Clival lesions are diverse and can be classified into primary, originating from notochordal or hematologic derivatives, or secondary tumors arising from the pituitary gland. Clival metastases are rare. The aim of imaging clival lesions is to delineate the disease's epicenter. However, it may not consistently differentiate between diagnoses in locally invasive lesions. We describe a challenging case involving a 51-year-old Chinese female who presented with atypical symptoms of headache and nasal pain. Initial computed tomography and magnetic resonance imaging findings revealed an invasive lesion of the clivus, supporting a diagnosis of either chordoma or chondrosarcoma. A definitive diagnosis was obtained through a transsphenoidal biopsy, which identified the lesion as a pituitary neuroendocrine tumor. The lesion was subsequently completely excised without postoperative complications. This case underscores the necessity of mandatory biopsy for invasive clival lesions, especially those presenting with atypical imaging features, rather than solely relying on imaging for diagnosis. In the era of minimally invasive transnasal endoscopic techniques, these diagnostic approaches routinely achieve a high diagnostic yield and must be considered to guide further treatment and prognosis.
A locally invasive clival lesion may arise from notochord-derived tumors (such as chordoma, chondromas, chondrosarcomas) and hematologic malignant tumors (myeloma, lymphoma, Langerhans cell histiocytosis), which are centered within the clivus. Less commonly, invasive pituitary adenomas may secondarily involve the clival region, typically occurring in older adults [1]. Rarely, clival metastases from head, neck, abdominal, and thoracic malignancies may be considered. Conventionally, a lesion is deemed to arise from the pituitary gland if the normal pituitary gland is not seen separately. In cases with atypical radiologic features, a biopsy is mandatory to establish a definitive treatment plan and to counsel patients regarding the prognosis, the morbidity of planned surgery in a high-risk skull base region, and the potential need for adjuvant treatment. Advances in trans-sphenoidal endoscopic biopsy techniques may facilitate a minimally invasive diagnostic approach; however, exact histologic diagnosis may be challenging due to the overlap in tumor morphology [2].
In the article, we report a challenging case of an invasive clival lesion, emphasizing the diagnostic complexities encountered due to its potential origins from various sources such as notochord-derived tumors, hematologic malignancies, and less frequently, invasive pituitary adenomas or metastases. The precise identification of the lesion's nature is crucial for determining the appropriate treatment pathway and for patient counseling regarding prognosis and surgical considerations. This case highlights the critical role of biopsy, especially with atypical radiological features, and showcases how recent advancements in minimally invasive biopsy techniques are pivotal in achieving an accurate histological diagnosis, despite the inherent morphological similarities among different tumor types.
A 51-year-old Chinese female with a history of hypertension, hyperlipidemia, and type 2 diabetes mellitus presented to the accident and emergency department complaining of left nasal pain, which radiated to her left periorbital and temporal regions over the course of one month. Upon further questioning, she reported intermittent episodes of pain that had gradually worsened over two years, accompanied by vomiting. This condition had been managed by her primary care physician as a migraine, with symptomatic medications prescribed. She exhibited no focal neurologic symptoms. However, the patient sought emergent medical attention due to the persistently worsening pain symptoms. A computed tomography scan of the brain, conducted in view of the worsening headaches and vomiting, revealed a midline clival mass extending into the bilateral sphenoid sinuses. The mass was locally invasive, eroding the sphenoid septum and pituitary fossa (Figure 1). There was no noted extension into the intracranial or cavernous sinus areas. She was referred urgently to our department for further evaluation.
