. (B) A proximal peroneal artery perforator flap was designed on the ipsilateral lateral leg. (C) The flap was transferred to reconstruct the defect. Microvascular anastomosis was performed to the lateral plantar artery and one concomitant vein. (D) The immediate appearance after flap reconstruction.
The ideal coverage to plantar forefoot is to use durable soft tissue with minimal bulkiness and follow the principle of “replace like tissue with like” [1]. Therefore, glabrous plantar skin from the spare part of foot is the first choice. Several local flap options have been described to reconstruct the plantar forefoot defect, including V-Y plantar flap [9], plantar marginal septum cutaneous island flap [10], island lateral plantar artery perforator flap [11], and distally based or reverse medial plantar flap [3,12,13]. In particular, the conventional flap design of the medial plantar flap has often limited mobilization, but if based on its retrograde flow, the arch of movement of the flap can greatly improve. However, venous congestion is a concern, requiring supercharging or delay procedure [14,15]. The local flap option is summarized in table 1. When the defect is large (>100 cm2) or the foot is severely traumatized, a reconstruction with free flaps is indicated [16]. Although the best flap type has not yet been determined, the instep flap, due to its similar viscoelasticity to the plantar forefoot skin, is undoubtedly the first choice [2,5,16,17] Thin perforator flap (< 6 mm in thickness), composed of small fat lobules invested by dense fibrous septa allowing less gliding, is another optimal choice [4,7]. Furthermore, sensate coverage is available by including branch of medial plantar nerve with the medial plantar flap, which is crucial for plantar defect reconstruction. In the case 1, although the defect was a candidate for a reverse medial plantar flap, we were concerned about the uncertainty of the venous drainage and felt safer to perform free flap reconstruction. In the case 2, the defect was 18 cm in length, which exceeded the conventional design of medial plantar flap [5]. The peroneal artery perforator (PAP) flap provided a thin and pliable skin [4]. Based on our previous experience, using it in the distal hand and foot reconstruction, we successfully transferred the PAP flap for resurfacing of the plantar forefoot defect.
Other than the flap type, the recipient vessels are of paramount importance. The dorsal metatarsal artery, dorsalis pedis artery, medial plantar artery, and posterior tibial artery have been well reported as recipient vessels in the literature [1-3,6,18]. Particularly, the dorsal metatarsal artery and the dorsalis pedis artery are suitable recipient vessels for dorsal foot and transmetatarsal foot defects; but not for pure plantar forefoot defect. The use of the medial plantar artery or posterior tibial artery is more convenient in this situation. Zelken et al. reported the use of innervated medial plantar flaps for forefoot reconstruction and mentioned that if ipsilateral medial plantar flap was employed, it required the interposition of a vein graft in order to reach the ipsilateral medial plantar artery or posterior tibial artery [18]. Size discrepancy was encountered between donor vein graft and recipient artery, which increased the chance of thrombosis. For defects mainly located in the lateral part of plantar forefoot, as in our two cases, the recipient vessels, the just above mentioned, are too far away to reach. Although it is possible to use the plantar metatarsal artery, the diameter is usually small and requires super-microsurgical technique; moreover, the presence of accompanying vein is unpredictable [19]. The recipient vessel choice for plantar forefoot reconstruction is summarized in table 2. The lateral plantar artery is rarely reported as recipient vessel due to its deep location. However, in the middle third of the reference line we have proposed, the lateral plantar artery runs superficially between the flexor digitorum brevis and abductor digiti minimi [8]. It can be easily exposed by incision through the plantar aponeurosis and separation of the muscles, the vascular diameter is closed to the flap pedicle size.
Division of the lateral plantar artery does not jeopardize the foot circulation because of anastomosis of the lateral plantar artery with the dorsalis pedis artery at the first intermetatarsal space. However, care should be taken with patients with peripheral artery occlusive disease and the flow of dorsalis pedis artery should be confirmed before surgery. Given the advantages of sizable vessel, easy dissection, and proximity to the defect, we believe that the lateral plantar artery might be a valuable option as recipient vessel for lateral plantar forefoot reconstruction.
Received date: April 30, 2017
Accepted date: September 28, 2017
Published date: October 03, 2017
© 2017 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). SciTeMed
Video Abstract
Interesting technique and a very timely paper! We are at a time when microsurgeons are migrating from the convention of using major vessels such as dorsals pedis/posterior tibial arteries as recipients for lower extremity reconstruction to more delicate approaches of using perforators or branches of named vessels as recipients. Doing so allow us to decrease the morbidities associated with microsurgical reconstruction. Foot is traditionally a site with few recipient options. The authors had demonstrated feasibility of using lateral plantar artery as recipient vessel, and the cases demonstrated were elegantly done. I would, however, recommend that the authors include a comparison/contrast of the proposed technique with more conventional technique, especially when the proposed technique is more technically complex. For example, how is the proposed technique compared to reverse medial plantar artery flap? The authors had mentioned that the reverse medial plantar artery flap might require supercharging for venous congestion, but doing so would still be technically more straightforward than performing it as a free flap. In other words, how does the proposed technique compare with the conventional techniques in terms of time spent, quality of reconstruction, functional outcome, aesthetics, and the surgeon effort? Adding such an analysis would make the paper more complete and also allowing surgeons to more thoroughly consider the various reconstructive options.
ResponseThanks for your precious comments. We agree that it is very important to compare the proposed technique with the conventional technique and let the readers know the difference in terms of the time spent, quality of reconstruction, functional outcome, etc. However, this manuscript is a case report and we aim to propose the use of lateral plantar artery as recipient vessel by using different flap (medial plantar flap and peroneal artery perforator flap). The point is to focus on the recipient vessel choice, but not on the flap type. So, it is difficult to compare the function result of the reconstruction. In addition, we don’t have enough case numbers to make comparison with the other conventional techniques. So, the best we can do is to summarize the advantages and disadvantages of the proposed technique and conventional technique based on the literature. The comparison is summarized in table 1 and table 2.
The authors present two cases of lateral plantar defects that were treated with free flap reconstruction using the lateral plantar artery as recipient vessels. The manuscript is well written and the anatomy is thoroughly described in detail. Therefore, in my opinion, the manuscript is very suitable for publication and of great interest to the journals readership. The only remark I would like to make is the importance of the sensibility of any reconstruction in this area, which whenever possible is very important to reconstruct.
ResponseWe appreciate the reviewer’s comments. Indeed, the sensibility of this area is very important. If you use the medial plantar flap, it is possible to include nerve as a sensate flap. We have included this comment in the revised manuscript page 10, line 1-2. Thank you.
The revised article can be accepted for publication.
The article is accepted, please go ahead and publish it.
Chen YC, Scaglioni MF. The lateral plantar artery as recipient vessel for microsurgical lateral plantar forefoot reconstruction: Case report. Int Microsurg J 2017;1(2):2. doi:10.24983/scitemed.imj.2017.00036