Background: Facial air gun injuries can result in destructive wounds and are accompanied by serious damage to the patients. The facial area contains pivotal blood vessels and nerves, which can be associated with significant functions. To date, there is no consensus whether air gun bullets should be removed or left in place; however, the removal of projectiles is generally recommended.
Case presentation: A case of a 16-year-old male Caucasian patient who had experienced an accidental shotgun in the face was presented and discussed. The injury was caused by a loaded air-pressurised weapon. During the initial visit to our department, the pellet was found to be stuck in the pterygopalatine fossa (PPF); however, there were no clinical signs or symptoms such as fistula formation, recurrent infections, or primary haemorrhage. The patient could open his mouth fully without pain and his dental occlusion was normal. Fifteen days later, the patient was readmitted with severe epistaxis. The case was successfully managed by embolization of maxillary artery followed by surgical removal of the bullet that was presented as a foreign body in the PPF on computed tomography (CT) scans.
Conclusion: Air gun injuries have a broad clinical appearance from minor to life-threatening injuries. Modern air gun muzzle velocity can be as high as that of the conventional guns. Therefore, air gun should be considered as a potentially lethal weapon and raising awareness regarding its potential threats is required in order to minimize the air gun injuries.
Gunshot injuries are caused by the action of shooting someone by any form of projectile using any class of firearm. Gunshot incidents take place in a variety of different situations classified into intended (criminal and terrorist attacks), non-intended, or accidental [1]. The degree of injury can range from an insignificant trauma to serious injuries such as stomach and intestinal perforation, cardiac and corneal perforation, liver laceration, hemopneumothorax, and even death [1]. The air gun injuries are mostly accidental and unplanned. Moreover, these weapons can also be used to commit suicide [2].
Based on the velocity of the bullets, two main wounds trauma can be caused: penetrating and non-penetrating or blunt trauma. Penetrating trauma occurs when the bullet penetrates the skin and enters the underlying tissues. This generally creates an open hole or wound. The bullet may remain in the tissue, return via the same pathway, or pass through an exit wound. In the latter case, called perforating injury, the exit wound is generally larger than the entrance wound. In blunt traumas, the skin is not necessarily damaged [3].
Generally, the factors that determine the severity of a gunshot injury are the amount and the efficiency of energy transfer (kinetic energy) from the gun to the bullet [3]. This energy increases with the distance between the weapon and the target as well as the size and shape of the bullet and the gun type. The soft-nosed, rounded, and hollow shape of the pellet could prevent the deep penetrating and reduce the likeliness of exit wounds [4]. Further, factors are related to the patient’s age, tissue composition, and the anatomic portion of the human body.
This case report highlights a very rare case of an accidental air gun injury fired by a friend at a birthday party. The lead pellet was presented as a foreign body in the right pterygopalatine fossa (PPF). Diagnostic and therapeutic strategies are discussed and presented.

Figure 1. Three-dimensional reconstruction from a CT scan showing an air gun pellet in the pterygopalatine fossa (red arrow).
A 16-year-old male patient presented with a complaint of an air gun shot in the right side of his cheek caused by a bullet fired from an air gun with a long barrel. The weapon was fired within 30 cm of the patient’s face. In the initial visit to our department, a minimal wound with a diameter of 1 mm and depth of 2 mm in the right cheek without inflammation or swelling was observed. At that time, the patient had no active bleeding. Computed tomography (CT) showed a foreign body located in the right pterygopalatine fossa (Figure 1 and 2). It was detected that the pellet penetrated through the anterior and posterior wall of the maxillary sinus without any noticeable injury to the blood vessels or nerve damage.
Accordingly, the pellet was not initially surgically removed, and the patient received oral antibiotics without developing further complaints. Fifteen days after the initial trauma, the patient returned to our department with massive nasal bleeding, requiring anterior and posterior nasal packings. Angiography indicated an injury to the right maxillary artery. After embolization, surgical removal of the pellet was conducted via a right-sided transfacial transmaxillary approach to the PPF (Figure 3). The patient was hospitalized for five days without any further complications.
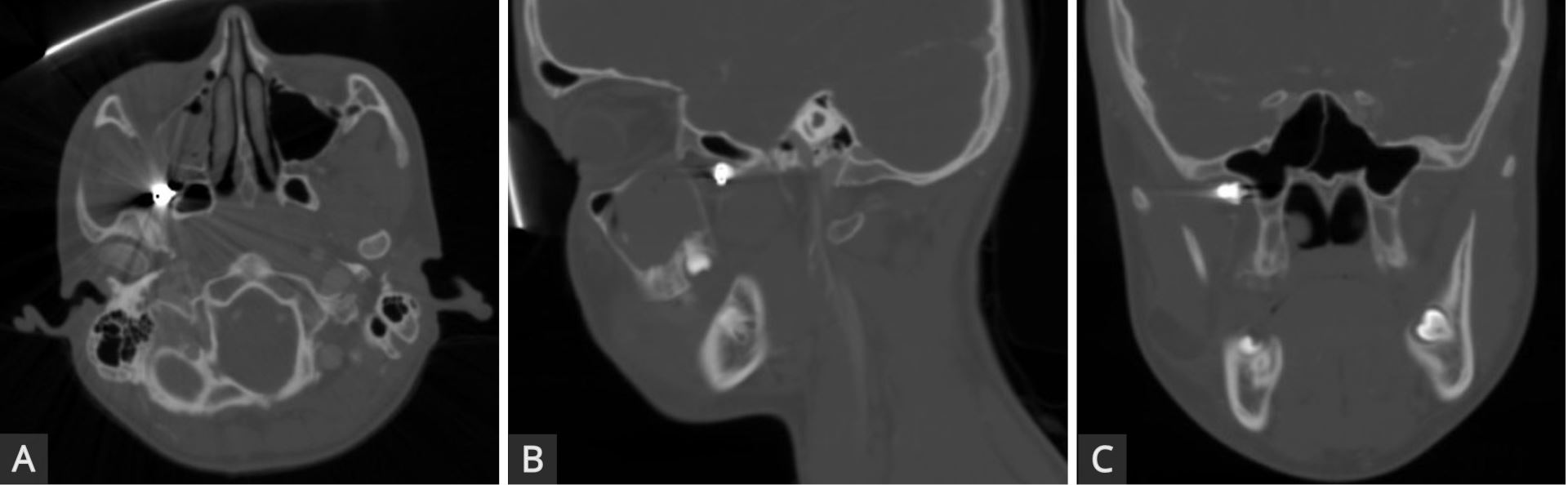
Figure 2. (A) Axial CT scan identifying the foreign body as an air gun pellet in the right pterygopalatine fossa. (B) Sagittal CT scan, transverse view showing that the pellet had penetrated the anterior and posterior wall of the right maxillary sinus with subsequent hematoma. (C) CT scan with a coronal view showing the pellet lodged in the pterygopalatine fossa. Note the minimal bone destruction and the proximity of the pellet to the lateral aspect of the sphenoid sinus.