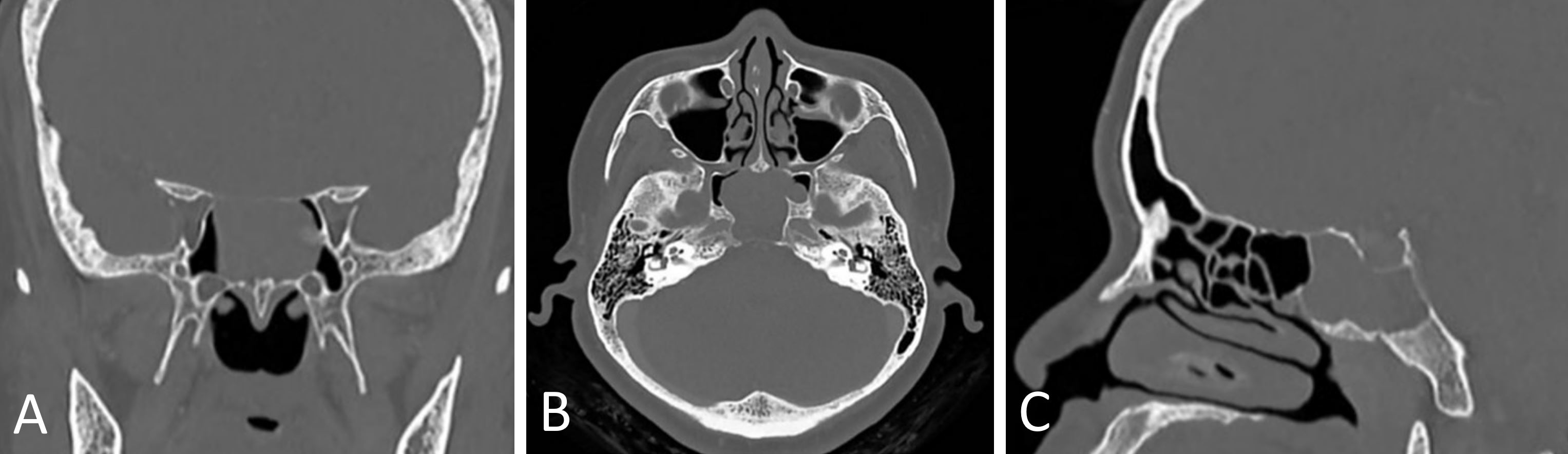
Figure 1. Computed tomography imaging of a locally invasive lesion at the clivus. (A) Coronal Section. (B) Axial Section. (C) Sagittal Section.
Head and neck examination, including flexible nasoendoscopy, was unremarkable. No tumor was visible within the nasal cavity proper or at the sphenoid ostia, even after meticulous decongestion. Neurological examination yielded normal results. Further workup was conducted with magnetic resonance imaging of the brain and paranasal sinuses.
The magnetic resonance imaging conducted to more precisely delineate the lesion revealed a large clival mass measuring 3.2 cm x 2.9 cm x 3.1 cm. The mass was observed displacing the pituitary gland superiorly and partially encasing the bilateral cavernous segments of the internal carotid arteries (Figure 2). The primary radiologic differentials considered were chordoma or chondrosarcoma.
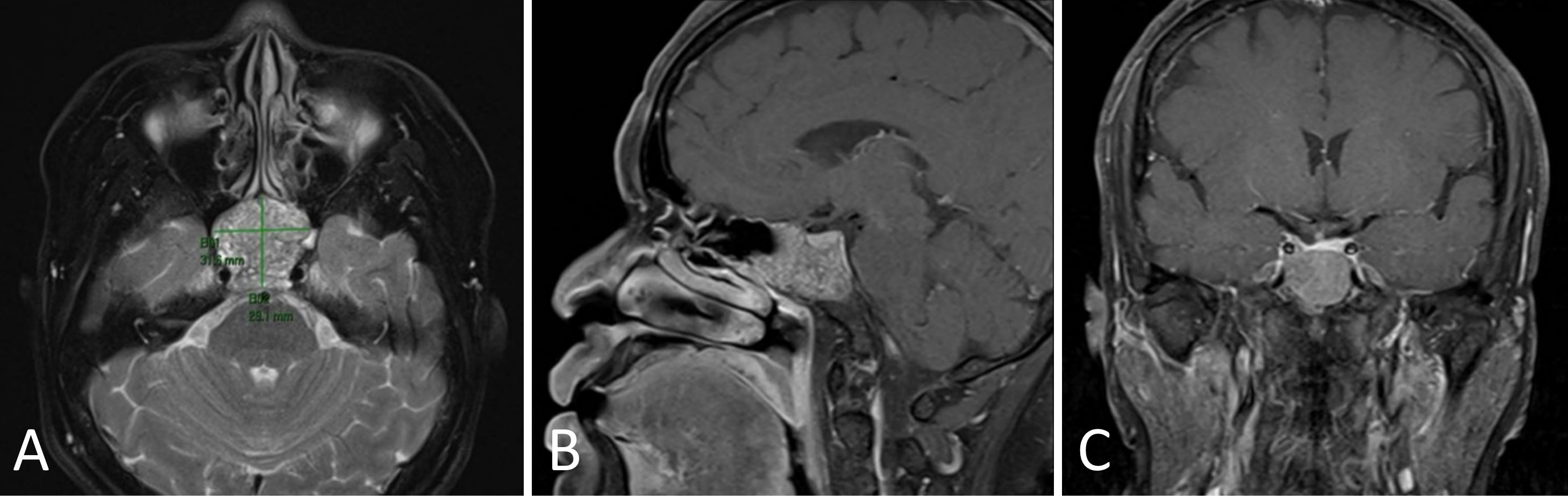
Figure 2. Magnetic resonance imaging depiction of the clival lesion, illustrating its proximity to the pituitary gland, sphenoid bone, and cavernous sinuses. (A) Coronal Section. (B) Axial Section. (C) Sagittal Section.
