Objective: The purpose of this study is to determine the utility of radiographic swallow study following a total laryngectomy or total laryngopharyngectomy when evaluating for presence of pharyngocutaneous fistula.
Methods: We performed a retrospective analysis of patients undergoing total laryngectomy and total laryngopharyngectomy at University of Maryland Medical Center between the years of 2009-2014. Patients underwent closure of surgical defect by a variety of methods including primary closure, regional muscle flap, and vascularized soft tissue transfer. The results of the swallow study were identified as being either positive or negative for a fistula. Medical records were reviewed to determine whether or not each patient went on to develop a clinically evident salivary leak.
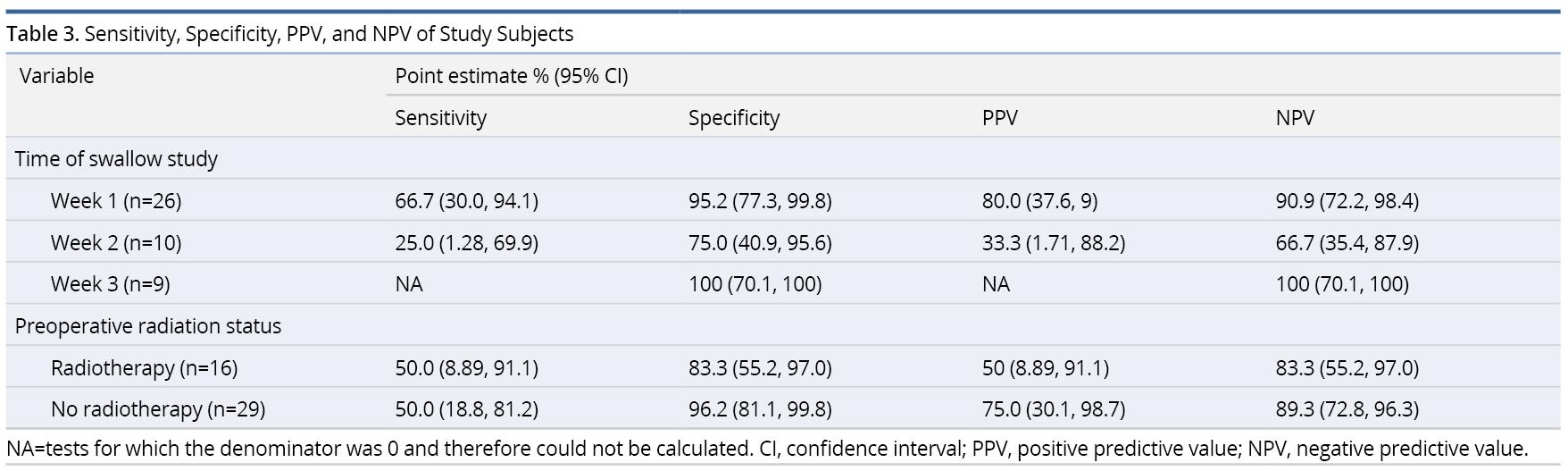
Results: Totally 48 patients were selected for inclusion into the study based on the presence of a swallow study performed at either 1 week, 2 weeks, or 3 weeks post-operatively. Sensitivity and positive predictive value (PPV) were optimized at 1 week, while specificity and negative predictive value (NPV) were optimized at 3 weeks. There was no significant difference between salivary leak rates in radiated versus non-radiated patients or with the various methods of closure. Overall sensitivity of swallow study was found to be 50.0%, specificity was 92.1%. PPV and NPV were 62.5% and 87.5% respectively.
Conclusion: The utility of contrasted swallow studies is limited due to its poor sensitivity, independent of timing. High risk patients may benefit from an extended period of NPO (nil per os; “nothing by mouth”) status, foregoing a contrasted study. Standardization of study protocols and randomized prospective trials will better investigate these issues.
A pharyngocutaneous fistula (PCF) is an abnormal communication between the pharyngeal mucosa and cervical skin. It is one of the most common complications following total laryngectomy (TL) and total laryngopharyngectomy (TLP) and is a cause of significant morbidity and mortality.
