Video Abstract
Eustachian tube dysfunction (ETD) can lead to a loss of vestibular function and eventually give rise to peripheral vestibular loss [1]. Vertigo caused by ETD is a distinct clinical entity [2]; therefore, a comprehensive understanding of the mechanism underlying vertigo is essential to elucidate the reciprocal causal relationship between laryngopharyngeal reflux and Eustachian tube obstruction [1].
In 1838, Nicolas Deleau the Younger (1799-1862), who was an expert in Eustachian tube catheterization, published a notable report in which the use of an India-rubber ball or an air pump as “douche d'air [air show-er-air douche]” was first documented [3]. Deleau reported that the douche d’air had initially been used for therapeutic purposes and then for diagnosis [4]. Deleau also described at least one patient who presented the three symptoms of dizziness, tinnitus, and hearing impairment, which were later defined as Menière's disease. He treated the patient by catheterizing the Eustachian tube and administering an air douche, which ameliorated symptoms [5]. This case is a typical example of why ETD should be ruled out before considering a diagnosis of Menière's disease [6]. ETD has long been recognized as a principal cause of hearing loss, tinnitus [7,8] and ‘vertigo’ [1,2,6-8]. Therefore, patients who exhibit such symptoms should be subjected to a therapeutic test of inflation of the tubes as a first step in a thorough clinical investigation [2].
Eustachian tube dysfunction is typically defined as a failure of the functional valve of the Eustachian tube to open and/or close properly. (However, note that a patulous (chronically patent) Eustachian tube, which is a common condition, has different clinical characteristics.) Vertigo from ETD can be explained by a pressure increase that occurs within a vestibular organ. Specifically, negative pressure in the middle ear can cause the tympanic membrane to retract, which in-turn causes the stapes to push against the oval window [7]. It is very likely that dysfunction of the Eustachian tube disturbs the air pressure in the middle ear cavity and stimulates the perilymph, which interferes with balance, which is normally maintained by the labyrinthine mechanism [2]. A number of researchers have noted that dizziness induced by a fluctuation in middle ear pressure is an example of alternobaric vertigo, a syndrome that occurs when an individual is able to ‘clear’ one ear but not the other [9-13]. Alternobaric vertigo resulting from ETD mainly affects scuba divers and airplane pilots.
The syndrome is likely caused by (1) asymmetry pressure in the inner ear in conjunction with a change in middle ear pressure or (2) displacement of otolithic membranes and the ossicular chain in conjunction with an imbalance in pressure between the middle and external ear. Pressure sensitivity is typically viewed as a symptom of some other underlying disease; therefore, it tends to be regarded as a normal variant [9-13]. However, physicians often fail to identify ETD as a potential cause of symptoms in patients who complain of nausea, vomiting, and perspiration accompanied by concomitant vertigo [1,2,8].