The patient was counseled for an endoscopic endonasal biopsy of the lesion. While an image-guided transcranial biopsy was considered, an endoscopic approach was eventually favored. This decision was made with the aim of optimizing lesion visualization, maximizing diagnostic yield, and facilitating ease of hemostasis, should torrential bleeding be encountered during the biopsy.
An endoscopic, transnasal, trans-sphenoidal biopsy of the clival lesion was performed. Intraoperatively, the tumor appeared smooth and well encapsulated, abutting bilateral sphenoid ostia yet separate from the anterior sphenoid wall. The biopsy identified the tumor as a pituitary neuroendocrine tumor (corticotroph subtype). Immunohistochemical staining demonstrated diffuse positivity for synaptophysin, chromogranin, and CD56, along with diffuse cytoplasmic-membranous positivity for CAM5.2 and cytokeratin AE1/AE3. The Ki-67 proliferation index was 2-3%. Further testing with a pituitary hormone panel assay returned normal results. Subsequently, the patient consented to and underwent an endonasal resection of her pituitary tumor, with a neurosurgeon involved in the procedure.
During this definitive surgery, surgical access was further optimized by performing a posterior septectomy and further widening the sphenoid ostia. A large, bulky tumor occupying the entire sphenoid sinus was encountered. Anteriorly, a clear plane was maintained between the lesion and the sphenoid sinus walls. Superiorly, the lesion had invaded the clivus and bony sellar walls. The tumor was decompressed prior to its complete endoscopic dissection. Post-resection, small segments of bony erosion were observed over the right internal carotid artery, but bilateral clival segments of the internal carotid artery were visualized and found to be intact. A small section of clival dura was exposed, yet no cerebrospinal fluid leak was encountered. The patient recovered well postoperatively, and the final histology identified the presence of an ACTH-positive adenoma, with a low Ki-67 index of up to 5% in focal areas.
The patient was well at the time of recording this case report, 6 months after surgery, with no features of disease recurrence on surveillance nasoendoscopy and imaging (Figure 3).
