Objectives: Transcanal endoscopic ear surgery (TEES) has become one of the most influential methods for the treatment of cholesteatoma. The present study aimed to discuss the feasibility of transcanal endoscopic management of congenital cholesteatoma in pediatric patients.
Methods: Two children with a diagnosis of congenital cholesteatoma underwent transcanal endoscopic tympanotomy and extended atticotomy to completely remove a cholesteatoma. The evaluations of these cases included surgical time, hearing gain, post-operative complications, and mastoid function reservation.
Results: There were no complications after the surgeries, and the patients were followed up for at least 6 months; excellent clinical appearance and hearing improvement were noted.
Conclusion: These cases demonstrated that TEES could be a satisfying alternative to traditional microscopic surgery for the management of congenital cholesteatoma, even in pediatric patients. However, one-handed surgery demands greater skill and requires more practice to achieve a good outcome.
Video. Transcanal endoscopic ear surgery for congenital cholesteatoma.
A cholesteatoma is defined as an epidermal cyst in the middle ear without a previous history of ear infection, head trauma, or ear surgery [1]. The cause of congenital cholesteatoma remains controversial, but the theory of retained epithelial cells has the most support and empirical evidence.
Some authors have reported that upper airway infection and otitis media may increase growth factors or matrix metalloproteinases, which can enable the cholesteatoma to become more invasive and destroy more of the surrounding structures [2]. Congenital cholesteatoma is managed through prompt surgical removal. Traditionally, microscopic transmastoid surgery via a retroauricular approach has been the most widely used procedure. However, the loss of additional healthy mastoid air cells and damage to the intact cartilaginous portion of the ear canal are inevitable during this procedure. The additional damage may result in unpredictable healing patterns, fibrosis, and narrowing of the meatus, and often prevents further ossicular reconstruction. In contrast, endoscopic techniques allow transcanal exploration of the disease-containing cavities without opening unaffected areas. This in turn creates a better framework for ossicular and tympanic membrane reconstruction.
