Esophageal granular cell tumors (GCT) represent a rare entity of tumors of the esophagus. Patients with esophageal GCTs are usually asymptomatic, with the lesion most commonly presenting as an incidental finding on endoscopy. The GCTs of the esophagus are poorly understood in medical literature. It is unknown if they undergo malignant degeneration, whether the malignancy can be diagnosed preoperatively, and how the tumor can be managed. Therefore, we evaluated the clinical and pathologic features of all esophageal GCTs at our institution to understand them better. A retrospective review of the Department of Pathology database at Singapore General Hospital was performed, looking at all cases of esophageal GCTs between 1990 and the present. Four cases of esophageal GCTs were found. A total of 4 patients were diagnosed with esophageal GCTs. All the patients were female with a median age of 45. The tumors were less than 10 mm in size and most of the lesions were located in the mid-esophagus. Three patients had abdominal symptoms while the other was asymptomatic. Active follow-up for 2 patients revealed no further change in the characteristics of the lesion.Esophageal GCT should be considered in the patients diagnosed with sub-epithelial lesions in the distal esophagus. Upper gastrointestinal endoscopy and biopsy are the mainstays of diagnosis, and surveillance is indicated.
Granular cell tumors (GCT) are uncommon, benign soft tissue neoplasms originating from Schwann cells. GCTs of the esophagus are even rarer and most GCTs occur as isolated lesions. Patients are usually asymptomatic, and the lesions are usually diagnosed incidentally on endoscopy. GCTs were first reported by Abrikossoff in a case series composed of benign tumors that were removed from the tongue, and according to medical literature, they could be found in other sites of the body as well [1]. However, the GCTs of the esophagus remain a poorly understood clinical entity. A retrospective review of the Singapore General Hospital Department of Pathology database was performed between 1990 and the present and 4 cases of esophageal GCTs were found. We thus report a case series of 4 patients diagnosed with GCT of the esophagus in our institution to further understand the clinical and pathological characteristics of these tumors and discuss on their follow-up and management.
Case 1
Case 1 was a 56-year-old female who was presented to our clinic with reflux. An esophagogastroduodenoscopy (EGD) performed revealed a mid-esophageal submucosal lesion. Histology returned as granular cell tumor (Figure 1). The tumor showed hyperplastic stratified squamous epithelium with nests of uniform, rounded, and polygonal lesional cells in the lamina propria. The cells contained a fine to coarse, eosinophilic granular cytoplasm with round nuclei. Lesional cells were positive for S100, PAS, and CD 68. She had a repeated endoscopy performed the following year, which revealed similar histology. She then defaulted from follow-up with us.
Case 2
Case 2 was a 31-year-old female presented to us with epigastric pain. EGD performed revealed an esophageal submucosal lesion where histology returned as granular cell tumor. The cells showed squamous mucosa with an underlying proliferation of nests, islands, and sheets of large cells with ample granular eosinophilic cytoplasm with small nuclei. The cells were positive for S100 protein and negative for CD34 and CD117(c-kit). She then had an endoscopic ultrasound (EUS) performed, which showed esophageal mucosal tumor of around 5 x 5 mm in size, with no extension to the submucosa. The tumor was located at the mid-esophageal lesion, around 31 cm from the incisor. She then had a CT thorax abdomen pelvis performed, which was normal. She had been under our follow-up for 7 years with no active change in her condition.
Case 3
Case 3 was a 44-year-old female who was presented to our clinic for abdominal bloatedness. EGD performed revealed a mid-esophageal submucosal lesion, 25 cm from incisors, where histology returned as GTC. Similarly, the lesional cells were positive for S100, PAS, and CD 68. She was under 11 years post-diagnosis and remained asymptomatic.