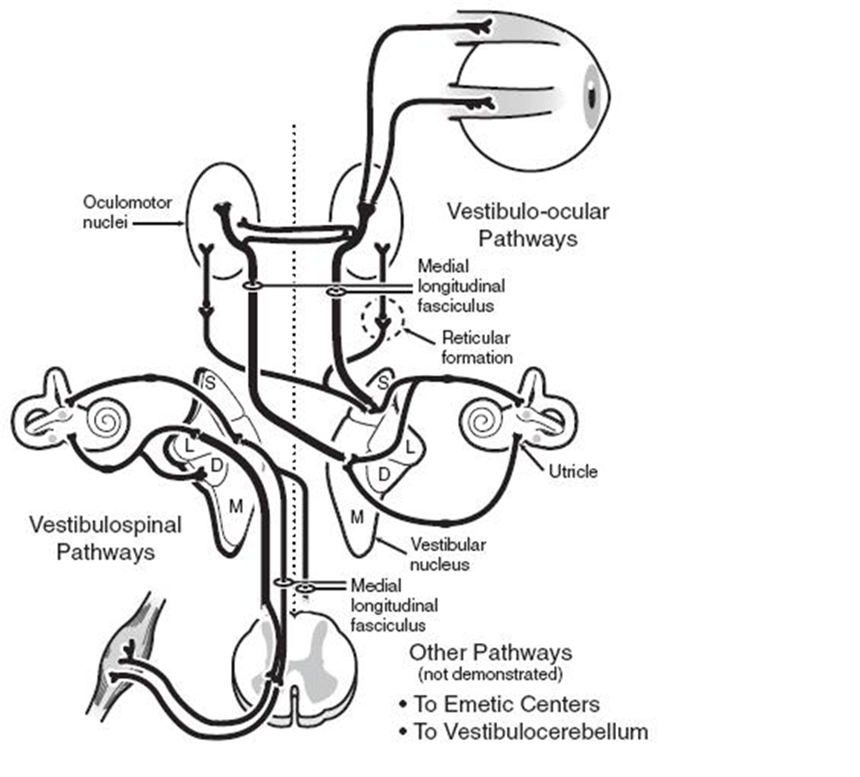
Humans perceive head movement (relative to the body) through the activity of linear (otolithic macula) and angular (semicircular canals) acceleration receptors in the inner ear. Electrical activity generated within the inner ear travels along the vestibular nerve (primary afferent neuronal pathway) to the central vestibular nuclei of the brainstem, forming second-order neuronal pathways that become the vestibulo-ocular reflex (VOR), vestibule spinal tracts, or vestibule cerebellar tracts. Pathways derived from vestibular information also connect to emetic centers in the brainstem, which explains why a patient typically experiences vegetative symptoms, such as nausea, vomiting, and perspiration, following acute unilateral vestibular loss (Figure 1) [14].
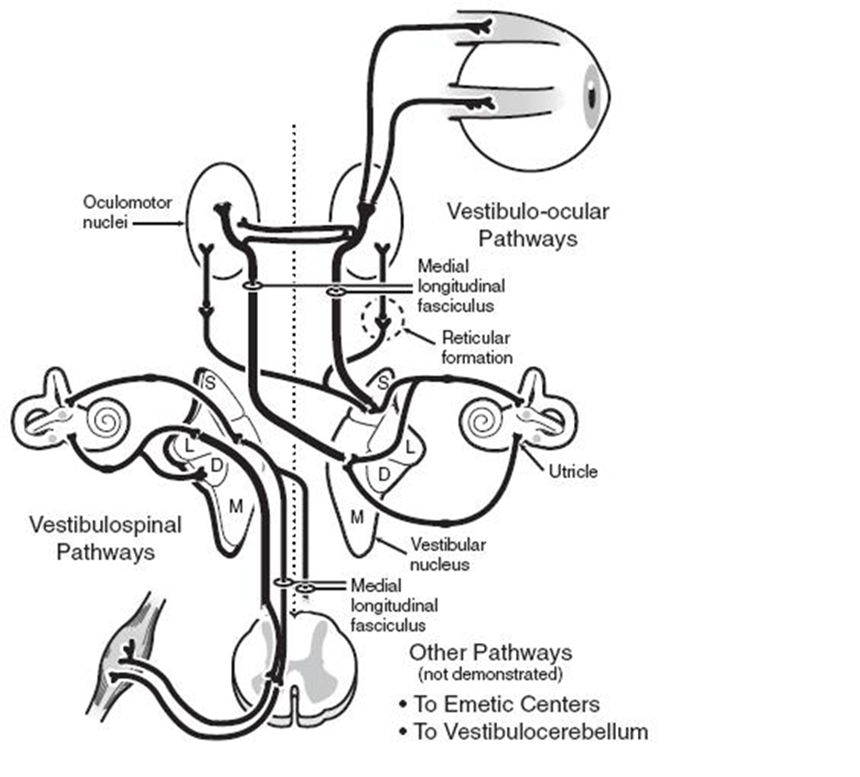
Figure 1. Schematic representation of the vestibular system and its pathways [14].