In recent years, more studies have demonstrated the benefits of TEES for the management of cholesteatoma in adult patients, including a clearer operation field, closer surgical views, and improved preservation of the mastoid air cells and ventilation function of the middle ear [2-4]. The two cases described here demonstrate the technique of TEES for the treatment of pediatric congenital cholesteatoma; the feasibility of applying this new technique in pediatric cases is discussed.
Case1
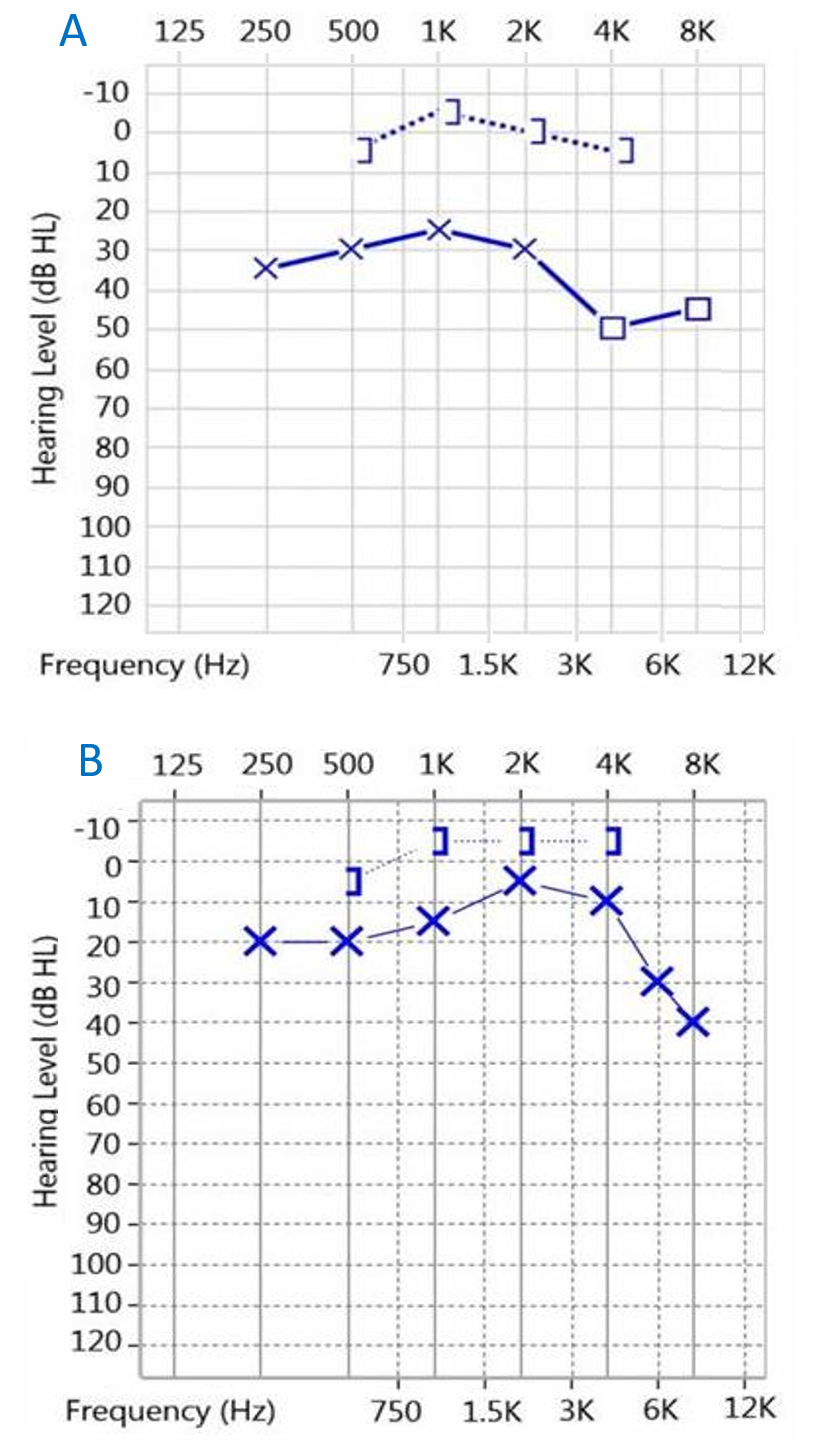
A 5-year-old girl came to our facility due to left side hearing impairment. There was no prior history of otitis media; the left eardrum was intact, and there was a hidden white mass beneath the post-superior quadrant (Figure 1A). Left ear audiometry showed conductive hearing loss with an air-bone gap (ABG) at approximately 32.5 dB (Figure 2A). The high-resolution computed tomography (HRCT) of the temporal bone revealed a soft tissue mass in the attic and the posterior-superior quadrant of the tympanic cavity. TEES was used to remove the congenital cholesteatoma. Ossiculoplasty and reconstruction of the middle ear were performed simultaneously.
Case 2
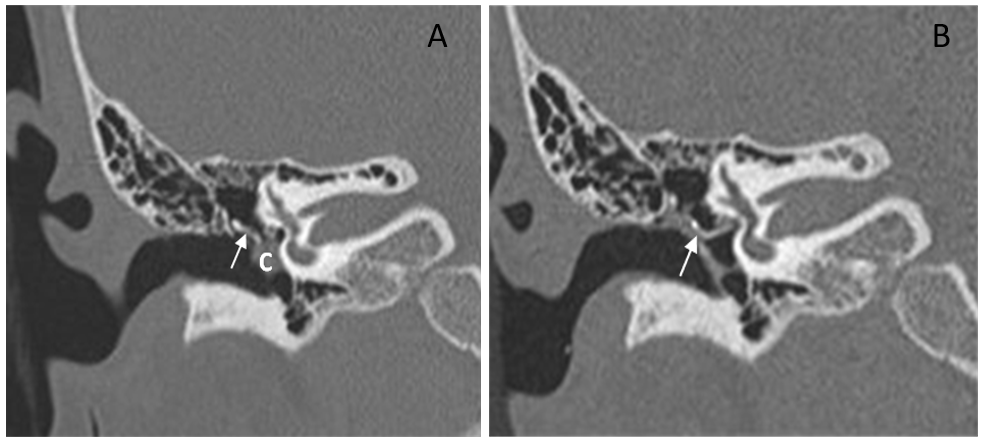
A 9-year-old girl had a history of congenital cholesteatoma in the right ear 5 years previously; it was treated using the retroauricular approach: removal of the growth using microscopic surgery. Unfortunately, a white mass beneath the intact eardrum was found at the 5-year follow-up. In addition, the HRCT revealed a soft tissue mass in the posterior tympanum with suspected ossicular chain destruction (Figure 3A). This time, TEES was used to remove the recurrent cholesteatoma completely. Ossiculoplasty and reconstruction of the middle ear were performed simultaneously.