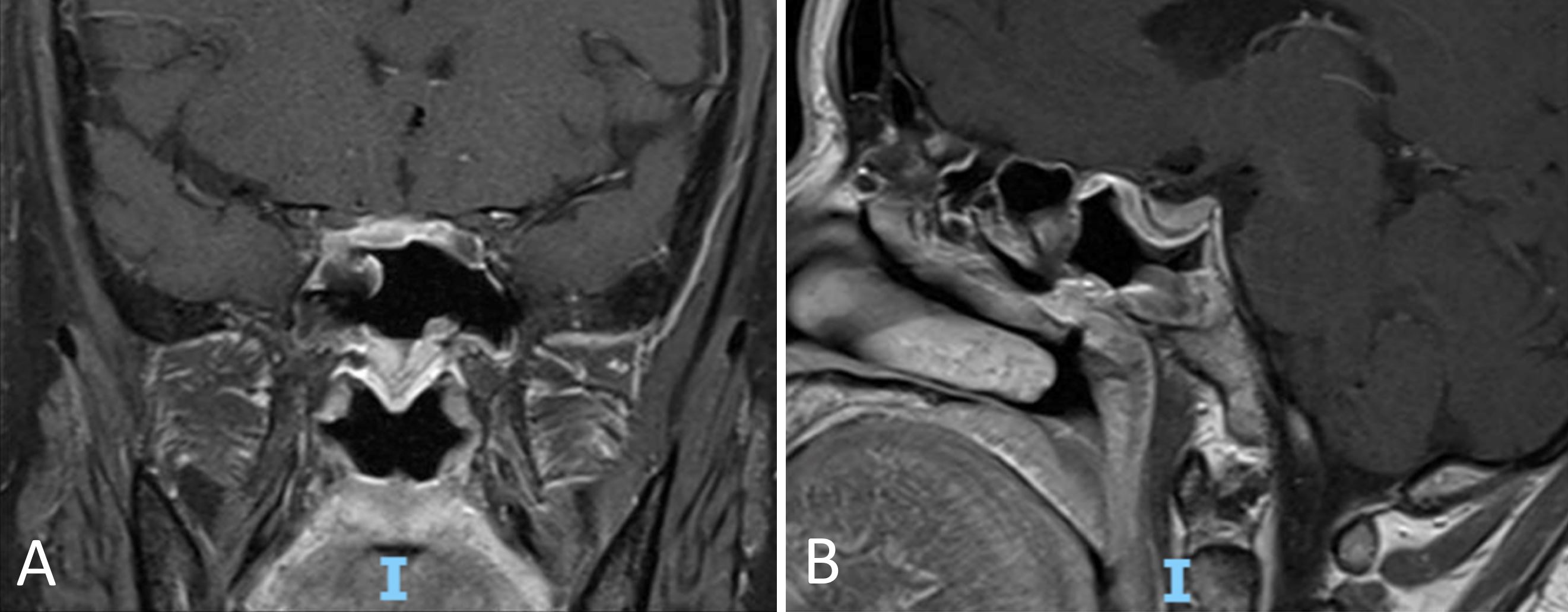
Figure 3. Post-operative magnetic resonance imaging confirms complete resection of the pituitary neuroendocrine tumor, with no evidence of recurrent neoplasm. (A) Coronal Section. (B) Sagittal Section.
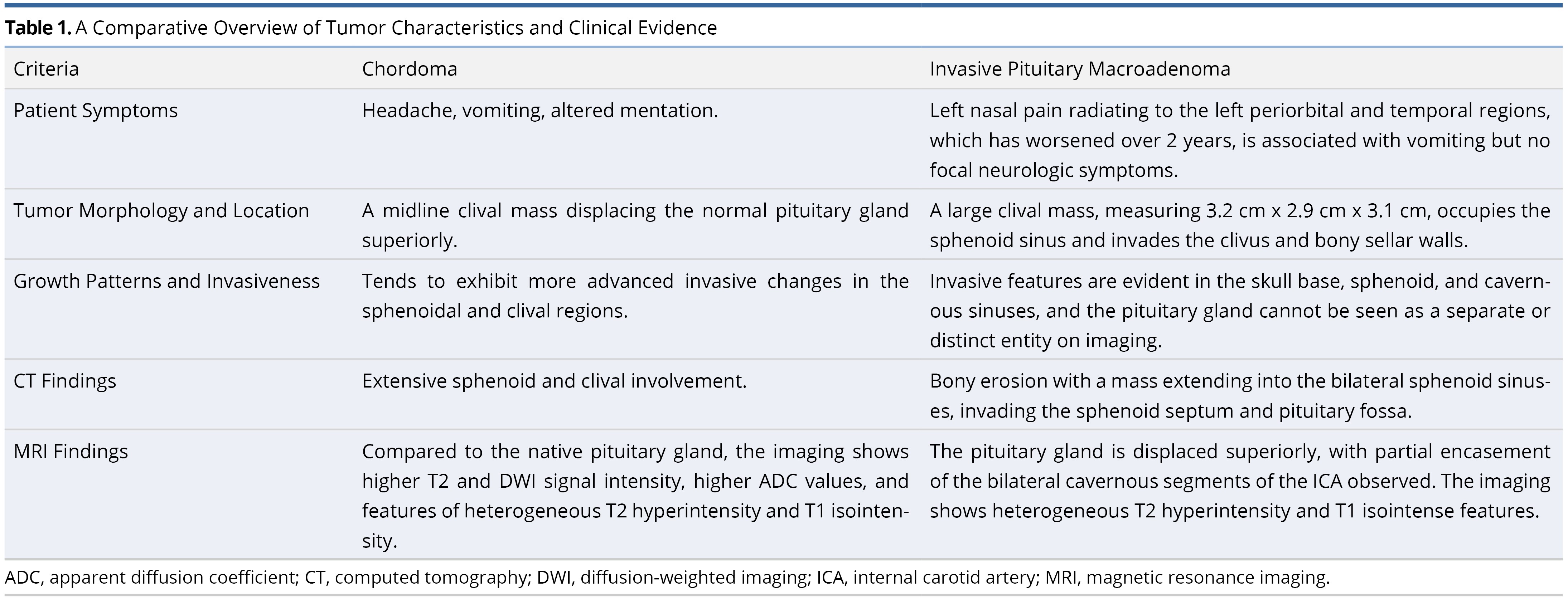
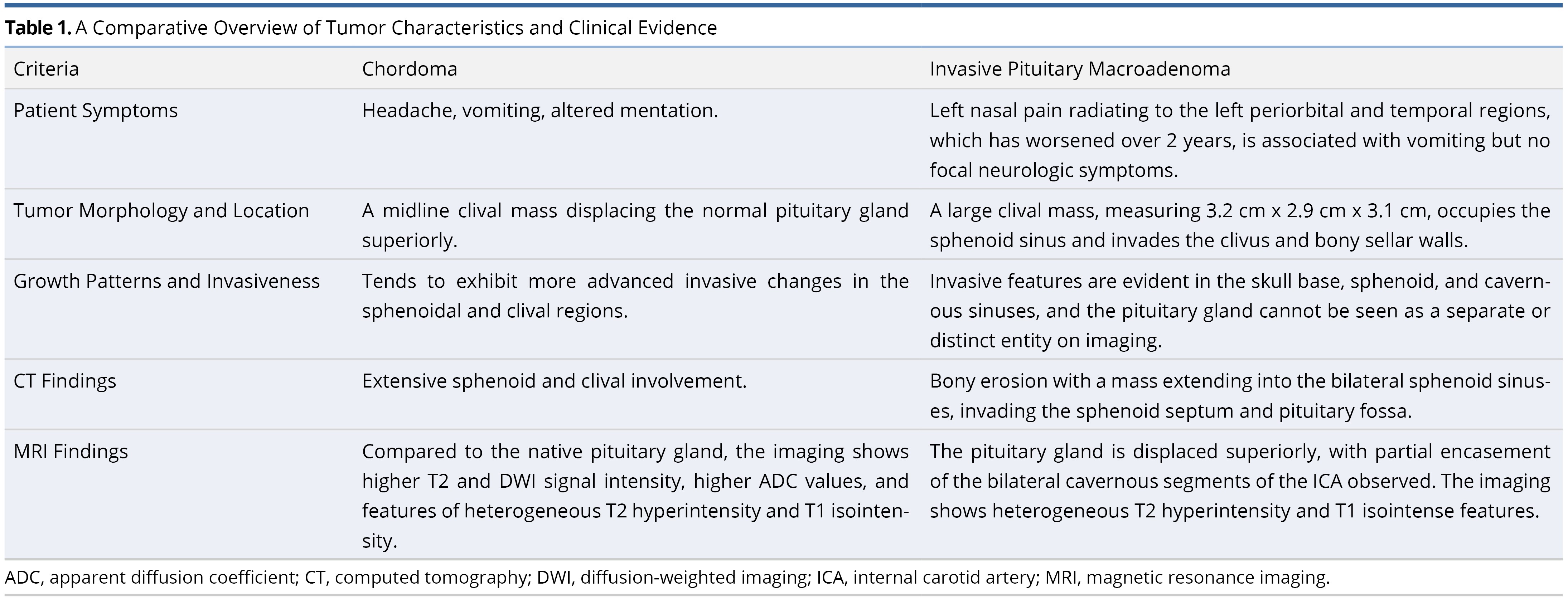
This case report details our management of a complex pituitary tumor, providing an in-depth examination of the strategies employed for the accurate diagnosis and treatment of a problematic clival lesion. It particularly emphasizes the challenge of differentiating between chordoma and invasive pituitary macroadenoma, a task made difficult by the presence of overlapping and vague characteristics that significantly obstructed our path to a conclusive diagnosis. The clinical and imaging diagnostic challenges encountered during this process are concisely summarized in Table 1.