Case 4
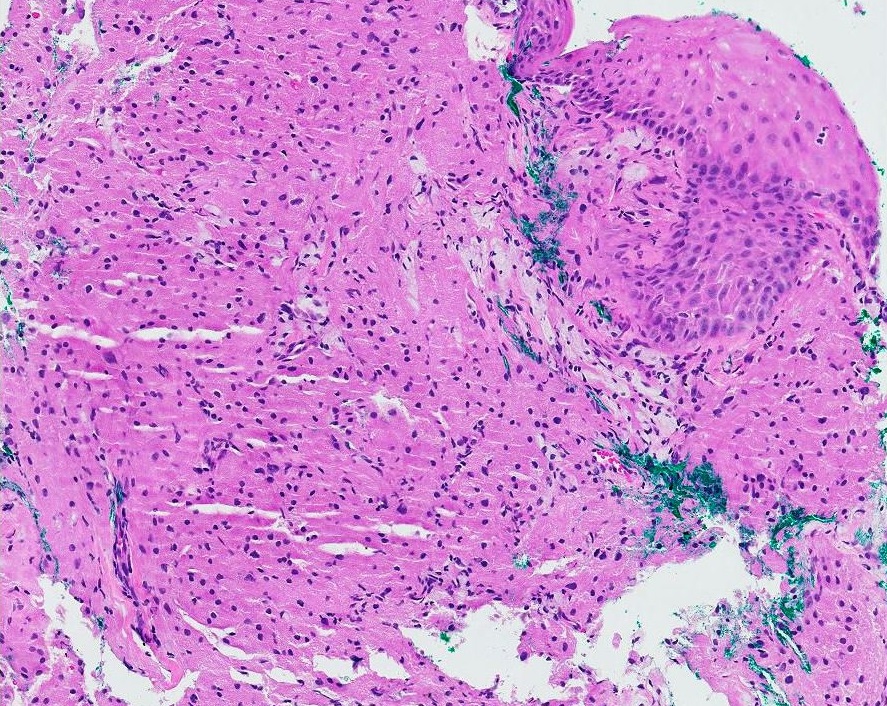
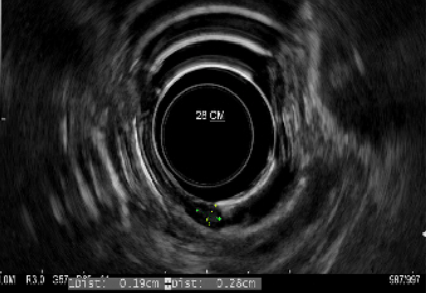
Case 4 was a 44-year-old female who had upper and lower gastrointestinal endoscopy performed for anemia. EGD revealed a 3 mm nodule located at 28 cm from incisors, with the histology returned as GCT (Figure 2). She then underwent an EUS, which revealed a lesion arising from the mucosa without extension into the surrounding structures (Figure 3). She had endoscopic mucosal resection performed with histology returned as granular cell tumor of 3 mm in size with clear margins. Immunohistochemical staining for S100 was strongly positive. She was under a 2-year post-procedure and showed no recurrence.
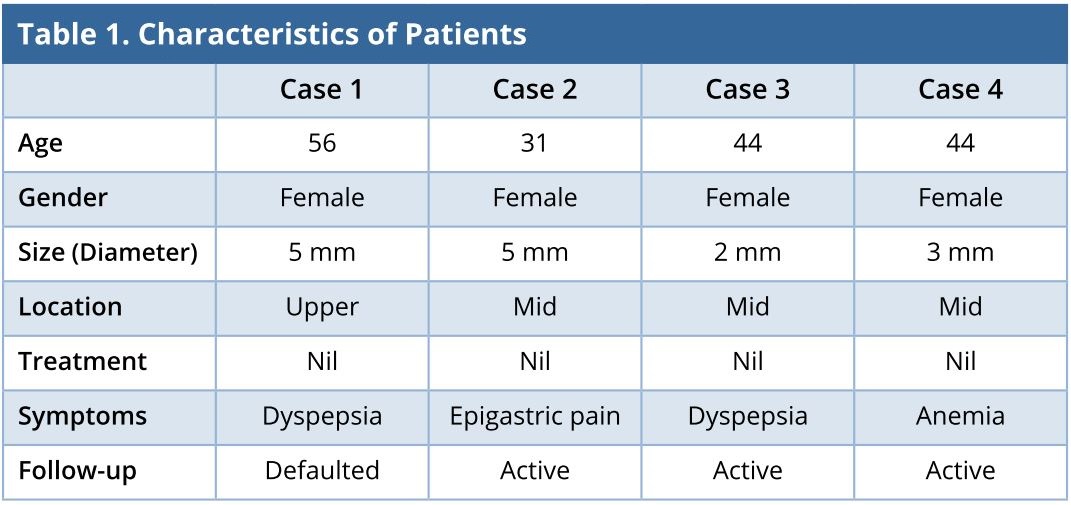
The clinical and pathological characteristics of these patients are summarized and presented in Table 1.