When a patient loses unilateral vestibular function due to unilateral ETD, he/she experiences an acute sensation of true vertigo, due to interruptions in the VOR pathways. Patients with these symptoms generally prefer to lie perfectly still, due to the fact that any movement can aggravate vegetative symptoms arising from emetic centers. Nystagmus beating away from the side of a lesion is the primary physical sign that obeys Alexander’s law. The quick phase of nystagmus, which is induced by an imbalance in vestibular nuclei activity, shows the greatest amplitude and frequency when the eyes are turned away from the side of the lesion [15]. Moreover, interruptions in vestibulospinal tract pathways can cause the patient to fall or list toward the affected side. Ipsilateral hemispheric cerebellar dysfunction that presents with behaviors, such as past-pointing, an inability to perform rapid alternating movements (dysdiadochokinesis), and gait ataxia are further indicative of acute vestibulocerebellar tract involvement [16]. In most or perhaps all cases, symptoms of vertigo are caused by unilateral ETD or by a Eustachian tube obstruction due to ETD that is more severe on one side than on the other. The direction of gait can indicate which side is affected, as most patients stagger towards the direction of the obstructed side [2]. Simply stated, unilateral ETD can cause a loss of unilateral vestibular function, which in-turn causes unilateral peripheral vestibular loss vertigo with nausea, vomiting, and/or nystagmus [1]. With compensation (implying that the central nervous system and contralateral peripheral vestibular system are normal and functional), symptoms may be minimal and may only be elicited by very rapid head movements. Spontaneous nystagmus subsequently disappears, vegetative symptoms are resolved, and gait improves. However, if the condition is chronic, the patient may still experience slight imbalance when turning quickly [16]. For this reason, no vestibular function test should ever be performed prior to ETD correction and the normalization of pressure in the middle ear [1].
Vertigo is not a feature of bilateral vestibular loss due to bilateral ETD, even when it is acute. Injury to end organs, which can occur in systemic aminoglycoside vestibulotoxicity, causes a bilateral loss of function, which tends to be electrically symmetric at the level of the vestibular nuclei in the brainstem. Patients with this syndrome tend to complain of oscillopsia (visual blurring with head movement) and imbalance. The gait is typically broad-based and ataxic, particularly when the eyes are closed. Falls are not infrequent and, in many instances, the patient requires assistive devices for ambulation or is relegated to a wheelchair. Compensation is generally unlikely even under good vestibular rehabilitation therapy and/or increased reliance on information from visual and proprioceptive receptors [16]. In other words, bilateral ETD causes bilateral loss of vestibular function, but does not cause bilateral peripheral vestibular loss vertigo. We can say that bilateral ETD can cause oscillopsia and imbalance but not vertigo [1]. It is therefore reasonable to question what pressure range in the middle ear cavity would be considered normal (i.e. does not impact vestibular function) [1].
In conclusion, vertigo due to ETD is caused by a pressure imbalance between the middle ear cavities of the two ears. Middle ear pressure is frequently influenced by the function of the Eustachian tube. Vestibular organ dysfunction is conceptualized as the need for better pressure regulation of middle ear pressure; therefore, vestibular organs are considered to be dependent variable organs. Every clinical test currently used to assess vestibular function should ideally be performed in a state where pressure in the middle ear cavity is in the normal range and perfectly balanced between the two ears [1,6-8].
Received date: May 22, 2017
Accepted date: June 04, 2017
Published date: June 16, 2017
ETD, Eustachian tube dysfunction; VOR, vestibulo-ocular reflex
© 2017 The Author. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Video Video abstract
According to this article, Meniere's disease might actually be a generic term referring to an inner ear disorder that causes vertigo and hearing loss. The author suggests that physicians should pay more attention to discussing any pathological changes associated with hearing loss and vertigo with patients rather than narrowly focusing on confirming the diagnosis of diseases.
Kim HY. Vertigo due to Eustachian tube dysfunction. Arch Otorhinolaryngol Head Neck Surg 2017;1(1):5. doi:10.24983/scitemed.aohns.2017.00017