Tumor Size and Invasiveness
Pituitary neuroendocrine tumors (PitNETs) represent a more precise terminology for lesions previously classified as pituitary adenomas. These PitNETs can be further classified into various lineages and morphofunctional subtypes [3]. The distinction between microadenomas and macroadenomas, beyond the criterion of tumor size greater than 1 cm, can also be based on radiologic evidence of local invasion. In our patient, both the size (the tumor measured 3.2 cm) and the presence of invasive features were indicative of an invasive macroadenoma. Such macroadenomas may invade the skull base or sphenoid and cavernous sinuses, rendering the pituitary gland indistinct or not separately visible on imaging.
Patient Symptoms
This case posed several diagnostic challenges. Primarily, the clinical symptoms of nasal pain and headaches, rather than the visual disturbances or other ocular symptoms more commonly associated with pituitary macroadenomas, suggested a non-pituitary origin. Rutkowski and colleagues, in their review of symptoms presented by patients with atypical pituitary macroadenomas, found that headaches and visual changes were reported by up to 42% of patients [4]. This indicates that symptoms related to the mass effect of pituitary lesions are relatively consistent, even in atypical cases. Consequently, clinicians are inclined to rely more heavily on imaging for further diagnostic clarification.
Imaging Diagnosis Distinctions
Additionally, diagnostic imaging presented its own set of challenges. It was critical to ascertain whether the lesion originated from the clivus or the pituitary gland. The tumor's size (3.2 cm) and the locally invasive characteristics, such as bony erosion observed on computed tomography scans, led to the consideration of a pituitary macroadenoma as a differential diagnosis. Imaging features that suggested a chordoma included extensive involvement of the sphenoid and clivus, alongside the displacement of a normal-appearing pituitary gland superiorly. Conversely, an invasive pituitary macroadenoma would likely exhibit more pronounced invasive changes in the sellar region before extending into the clivus. Regarding patterns of extrasellar extension, research indicates that growth hormone-related macroadenomas often show infrasellar extension, while non-functional macroadenomas typically extend into the suprasellar region [5]. An ectopic clival pituitary adenoma could also be considered in the differential diagnosis, although such lesions are exceedingly rare. Given the non-definitive nature of the imaging diagnosis, the emphasis shifts towards securing an accurate tissue diagnosis, essential for devising a treatment plan.
Moreover, the consideration of various methods for tissue diagnosis presented its own set of challenges. While an image-guided biopsy would obviate the need for general anesthesia, an endonasal approach offered several advantages, including superior visualization, diagnostic yield, and ease of hemorrhage control. Given that the tumor bulk was centered in the sphenoid sinuses, a standard sphenoidotomy approach would allow the surgeon to safely visualize the mass and proceed with the biopsy. A transcranial biopsy would require navigating through multiple intervening critical structures, posing a greater risk. It is crucial for such a biopsy to be undertaken in institutions equipped with specialized personnel and facilities, to ensure the highest accuracy of diagnosis while minimizing risks to patient safety.
Magnetic resonance imaging can be instrumental in distinguishing between chordoma and invasive pituitary macroadenoma. Chordomas exhibit higher signal intensity on T2-weighted images and diffusion-weighted imaging, along with higher apparent diffusion coefficient values compared to invasive macroadenomas, attributable to their distinct histopathological features [6]. These features include an abundant myxoid stroma and large cytoplasmic components within each cell. On magnetic resonance imaging, ectopic pituitary adenomas within the sphenoidal sinus typically appear isointense relative to the adjacent grey matter and exhibit mild to moderate enhancement following contrast administration. They are generally heterogeneous, characterized by areas of low signal intensity on T1-weighted images and high signal intensity on T2-weighted images [7].
