A 59-year-old woman had an intrathecal morphine pump therapy for the last 20 years, due to chronic lumbar back pain and L4,5 post-laminectomy syndrome, and was presented with 6 days onset of lower thoracic back pain accompanied with feelings of heaviness and tingling below mid-thigh level bilaterally. There was no change in the drug concentration (20 mg/ml) within the last four years. She denied having fever, headache, confusion, saddle anesthesia, bladder or bowel incontinence and history of cancer. Upon examination she had decreased pin-point sensation, and absent vibration sense below mid-thigh level bilaterally with intact motor exam.
The gadolinium enhanced magnetic resonance imaging (MRI) of thoracic spine showed an intraspinal extramedullary ring enhancing lesion at T10 level abutting the spinal cord posterior-laterally on the right side (Figures 1-6). MRI of the head, and the cervical and lumbar spines were unremarkable. Cerebrospinal fluid analysis was normal and cultures were negative for infection. She was diagnosed with catheter tip granuloma [1,2] and the intrathecal morphine was stopped. Pump was operated with normal saline, and serial thoracic MRI was obtained every week until symptoms were resolved after 2 weeks; and granuloma was resolved after 3 weeks.

Figure 1. Gadolinium contrast enhanced mid-line sagittal view of thoracic spine MRI. intraspinal extramedullary ring enhancing lesion at T10 level abutting the spinal cord posterior-laterally on the right side. It measured 14.8 mm superior to inferior and 7.7 mm anterior to posterior abutting the spinal cord posterior-laterally on the right side with no signs of inflammation. MRI, magnetic resonance imaging.

Figure 2. STIR thoracic MRI mid-line sagittal view with no signs of inflamation. MRI, magnetic resonance imaging; STIR, short inversion time inversion recovery.

Figure 3. T1-weighted thoracic MRI mid-line sagittal view. MRI, magnetic resonance imaging.

Figure 4. T2-weighted thoracic MRI mid-line sagittal view. MRI, magnetic resonance imaging.
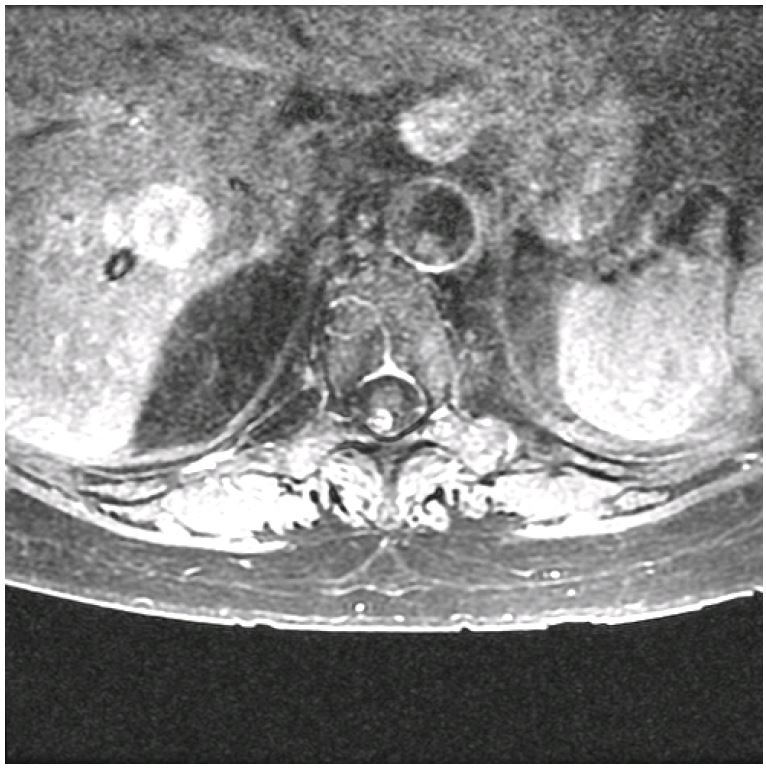
Figure 5. Gadolinium contrast enhanced transverse view of thoracic spine MRI at upper T10 level. MRI, magnetic resonance imaging.
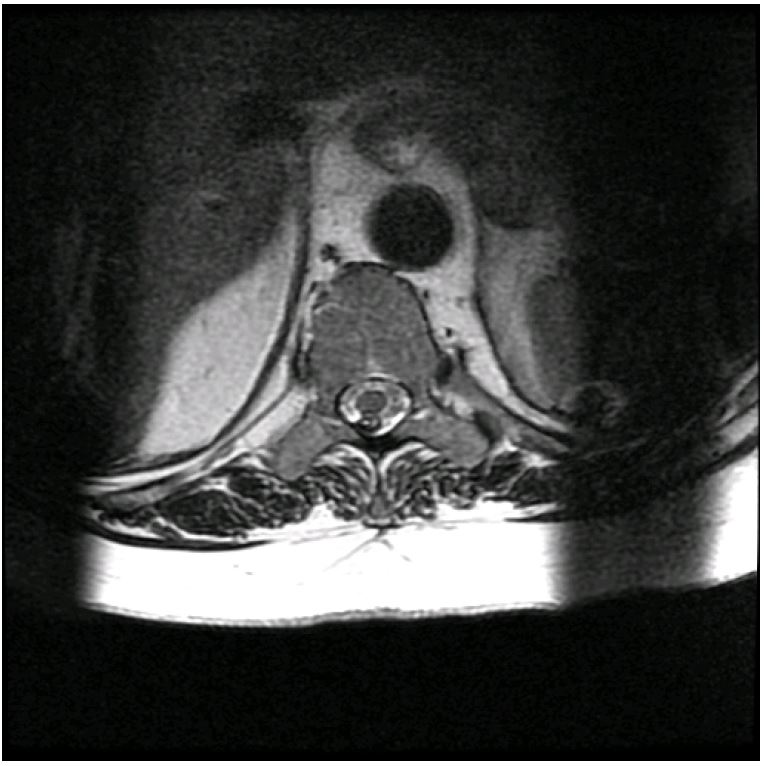
Figure 6. T2-weighted transverse view of thoracic spine MRI at upper T10 level. MRI, magnetic resonance imaging.
Received date: July 26, 2017
Accepted date: October 27, 2017
Published date: June 20, 2018
None
None
© 2018 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Jain G, Rizk NN. Spinal cord compression due to a catheter tip granuloma of an intrathecal morphine pump. Neurol Neurosci Res 2018;1(1):5. https://doi.org/10.24983/scitemed.nnr.2018.00066