Instrumentation
Endoscope A wide-angle endoscope (HOPKINS® telescopes ) with a diameter of 3 mm, a length of 14 cm, and angles of 0 and 30 degrees was used.
Video equipment A three-chip video camera and a monitor were used.
Instruments Ear instruments with elevators, a micro dissector, joint knife, micro forceps, House-Bellucci alligator scissors, alligator, cupping forceps, and curettes were used.
Operating room layout The surgeon operated beside the lesion ear, directly facing the monitor placed on the opposite side of the table across the patient’s head. The three-chip video camera set was covered with a sterile bag. An absorbent pad soaked with anti-fog solution was placed at the patient’s head.
Preoperative Evaluation
A detailed history, a physical examination, and a hearing survey were necessary. A temporal bone HRCT was also essential to estimate the extent and location of the cholesteatoma and identify the erosion of the ossicles, fallopian canal, and scutum (Figure 3A).
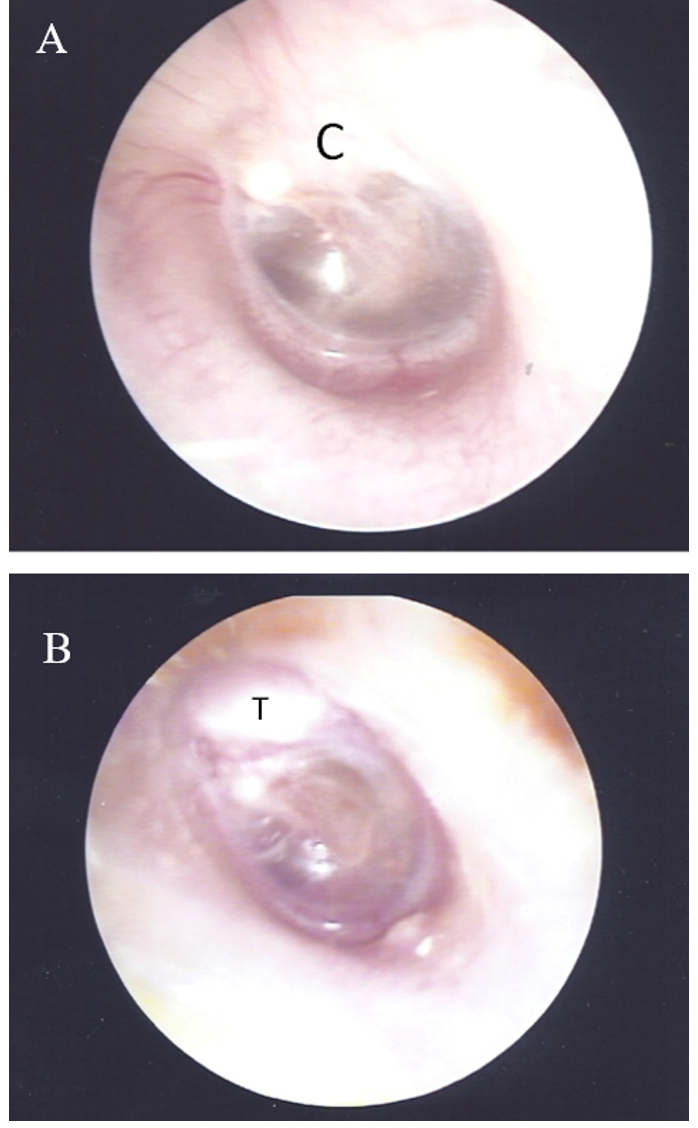
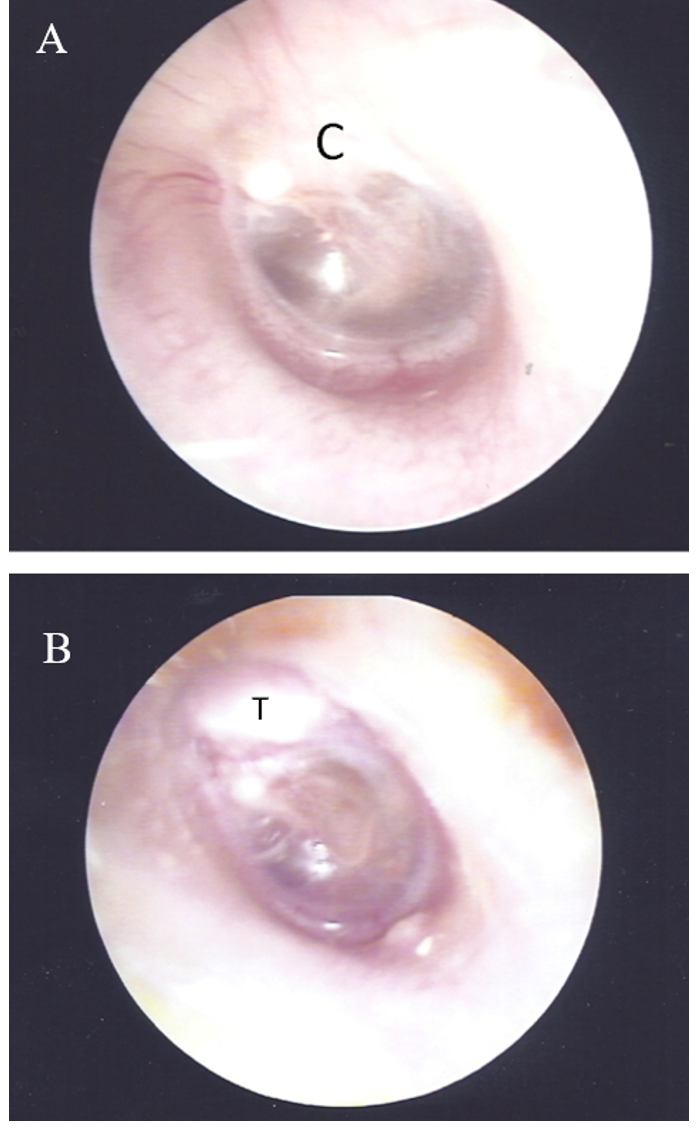
Figure 1. Otoscopy image of the left ear of a 5-year-old girl (case 1). A, before surgery, a whitish mass was visible beneath the superior posterior quadrant of the eardrum. B, two months after surgery, reconstruction with tragus cartilage and TORP. Abbreviations: C, cholesteatoma; T, tragus cartilage.