Figure 3. Severely deformed air gun pellet removed without causing any injury to the adjacent structures.
Accidental gunshot injuries frequently affect children [5]. In a retrospective study reporting on a cohort of 101 children, 81% were male with a median age of 10.9 years. In children, air gun injuries are more serious than those found in adults. Children have thinner bones which are easily traversed by the foreign body [5].
In this case, the embedded pellets in the PPF did not cause any clinical signs or symptoms. No further complaints were stated by the patient in relation to the retained pellet. According to these findings, it was initially suggested that the pellet could be retained, which was in accordance with the findings in the literature.
To date, there is no common consensus on the definitive management of gunshot-injured patients in terms of surgery and reconstruction [6]. The emergency care of firearm injuries to the head and neck must be focused on the basis of resuscitation to restrict any functional or aesthetic damaging [7]. Attention should be given to the condition of airways as bleeding and subsequent swelling can compromise respiratory function [8]. Possible damage to the gunshot-related blood vessels and nerves (such as the maxillary nerve, the pterygopalatine ganglion, and the maxillary artery) needs to be evaluated. Although uncommon, these injuries could cause significant damage to the patient [9].
Head and neck gunshot injuries require a detailed examination including vascular and laryngotracheal areas, inspection for expanding hematomas, active haemorrhage, pulse deficits, neurological deficits, subcutaneous emphysemas, sucking chest wounds, stridor, dyspnoea, hoarseness, dysphonia, or haemoptysis [7]. The easily accessible pellets should be removed surgically by individualized and tailored approaches. Endoscopy techniques cause a low complication rate and are recommended for pallet removal, if feasible [4]. However, if the pellets are located in unfavourable anatomical areas, surgical intervention can result in significant morbidity [7]. Additionally, air gun injuries in the head and neck areas could cause damage to the eyeball, resulting in loss of vision and in some cases even requiring enucleation of the eyeball [10]. The entry of pellet to the cranium may cause intra-cranial bleeding, leak of cerebrospinal fluid (CSF), meningitis, brain abscess, development of traumatic aneurysm, and carotid-cavernous sinus fistulas [7,11].
Due to the relatively short distance of 30 cm, the pellet was able to penetrate through the anterior and posterior wall of the maxillary sinus and was retained in the right pterygopalatine fossa (Figure 2A-C). The proximity to the maxillary nerve, the pterygopalatine ganglion, and the maxillary artery highlighted the potentially endangered adjacent structures. Initially, the pellet’s anatomical localisation and the additional risk of surgery refrained us from removing the pellet, respecting the parental decision. However, selective or emergency angiography as part of management needed to be considered.
Permitting pellets within the body can induce foreign body reaction resulting in delayed severe bleedings from the affected vessels [12]. Generally, metallic pellets are surrounded by a fibrous capsule [13]. Air gun bullets are mainly made of lead, leading to a risk of poisoning [14].
Air gun injuries normally present with a wide variety of clinical forms from minor to life-threatening injuries. The rare case of an air gun pellet retained in the pterygopalatine fossa has the risk of immediate or delayed haemorrhage as illustrated by our patient. Gunshot injuries must be considered as potentially life-threatening and raising awareness regarding its potential threats are required in order to minimize the air gun injuries, especially in children.
Received date: January 01, 2019
Accepted date: February 09, 2019
Published date: February 20, 2019
The authors are grateful to Mrs. Planer from the Department of the Otolaryngology-Head and Neck Surgery, Klinikum Bielefeld, Germany for her support.
This report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors report no financial or other conflict of interest relevant to this article, which is the intellectual property of the authors.
A. Darwish and H. Sudhoff conceived this report, drafted the article, and revised it critically for important intellectual content. L.U. Scholtz and B. Gehl helped to draft the manuscript. All authors read and approved the final manuscript.
The presented case report is in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent for participation was obtained from the patient presented. Since no experimentation with human subjects was performed, no review/approval by an ethics board was required.
© 2019 The Author (s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Darwish A, Scholtz LU, Gehl B, Sudhoff H. An unusual foreign body within the pterygopalatine fossa: A case report. Arch Otorhinolaryngol Head Neck Surg 2019;3(1):3. https://doi.org/10.24983/scitemed.aohns.2019.00100