The incidence of fistula formation is highly variable, but is generally cited in the range of 10-20% of patients undergoing TL or TLP. It has been reported as high as 65% in high risk patients with risk factors to include malnutrition, diabetes, positive margins, infection, and prior surgery [1,2]. Pre-operative radiation and hypothyroidism have also been found to have significant correlation with fistula formation [3].
Patients who develop a PCF require longer hospital admission, antibiotics and may need additional procedures, which can delay adjuvant therapy [4,5]. These patients can develop life-threatening infections especially in the setting of salivary leak that tracks toward the great vasculature or retropharyngeal space resulting in a risk of carotid blowout and mediastinitis, respectively [6]. Furthermore, measures taken to avoid or treat the development of a PCF may significantly delay a patient’s return to oral feeding [7,8].
The timing of post-operative oral feeding has been highly debated and often dependent on surgeon preference and patient risk factors [9-11]. Many surgeons have adopted the use of contrasted swallow studies to assess for pharyngeal leak prior to oral feeding despite their history of being poorly sensitive [3].
In this study we review our use of barium swallow studies in both primary and salvage TL and TLP patients. We investigate the study’s utility in the evaluation for pharyngeal leak prior to oral feeding with respect to sensitivity and specificity, but with particular attention to timing and the information they provide for clinical decision-making.
The authors performed a retrospective analysis of patients undergoing either primary or salvage TL or TLP at a single tertiary medical center between the years of 2009-2014. Subjects who did not have a post-operative barium swallow evaluation were excluded from the study. Patient information was collected, including age, sex, medical co-morbidities, history of radiation and type of pharyngeal closure. Further details specific to the development of a PCF were recorded for that subset of patients including length of time to fistula, imaging results and management. This study was approved by the Institutional Review Board at the University of Maryland for ethical medical research.