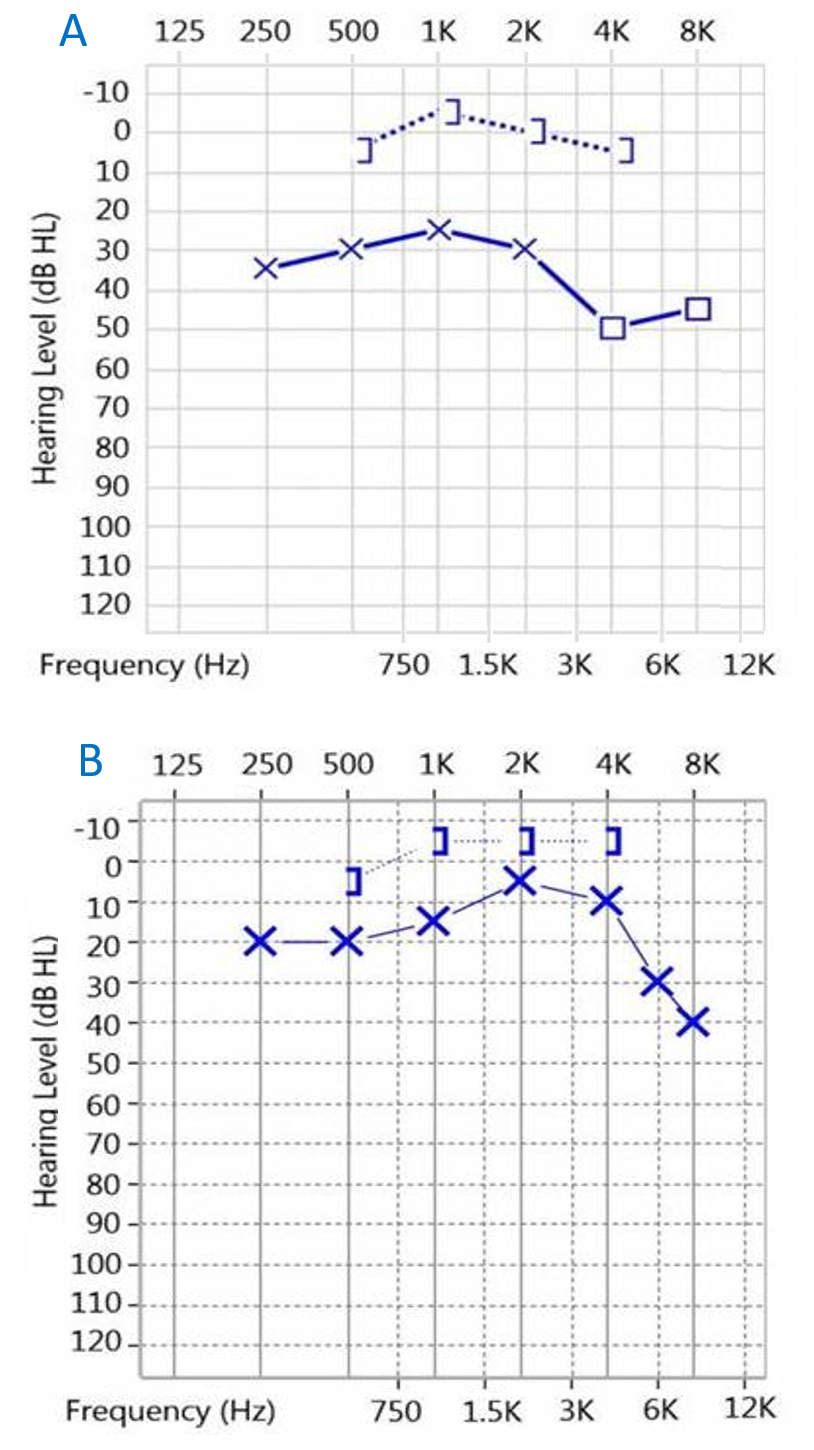
Figure 2. Left ear audiometry of a 5-year-old girl (case 1). A, Pre-operative air-bone gap 32.5 dB. B, Post-operative air-bone gap 15 dB.