In our case, the lesion exhibited heterogeneous T2 hyperintensity and T1 isointense characteristics. In contrast, the native pituitary gland displayed T1 hyperintensity and contrast enhancement, making the lesion appear incongruous and suggesting it was of non-pituitary origin. This distinct appearance of the sellar pituitary component reinforced the working diagnosis of a non-pituitary lesion.
While clival chordomas are the most commonly encountered midline clival lesions, invasive clival lesions presenting with atypical radiologic features necessitate a confirmatory biopsy for histologic diagnosis. This is crucial for accurately counseling patients about their treatment options. The use of image-guided endonasal trans-sphenoidal techniques offers a high diagnostic yield while minimizing surgical morbidity, thereby informing further treatment strategies. Furthermore, ongoing research efforts aim to refine the diagnostic accuracy of traditional imaging techniques. This involves defining precise apparent diffusion coefficient value thresholds [8] for diagnosing clival chordomas, and assessing the efficacy of advanced imaging modalities, such as positron emission tomography-computed tomography, in accurately determining the epicenter of the disease [9].
Nevertheless, such methodologies ought to complement, rather than replace, histological diagnoses. It is imperative to conduct further research to identify any distinctive imaging traits of PitNETs across different lineages. This, coupled with hormonal analysis, could pave the way for the development of a more sophisticated and accurate diagnostic protocol.
Study Limitations
This case study, focused on the management of a complex clival lesion, encounters several notable limitations. Firstly, its reliance on a single patient's experience restricts the ability to extrapolate findings to a broader patient demographic. Additionally, due to its confinement to a single healthcare center, the outcomes and observations may not fully encapsulate the diverse clinical settings and practices prevalent beyond the confines of this institution. Furthermore, the six-month follow-up period, though informative, may not encompass the entirety of potential complications and unfavorable outcomes. It is imperative to acknowledge the rare nature of clival lesions, which can introduce a bias towards reporting positive outcomes in case studies. Nonetheless, it is worth noting that this case study makes a meaningful contribution to the existing medical literature, shedding light on the intricacies surrounding the invasiveness of PitNETs. This area of research has historically received limited attention and remains shrouded in controversy. As we accumulate additional published cases akin to the one presented herein, it is poised to significantly enhance our comprehension of this subject matter and enable more refined statistical analyses.
This case emphasizes the vital need for mandatory biopsies when dealing with invasive clival lesions, especially those with unusual imaging characteristics. Relying solely on imaging for diagnosis can fall short in these complex scenarios. In today's age of minimally invasive transnasal endoscopic techniques, these diagnostic methods consistently provide highly accurate results. They play a pivotal role in guiding treatment decisions and offering valuable insights into a patient's prognosis. These advancements in diagnostics are improving the way we manage clival lesions, ultimately leading to more effective and patient-centric care in this intricate medical field.
Received date: November 20, 2023
Accepted date: January 29, 2024
Published date: February 14, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
The article stands out by providing a comprehensive analysis of a rare case of a midline branchial cleft cyst, a significant contribution given that only three other cases have been documented in medical literature. This scarcity underscores the article's value, making it a crucial read for medical professionals. It not only highlights the diagnostic challenges and treatment strategies for such atypical presentations but also enriches the understanding of branchial cleft cysts beyond the common lateral neck occurrences. By including a detailed review and comparative analysis of these few reported cases, the article offers unique insights into the demographic, symptomatic, and anatomical variations of branchial cleft cysts. This focused analysis makes the article an indispensable resource for clinicians, surgeons, and students in the medical field, aiming to enhance diagnostic accuracy, inform clinical practice, and ultimately improve patient outcomes in dealing with complex and rare presentations of congenital anomalies.