Studies have shown that the majority of fistulae following a TL tend to occur within the first 35 days post-operatively, which is roughly equivalent to 21 days following typical contrasted swallow study [3]. The duration of 21 days was selected to allow for adequate time for the development of a fistula. Leaks that developed beyond this time were felt to be more likely new onset, “late” leaks, rather than fistulae that were missed on initial imaging. There were 2 patients excluded from the results analysis that had negative swallow testing who went on to develop clinical salivary leaks after greater than 1 month following testing.
Chi-square or Fisher Exact tests were used to test the association between categorical variables. The significance level for all tests is 0.05. The results of the swallow study were identified as being either positive or negative for a fistula. Medical records were reviewed to determine whether or not each patient went on to develop a clinically evident salivary leak. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. Results were also stratified based on the presence of preoperative radiation therapy and type of pharyngeal closure. Positive and negative values were defined. True positive indicates a (+) swallow study with clinical evidence of leak within 21 days; false positive indicates a (+) swallow study without clinical evidence of a leak within 21 days; true negative indicates a (-) swallow study without clinical evidence of a leak within 21 days; and false negative indicates a (-) swallow study with clinical evidence of leak within 21 days.
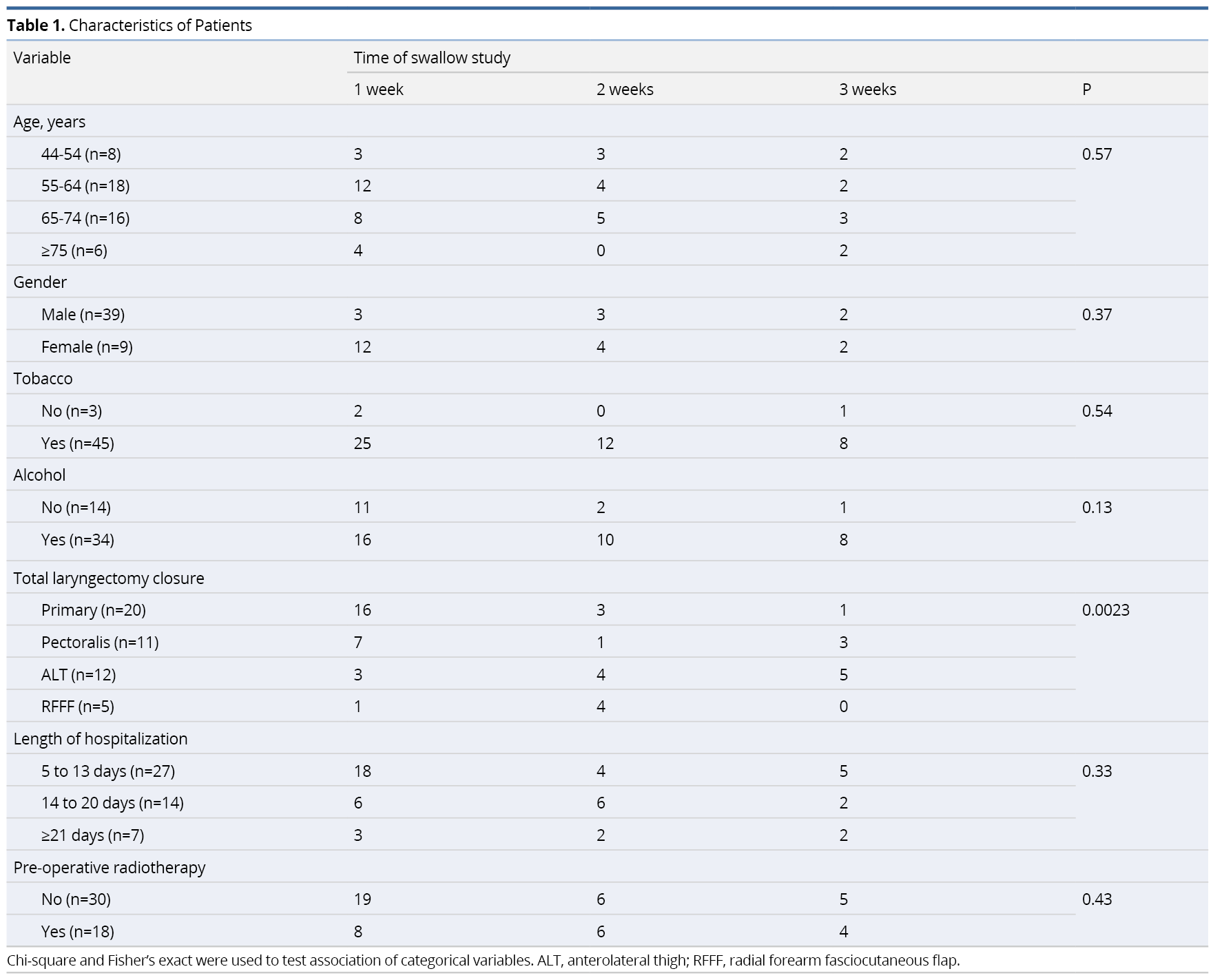
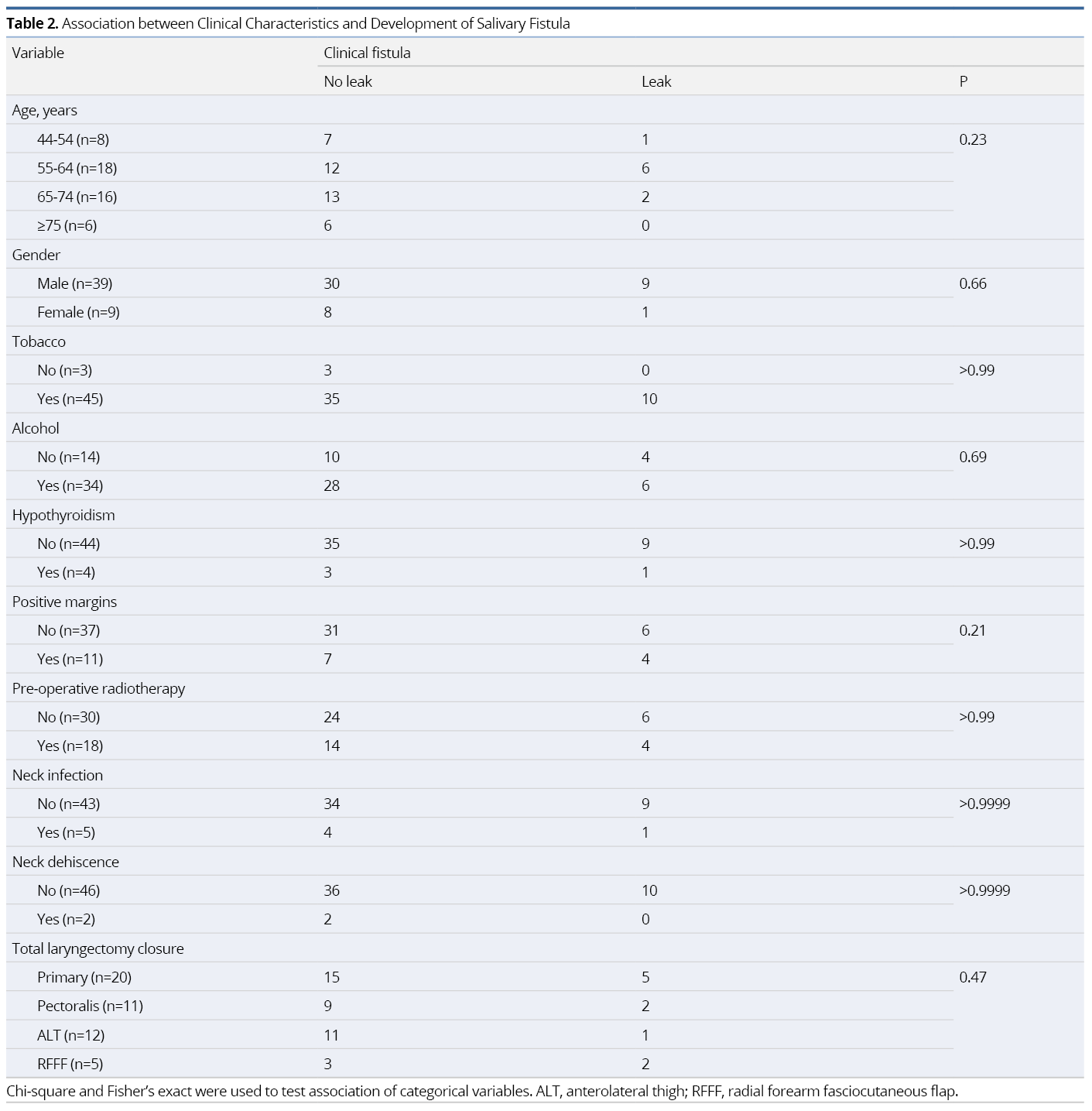
There were 85 patients who underwent TL or TLP at the University of Maryland Medical Center between 2009-2014. After eliminating those patients who did not undergo contrasted swallow study, 48 patients were identified for inclusion into the study. Those patients who did not undergo contrasted swallow study underwent a bedside, clinical swallow assessment, and this was largely based on attending practice and preference. 