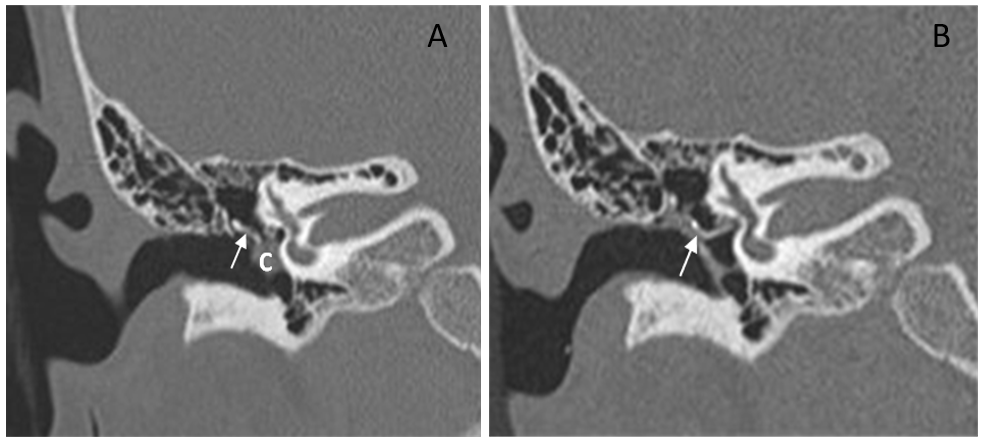
Figure 3. High-resolution computed tomography of temporal bone of the right ear in a 9-year-old girl (case 2). A, before surgery. Cholesteatoma at the mesotympanum; the ossicle chain was decayed (arrow = decayed incus). B, six months after surgery. The lesion was cleaned, and the TORP ossiculoplasty was observed in the correct position (arrow = tragus cartilage and TORP). Abbreviation: C, cholesteatoma.
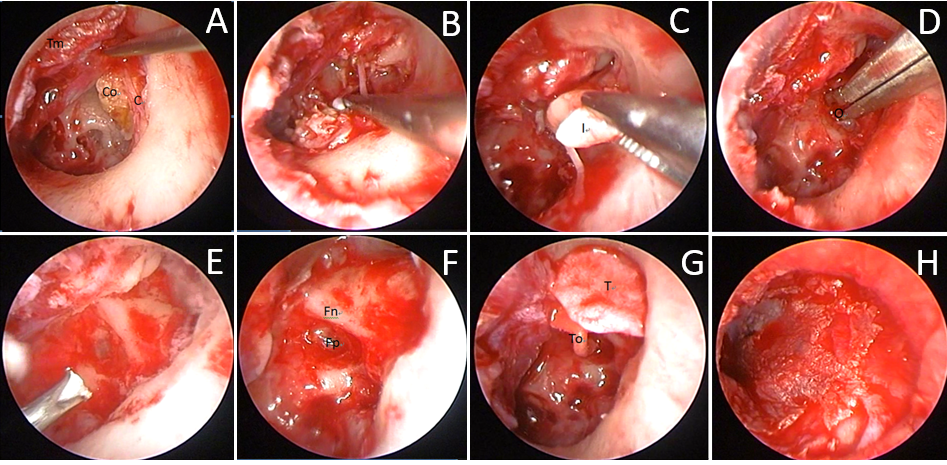
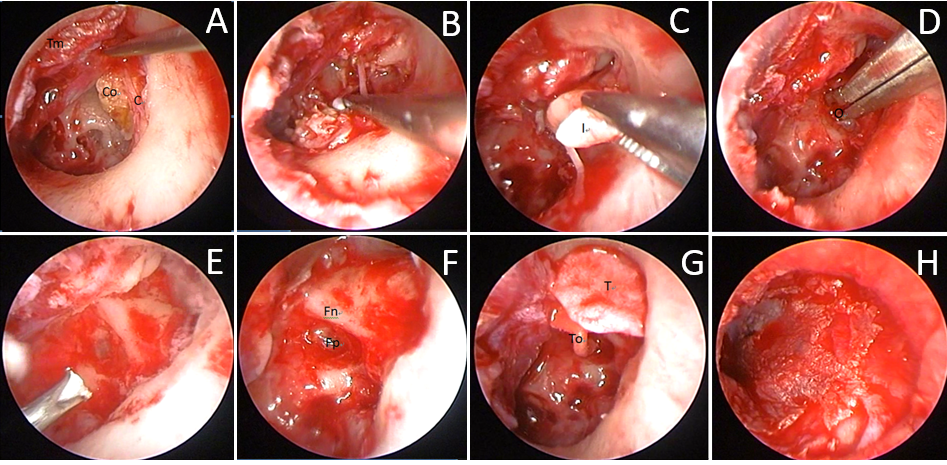
Figure 4. Surgical image of TEES congenital cholesteatoma removal and tympanoplasty of the left ear of a 5-year-old girl (case 1). A, after elevating the tympanomeatal flap, the cholesteatoma behind the corda tympani was visible. Co = cholesteatoma; C = corda tympani nerve; Tm = tympanomeatal flap. B: after drilling out the scutum, the surgeon carefully removed the cholesteatoma. C, the incus was decayed and the stapes could not be identified during surgery. Therefore, the decayed incus was removed. I = decayed incus. D, the residual cholesteatoma at the sinus tympanum and the matrix at the oval window were removed. O = oval window. E, water irrigation of the middle ear. F, identification of the location of the foot plate and facial nerve. Fp = foot plate; Fn = facial nerve. G, the scutum was reconstructed using tragus cartilage. Meanwhile, the ossicle chain was restored using total ossicular replacement prosthesis. T = tragus cartilage; To = TORP. H, replacement of the tympanomeatal flap.

Figure 5. Surgical wound status post TEES or MES. A, left ear of a 5-year-old girl (case 1). The only wound in the inner surface of the tragus was for the collection of graft tissue during TEES. B, the short tragus scar in the right ear of a 9-year-old girl (case 2) after TEES. C, the long retro-auricular scar behind the right ear of a 9-year-old girl (case 2) after MES.
Surgical Technique
The tissue graft was harvested previously from the inner surface of the tragus, including the perichondrium and cartilage, where it left a small, almost invisible wound after the surgery. TEES was initiated with a transmeatal incision from the 6:00 position to the 12:00 position. After elevating the tympanomeatal flap, the scutum was drilled out to expose