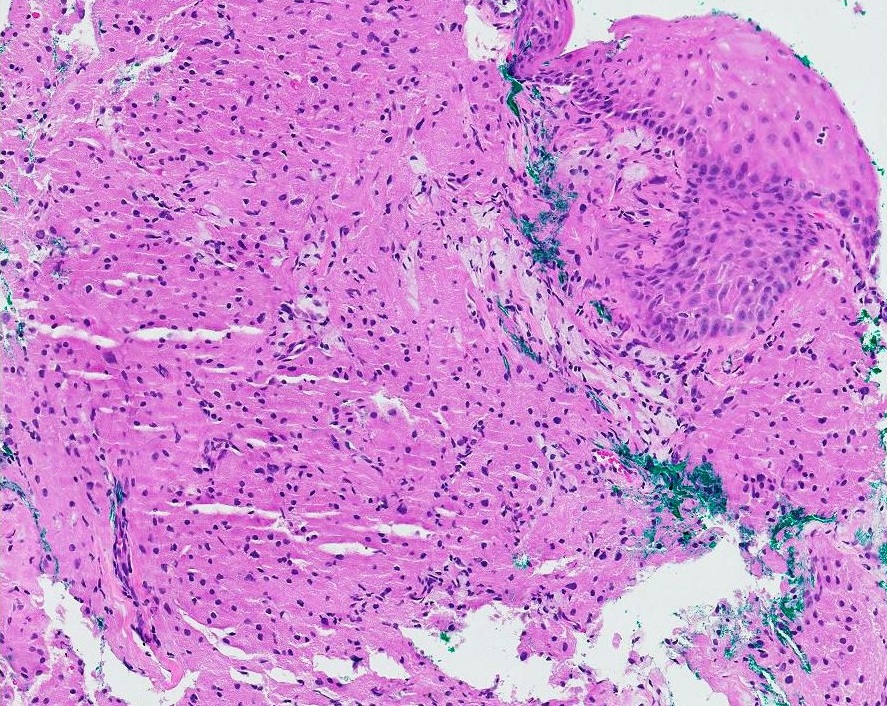
Figure 1. Granular cell tumour of the esophagus (H&E stain, 10x).

Figure 2. Endoscopic image of submucosal lesion of the esophagus.
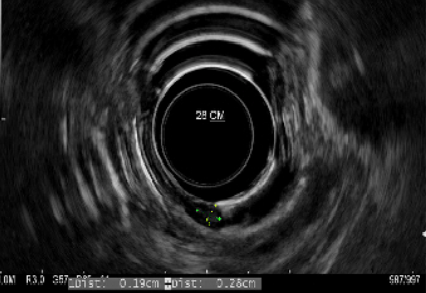
Figure 3. Endoscopic ultrasound features of granular cell tumor. Lesion arising from mucosa layer and does not extend to surrounding structures.
Granular cell tumors of the esophagus occur mainly in the middle age and most tumors are solitary and benign [2]. They were first described by Abrikossoff in 1931. GCTs occur in the tongue, skin, breast, respiratory tract, biliary system, and digestive tract [1]. Several detailed reviews found that approximately 1 to 8 % of all GCTs occur in the gastrointestinal tract [3,4]. In the digestive tract, the esophagus is considered the most common site of occurrence. Esophageal GCT is the second most common esophageal stromal tumor after leiomyoma [5].
The most common location in the esophagus for GCTs is the distal esophagus. Orlowska et al. reported that 65% of esophageal GCTs were detected in the distal esophagus, with only 20% and 15% in the middle and the upper esophagus respectively [6]. However, in our series, 3 patients had lesions detected in the mid-esophagus, while one had the lesion found in the upper esophagus. Female predominance was reported in the literature with 2.9:1 female to male preponderance [16]. In our series, all patients were female.