27 patients had their swallow study performed at 1 week (6-10 days), 12 patients at 2 weeks (11-16 days), and 9 patients at 3 weeks (17-21 days). Of the 48 patients studied, 10 (20.8%) went on to develop a salivary leak as defined by the parameters (true positive or false negative) within this study. There were 39 male (81.3%) and 9 (18.8%) female patients with 93.7% and 72.9% of patients having a history of tobacco use and alcohol use history, respectively. Eighteen patients (37.5%) underwent preoperative radiation therapy (Table 1). There were no statistically significant associations between the development of salivary leak and the presence of clinical patient characteristics (Table 2).
Overall sensitivity of swallow study was found to be 50.0%, specificity was 92.1%. The PPV and NPV were 62.5% and 87.5%, respectively. Performing the study at week 1 appeared to provide the highest sensitivity (66.7%) and PPV (80%). In contrast, performing the study at 3 weeks resulted in the highest specificity (100%) and NPV (100%). Patients without pre-operative radiation appeared to have a superior specificity, PPV and NPV than those with a history of head and neck radiation. Sensitivities were equivalent between the irradiated and non-irradiated groups, at 50% (Table 3).
True Positive (Occult Salivary Leak)
Five patients in our series qualified as true positives. True positives are patients who test radiographically positive for fistula and then go on to develop a salivary leak within 21 days of contrasted swallow study. Occult leaks are a subgroup of true positives, who demonstrate no clinical suspicion of pre-existing leak prior to their swallow study. An additional subset of true positives is those who have clinical suspicion of salivary leak (i.e. neck drainage, saliva within a surgical drain, neck swelling/erythema, clinical evidence of infection) prior to their positive swallow study. In these cases, the swallow study acts as a confirmatory test. There were two patients in the initial dataset who fit the definition of confirmatory true positive; and they were considered true positives for the purposes of statistical analysis.