the attic area. The surgeon dissected carefully along the sac of the cholesteatoma and removed it completely, along with any decayed ossicles. In both cases, the supra-structures of the stapes were absent, the footplate and tympanic portion of the facial nerve were identified, and the residual matrix around the oval window was removed. Water irrigation was critical to ensure all affected areas in the mesotympanum and epitympanum were removed. Subsequently, the attic was reconstructed with a piece of tragus cartilage and the ossicle chain was rebuilt with TORP (Total Ossicular Replacement Prosthesis) (polycel, 4.0 mm height). Finally, the perichondrium graft was placed under the tympanomeatal flap to restore the tympanic membrane and cavity (Figure 4) (Video).
There were no post-operative complications in either case. Both patients had an excellent clinical appearance and experienced significant hearing improvement during the follow-up period (Figure 1B and Figure 2B). Post-operative HRCT was performed 6 months after the surgery, and second-look surgery was conducted 1 year later. No residual or recurrent cholesteatomas were noted in either case, and the TORPs were in the correct location (Figure 3B). With TEES, the only surgical wound was on the inner surface of the tragus, and it was small and very difficult to see (Figure 5).
TEES is particularly valuable for the management of pediatric diseases. The smaller surgical wounds can also decrease the recovery time after surgery, and impose fewer physical and psychological burdens on patients, especially children. Most importantly, most of the healthy structure and mastoid air cells can be preserved, as can the mucosal gas exchange and mastoid buffer, which are crucial for the restoration of the middle ear and the reduction of post-operative morbidity [2,6]. A congenital cholesteatoma, including the surrounding granulation or fibrotic band, was eradicated thoroughly with a high-resolution image and wide surgical view with endoscope assistance. Good Eustachian tube function and mastoid pneumatization can provide better ventilation and prevent recurrence. Healthy mastoid cell preservation is essential for children, but is predicated on the condition that the congenital cholesteatoma is completely removed.