Most GCTs of the esophagus are asymptomatic. However, when the tumor diameter is more than 1 cm, the patients may present with dysphagia [7]. Other symptoms associated with esophageal GCTs are abdominal symptoms, which include abdominal distension, dyspepsia, and loss of appetite. The authors feel that the correlation between the symptoms and the presence of an esophageal GCT is not strong; in our series, 3 patients had vague abdominal symptoms and one patient was scoped for investigation of anemia. We thus feel that the finding of a GCT on endoscopy was more incidental and the tumor may or may not explain the patients’ symptoms. Esophageal GCTs can be diagnosed via endoscopic biopsy. These tumors frequently present as a submucosal mass during endoscopic evaluation. Obtaining multiple biopsy specimens at the same site allows for better access to the submucosa [8]. Another alternative would be the endoscopic ultrasound (EUS). A GCT on EUS would appear as a round, hypoechoic, and homogeneous lesion with clear borders. Palazzo et al. found that GCTs had three characteristics: (1) tumor size < 2 cm in 95% of cases; (2) a hypoechoic solid pattern in all cases; and (3) a tumor arising in the inner layers in 95% of cases [9]. Endoscopic ultrasound is useful to distinguish GTC from lipoma, which can also arise in the submucosal layer. However, lipomas are more hyperechoic, differentiating it from GCTs. In our series, 2 patients underwent endoscopic ultrasound, which revealed the lesion arising from the mucosa. The lesions were hypoechoic and solid, with clear margins, which corresponded to Palazzo’s initial findings.
Histology of GCTs reveals large, polygonal Schwann cells with granular and eosinophilic cytoplasm. The cell nuclei are ovoid with fine chromatin and no mitotic figures. The cells are arranged in a nest or acinar form [10]. The tumor is usually benign and remains biologically quiescent for a long period of time. However, approximately 2% of them can be malignant. A report by Wyatt et al. identified 3 cases of malignant GCT of the esophagus in a total of 29 cases of malignant GCTs in various organs [10]. The size of the tumor is important as the malignant potential of GCT increases when it exceeds 50 mm in diameter. In our series, all patients had a tumor diameter of 5 mm and below.
Detecting esophageal GCT is straightforward, but the treatment of GCT remains controversial. Currently, GCTs can be managed via the following approaches: (1) Conservative endoscopic follow-up of patients with tumors < 1 cm in length, provided that the biopsy does not reveal any signs of malignancy; (2) Removal of lesions of > 2 cm in length by EMR or endoscopic submucosal dissection; or (3) Resecting lesions that are symptomatic or displaying malignant features [11].
Endoscopic polypectomy can be performed in patients with a tumor less than 2 cm and not attached to muscularis propria [12]. The main dilemma with GCTs is in determining the malignancy potential. A vast majority of GCTs were histologically benign and in most cases, malignancy was diagnosed retrospectively upon discovery of lymph node metastases, and re-review of the original tumors found most lesions to be indistinguishable from the histologically and clinically benign GCTs [13]. Thus, several other authors such as Narra et al. suggested treatment options that included endoscopic surveillance, endoscopic resection, and surgery [14]. Asymptomatic GCTs less than 10 mm did not require surgical resection and should be followed up with surveillance endoscopy [15].
In our series, all the 4 cases had only endoscopic surveillance but one patient was lost to follow-up. Fortunately, the prognosis of esophageal GCT is good, and the recurrence and metastasis are uncommon.
When clinicians are presented with sub-epithelial lesions in the distal esophagus, a potential differential should be the esophageal GCTs. Upper gastrointestinal endoscopy and biopsy are the mainstays of diagnosis and the endoscopic ultrasound can provide additional information, namely, a layer of origin and tumor extension. Surveillance is indicated if the patient is symptomatic, and the tumor size is larger than 1 cm or has atypical endoscopic ultra-sonographic or histologic features. Esophageal GCTs have low malignant potential and the asymptomatic patients should be followed up with surveillance.
Received date: July 04, 2018
Accepted date: July 25, 2018
Published date: August 16, 2018
None
None
© 2018 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).

The authors report a case of otogenic Lemierre's syndrome in a male patient who presented with atypical symptoms and was subsequently treated aggressively with antibiotics and surgery. In this article, the authors demonstrate how they could have avoided serious complications by diagnosing and treating the patient earlier. The authors suggest key points that should be noted in clinical practice in order to prevent misdiagnosis or delayed diagnosis of Lemierre's syndrome.
I have reviewed the revised article. I accept it for publication.
The revision is accepted for publication.
Tan HJ, Chong CXZ, Lim KH, Ong HS. Granular cell tumor of esophagus: A rare disease of the esophagus. Ann Case Rep Images 2018;1(1):3. https://doi.org/10.24983/scitemed.acri.2018.00076