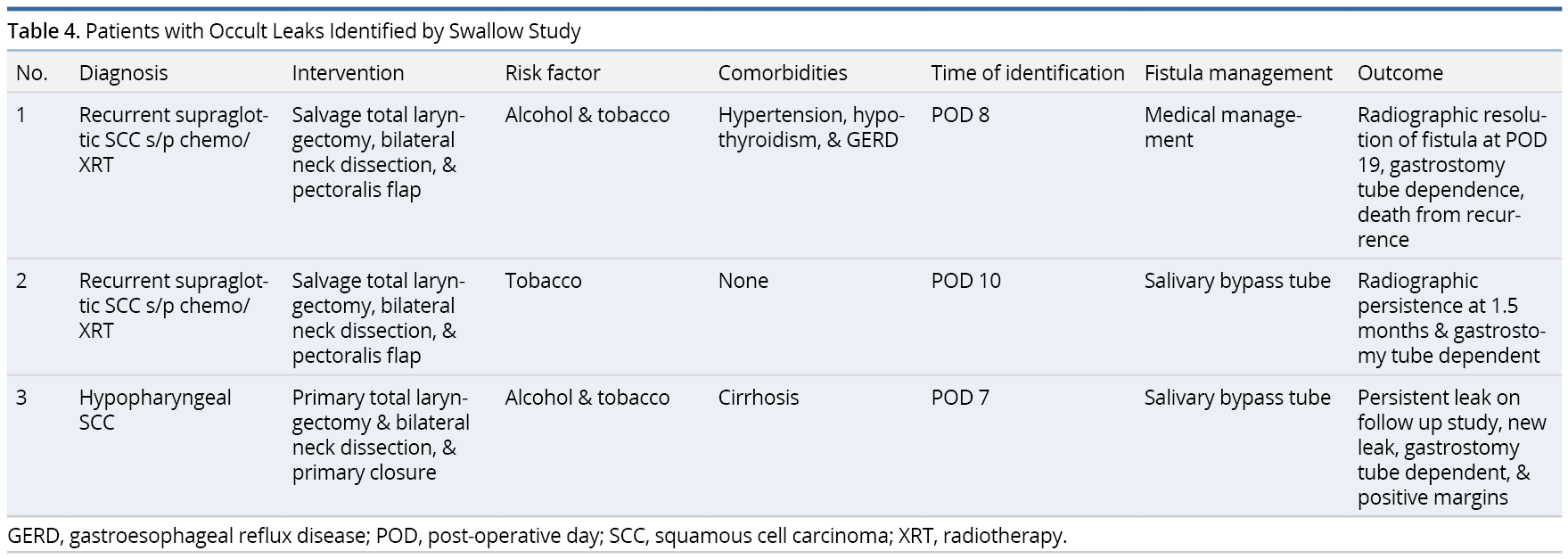
The current study identified three patients with occult leaks that were identified by modified barium swallow (MBS) or esophagram. Patient 1 underwent salvage total laryngectomy after chemo-radiation and reconstruction with a pectoralis flap for recurrent supraglottic cancer. An esophagram on post-operative day (POD) 10 identified a salivary leak, and this was managed with a salivary bypass tube. Patient 2 underwent salvage TL and pectoralis flap after chemoradiation failure. An esophagram on POD 8 identified a leak, which was managed conservatively with antibiotics. Patient 3 underwent TLP with primary closure for hypopharyngeal cancer. An esophagram on POD 7 identified a leak that what managed with salivary bypass tube and cauterization (Table 4).
False Negative
False negatives include patients who develop leaks after negative imaging. Five patients in our study were analyzed as false negatives. There were four (4/48, 84%) patients who tested negative for fistula, but who then went on to develop a salivary leak after initiation of an oral diet. Two of these patients tested negative at 1 week, but presented with a clinical leak on POD 12, and POD 17 respectively. The third patient tested negative at 2 weeks, and subsequently presented with a clinical leak on POD 21. One patient out of the five totals was considered a false negative by confirmatory testing, i.e. he developed clinical evidence of a leak, but went on to have a negative swallow study at POD 7.