This article offers valuable insights into the intricacies associated with diagnosing and managing clival lesions, with a particular focus on those involving the pituitary gland. The thorough examination of the presented case and the emphasis on histological diagnosis are noteworthy aspects of this work. The case under consideration significantly contributes to the extant medical literature on the invasiveness of pituitary neuroendocrine tumors, a subject that has not received extensive research attention and remains marked by several areas of controversy. The accumulation of additional published cases like the one presented here will undoubtedly advance the overall comprehension of this subject matter and facilitate more precise statistical analyses. Nevertheless, there exist certain areas within the article where further exploration and clarification could augment its impact.
|
Table 1. A Comparative Overview of Tumor Characteristics and Clinical Evidence |
||
|
Criteria |
Chordoma |
Invasive Pituitary Macroadenoma |
|
Patient's Symptoms |
Not applicable |
Left nasal pain radiating to left periorbital and temporal regions, worsening over 2 years, associated with vomiting, no focal neurologic symptoms |
|
Tumor Morphology and Location |
A midline clival mass with the presence of a normal pituitary gland being displaced superiorly |
A large clival mass: 3.2 cm x 2.9 cm x 3.1 cm; occupying sphenoid sinus, invading clivus and bony sellar walls |
|
Growth Patterns and Invasiveness |
Tends to show more advanced invasive changes in sphenoidal and clival regions |
Invasive features evident in the skull base, sphenoid, and cavernous sinuses, with the pituitary gland not seen separately or distinctly on imaging |
|
CT Findings |
Extensive sphenoid and clival involvement |
Bony erosion, mass extending into bilateral sphenoid sinuses, invading sphenoid septum and pituitary fossa |
|
MRI Findings |
Higher T2 and DWI signal intensity, higher ADC values, heterogeneous T2 hyperintensity, T1 isointense features compared to native pituitary gland |
Displacement of pituitary gland superiorly, partial encasement of bilateral cavernous segments of ICA, heterogenous T2 hyperintensity, T1 isointense features |
This is a case report of a 51-year-old woman who presented with nasal pain and was diagnosed with a clival lesion. Initially suspected to be a chordoma, the lesion was later confirmed as a pituitary neuroendocrine tumor following a biopsy. The report details the challenges in diagnosing this case. The lesion's origin, whether clival or pituitary, was difficult to ascertain due to its size, invasive nature, and imaging characteristics. Initially, radiological assessments suggested possible chordoma or chondrosarcoma, but these were ruled out with an endoscopic biopsy, which identified the lesion as a pituitary neuroendocrine tumor. This case emphasizes the complexity of diagnosing clival lesions and the essential role of biopsy in obtaining an accurate histological diagnosis, especially when radiological features are atypical. It highlights the potential for misdiagnosis based on imaging alone and underscores the importance of histological confirmation. The report offers significant educational value by providing a detailed account of the complex diagnostic process for a clival lesion, ultimately identified as a pituitary tumor. By highlighting the challenges in differential diagnosis of clival lesions, this case contributes to the medical literature. It underlines the necessity of integrating imaging with histopathological examination and advocates for a multidisciplinary approach in handling complex medical cases. The article demonstrates a high level of proficiency and, upon resolution of specific issues, would merit publication.
In this case report, the authors document the medical journey of a 51-year-old female patient who initially presented with persistent nasal pain. This ultimately led to the identification of a clival lesion. Initially, the medical team suspected a chordoma, but subsequent biopsy results revealed it to be a pituitary neuroendocrine tumor. The authors followed a systematic approach to diagnosis and treatment, employing advanced imaging, precise biopsy techniques, and appropriate surgical procedures. The report adheres to established medical standards without significant omissions or deviations. Furthermore, this report underscores the critical importance of conducting a thorough evaluation when confronted with intricate cranial base tumors. Although this article is well-written and supports its case for publication, it is essential to acknowledge the necessity for careful consideration and resolution of certain elements before it can be deemed fully prepared for scholarly dissemination.
Fong PY, Low DYM, Lee TS, Pang MCY. Managing a complex pituitary tumor: A case study on effective diagnosis and treatment of a challenging clival lesion. Arch Otorhinolaryngol Head Neck Surg. 2024;8(1):1. https://doi.org/10.24983/scitemed.aohns.2024.00180