Children may have smaller ear canals than adults. It is not easy to treat a congenital cholesteatoma with a microscope via the trans-canal approach. For some patients, especially those with narrow or tortuous ear canals, it may be difficult for the surgeon to use the retro-auricular approach, and even mastoidectomy, to achieve a sufficient surgical field when treating pediatric cholesteatoma. TEES provides a closer surgical view and an adequate operating space without a large retro-auricular wound and wide-range mastoidectomy [5].
Muaaz et al. also claimed that the duration of endoscopic ear surgery is shorter than traditional microscopic ear surgery. With the endoscopic approach, faster access to pathologic lesions directly through the ear canal without drilling the mastoid cavity may significantly reduce the surgical time [7].
Furthermore, unlike the conventional thought that most congenital cholesteatomas appear in the anterior-superior quadrant, previous reports from Taiwan and Japan suggest that most congenital cholesteatomas appear in the posterior portion of the tympanic cavity [8,9]. These areas may have a number of hidden recess and sophisticated structures, and are difficult to navigate using the microscopic approach. Nevertheless, the TEES can offer a wider field of view to observe the corners of the middle ear, and is helpful in eradicating the lesions in the facial recess and sinus tympanum [2,3].
According to Adrian et al., when compared to microscopic middle ear surgery, endoscopic dissection can reduce the risk of residual disease in the middle ear, including the mesotympanum and retrotympanum [10].
Regarding facial nerve avoidance, the endoscope can provide a high-resolution image to clearly identify the tympanic segment of the facial nerve. The facial recess can be explored easily using an endoscope with an angle view without curetting or drilling the surrounding structure around the facial nerve [7,11]. These advantages of TEES not only reduce the risk of complications, but also guarantee a satisfying outcome.
One-hand manipulation is the most challenging aspect of TEES. Cadaver dissection is helpful to understand the endoscopic anatomy of the middle ear. When performing a dissection, attempts to manipulating a small cotton ball or grain of rice in the middle ear are effective methods to practice endoscope-assisted movement. In addition, clinical training for ear surgery to improve the sensation of the hand to the endoscope view and the tools are essential for surgical practice.
These two cases demonstrated that TEES may be a good alternative to traditional microscopic ear surgery for the management of pediatric congenital cholesteatoma. It can achieve a satisfying outcome, with a lower physical and psychological burden imposed on the pediatric patient. Of course, additional case analyses are still required to confirm the benefits of TEES. We believe that in the near future, along with the evolution and progress of surgical devices, TEES will become less challenging and more prevalent in the treatment of pediatric congenital cholesteatoma.
Received date: May 26, 2017
Accepted date: August 04, 2017
Published date: August 22, 2017
© 2017 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).

Video Transcanal endoscopic ear surgery for congenital cholesteatoma.
Transcanal endoscopic ear surgery (TEES) is an acceptable and safe technique for the exposure and eradication of middle ear and/or attic cholesteatoma, which has been developed rapidly in the past 5 years. TEES is a minimally invasive surgical procedure for middle ear, even inner ear, especially in paediatric patients. After performing TEES, most of the important structures can be preserved, which means a quick recovery after operation. Undoubtedly, TEES is the future of ear surgery. So far, lots of relevant issues have been addressed by many publications. But, there are still many areas of controversy, such as indications and outcomes.
A well-written case report of two children who underwent Trans-Canal Endoscopic Ear Surgery for congenital cholesteatoma. One minor correction to be made.
The revisions made by the author have improved this paper considerably. It can be accepted for publication.
Satisfied with the final version and accepted for publication.
Sun WH, Kuo CL, Huang TC. Transcanal endoscopic ear surgery for congenital cholesteatoma: A preliminary report. Arch Otorhinolaryngol Head Neck Surg 2017;1(2):2. doi:10.24983/scitemed.aohns.2017.00025