False Positive
Three patients tested positive radiographically but did not ever develop clinical evidence of a leak. In all three cases radiographic swallow evaluation was performed either at 1 week or 2 weeks post-operatively and demonstrated a focal outpouching or small tracheoesophageal fistula. Reconstruction in each of these cases consisted of either pectoralis major rotational flap or anterolateral thigh microvascular free flap. Conservative management included continuation of nasogastric or gastrostomy tube feeding with a short course of antibiotic. As previously stated, each of these three patients never developed clinical evidence of a pharyngeal leak on subsequent exam.
Time to Salivary Leak and Previous Radiation Exposure
Of the 10 patients who developed salivary leaks or early fistula, four (40%) occurred in those patients who were previously treated with radiotherapy with an average time for salivary leak of 14.755 days as compared to 12.8 days in the non-radiated group (P=0.78).
Development of a PCF is one of the most common complications after a TL or TLP [12]. It can be devastating to the patient, family, and health care system. Many patients will require prolonged hospitalization, antibiotics, or additional procedures ranging from simple wound care, placement of a salivary bypass tube to more invasive surgical procedures such as closure of the defect by regional or free tissue transfer. Moreover, management of this complication can delay adjuvant therapy [5].
Determining when to initiate an oral diet in the post-operative period is an important and difficult decision. For obvious reasons, early initiation of oral feeding is the preferred method of nutrition by both the patient and surgical team, but is often outweighed by the risk of potentiating a salivary leak [13]. Currently there are no universal protocols or guidelines for initiating oral feeds following TL or TLP.
For primary TL or TLP patients, many surgeons will allow one week for neo-pharyngeal healing prior to starting a clear liquid diet [14]. Patients with significant risk factors may necessitate a more conservative approach of waiting several weeks [9]. Some institutions choose to maintain all patients on nasogastric/gastrostomy tube feeding for a minimum of two weeks, very often necessitating hospital discharge with some form of alternative feeding method [15]. Suslu et al. reported a rate of PCF of 12% and found this rate to be the same in patients who were fed orally within three days of surgery or after three days [16]. Eustaquio demonstrated similar findings in irradiated patients who were status post salvage total laryngectomy [17].
Historically, the method of evaluation of post-operative pharyngeal leak has been largely surgeon dependent. Many surgeons will reflexively order a barium swallow in order to rule out a salivary leak with intention for earlier feeding. Despite the popularity of the MBS and its high specificity, a negative swallow study can be falsely reassuring as the reported sensitivity of this study has been suboptimal with sensitivity rates as low as 15-70% [18,19].
A majority of literature on leak detection arises from evaluation of esophageal and gastric anastomotic procedures and their outcomes. Reported sensitivities and specificities of contrasted studies in these patients are consistent with those found in TL/TLP patients [20]. Regardless of the anatomic location or surgery, the evolution of fistula formation and complexity of TL/TLP patients must be fully understood in order to accurately interpret the contrast study.
Patients can frequently develop a pharyngocutaneous leak despite a negative barium swallow study. It is often difficult to determine; however, whether a negative study is secondary to a pre-existing leak not identified on the study (i.e., a true false negative) or a de novo leak caused by initiation of oral feeding following an initial negative study. In either scenario it is important to understand that a swallow study only captures one moment in this process that can evolve over a course of a week or more. Determination of when to perform the study can be difficult for this reason. In our study, sensitivity and PPV were optimized at 1 week, while specificity and NPV were optimized at 3 weeks.
The maximum utility of a post-operative barium swallow occurs when the study identifies an occult leak and subsequently changes management. We identified six patients with subclinical fistulas found on barium swallow studies. All six patients were treated conservatively including antibiotics, wound care and tube feeding. Three of these patients never developed clinical signs of a leak. Three patients received prior chemotherapy and radiation. Seven patients developed early signs of PCF and were treated regardless of swallow study results.
Barium swallow studies are highly specific and excellent for confirming the presence of a pharyngeal leak. In our review we found it difficult to differentiate a false positive from a true positive that was adequately treated. For this reason, there were no false positives reported unless there was radiographic evidence confirming a false read (i.e., Surgical clip or drain). Depending on how prior studies interpreted this data, the reported specificities and positive predicted values may be overestimated. We also found that many patients will often develop a clinical leak as their first presentation regardless of swallow study results. Regardless, barium swallows can offer important information regarding the location and size of the fistula. Krouse et al reported that fistulas greater than 2 cm on radiograph may predict evolution of a subclinical tract to fully manifest itself [21].
Standardized imaging protocols should be instituted to reduce variability in performing and interpreting radiographs amongst different institutions. We propose a universal TL protocol. This framework would ideally include a radiologist and speech language pathologist highly familiarized with the altered anatomy post laryngectomy. Inclusion of the speech language pathologist may not be necessary in identifying leak, but rather to provide guidance on swallowing strategies and anticipated timeframe for diet advancement, and to identify other factors that may contribute to post-surgical dysphagia. The patient would consume 1 cc, 3 cc and 10 cc of water-soluble contrast in lateral and AP views. Oblique view may be utilized if there is limited exposure due to body habitus or post-surgical edema. If no leak is identified, the patient should trial serial swallows of thin contrast. If material clears adequately from the pharynx, two 3 cc boluses of barium puree may be trialed. These therapeutic trials are not to put undue stress on the suture line, but rather to provide a thorough examination and guidance for future diet planning. The exam should be focused on the cervical esophagus with at least one screen of the complete esophagus. Motility, the presence of narrowing, and pharyngoesophageal bolus clearance should be detailed in the report.
Rosenthal et al. found that the sensitivity of the barium esophagram at their institution was found to be 26%, with a specificity of 94%. The sensitivity of the study in primary laryngectomy patients only was much higher at 55%, with a specificity of 97%. In contrast, the sensitivity in salvage patients was 14%, with a specificity of 91% [3].
The validity of the definitions used in this study are, in some ways, limited. As other authors have shown, fistulas up to a certain size can often be managed successfully without surgical intervention [21]. Therefore, false positives may represent a limitation of the swallow study, but they may also represent what amounts to an adequately treated fistula. However, stratifying between those who were treated adequately versus true false positives would require delaying treatment on a patient with a potential fistula, an intervention which was not incorporated into this retrospective study.
In general, timing of swallow study at our institution is attending dependent and dependent on patient risk factors. Those at high risk for developing salivary leaks often have swallow studies delayed beyond the first week. The same is true for those patients with other complicating factors, such as concomitant bulky oral cavity flaps that may limit the oral phase of swallowing, or patients who are otherwise too medically sick for initiation of a diet. It is not the practice at our institution to perform confirmatory barium swallow testing, although follow up studies are often performed to confirm resolution of a leak, or to diagnose a leak in a patient with subtle signs of a leak such as neck erythema, without frank drainage of saliva from the neck.
There are several additional limitations to our study. The most significant relates to the retrospective nature of the investigation, which does introduce a selection bias. We only included those patients from our institution with a complete medical record, and, therefore, several patients with missing data (such as no barium swallow study) were excluded. In addition, swallow studies were interpreted by several different radiologists, all of whom may have different thresholds for radiographically diagnosing pharyngocutaneous fistulae. Another limitation to our study, which follows its retrospective nature, is that it was not randomized by type of reconstruction. There is a tendency at our institution for those patient’s with free flap reconstruction to undergo delayed swallow study, and this tendency may influence our results. Despite the above limitations, we feel our results provide valuable information regarding the strengths and pitfalls of contrasted swallow studies and when they are most useful following total laryngectomy.
The development of PCF is a multi-factorial process which is hard to predict. The utility of contrasted swallow studies is limited due to its poor ability to detect a subclinical leak, independent of timing. High risk patients may benefit from an extended period of tube feeding as they tend to have delayed leaks. Patients at low risk may benefit from early oral feeding and forego the use of a contrasted study. In select patients, the contrasted study may offer valuable information regarding location and size of a fistula that may help with management. Standardization of study protocols and randomized prospective trials will better investigate these issues.
Received date: October 27, 2019
Accepted date: January 13, 2020
Published date: July 22, 2020
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors report no financial or other conflict of interest relevant to this article, which is the intellectual property of the authors.
© 2020 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Amin J, Ortlip TE, Cohen D, Vakharia K, Lubek JE. The utility of barium swallow studies for evaluation of pharyngocutaneous fistula after total laryngectomy. Arch Otorhinolaryngol Head Neck Surg 2020;4(2):4. https://doi.org/10.24983/scitemed.aohns.2020.00133