Refluxing does not stop at the esophagus. The gastric acid continues upwards to the pharynx, larynx, oral cavity, and nasal cavity. In histology, mucosal changes associated with acid have been confirmed. Previous research has shown that the long-term corrosion of mucosal regions in the head and neck such as the pharynx and larynx would increase the risk of cancerous lesions. Establishing a relationship between a benign disorder (i.e., acid reflux disorders) and a malignant disease (i.e., oropharyngeal, hypopharyngeal, or laryngeal cancers) has a certain influence on clinical practice. Clinicians need to remain vigilant with patients with acid reflux disorders and rule out the possibility and presence of head and neck cancer although co-existence does not necessarily mean that a causal relationship exists.
Nowadays, people’s daily routines are becoming increasingly irregular, particularly when it comes to eating and drinking. For example, people need to cope with pressures at work and rely on coffee to get them through the day. Some people even drink coffee as they would water, which could lead to heartburn in the long term. As the esophagus is unable withstand gastric acid like the stomach wall can, persistent exposure to gastric acid may corrode the esophagus. Previous studies have found that long-term corrosion of the esophagus by gastric acid could result in esophageal cancer [1].
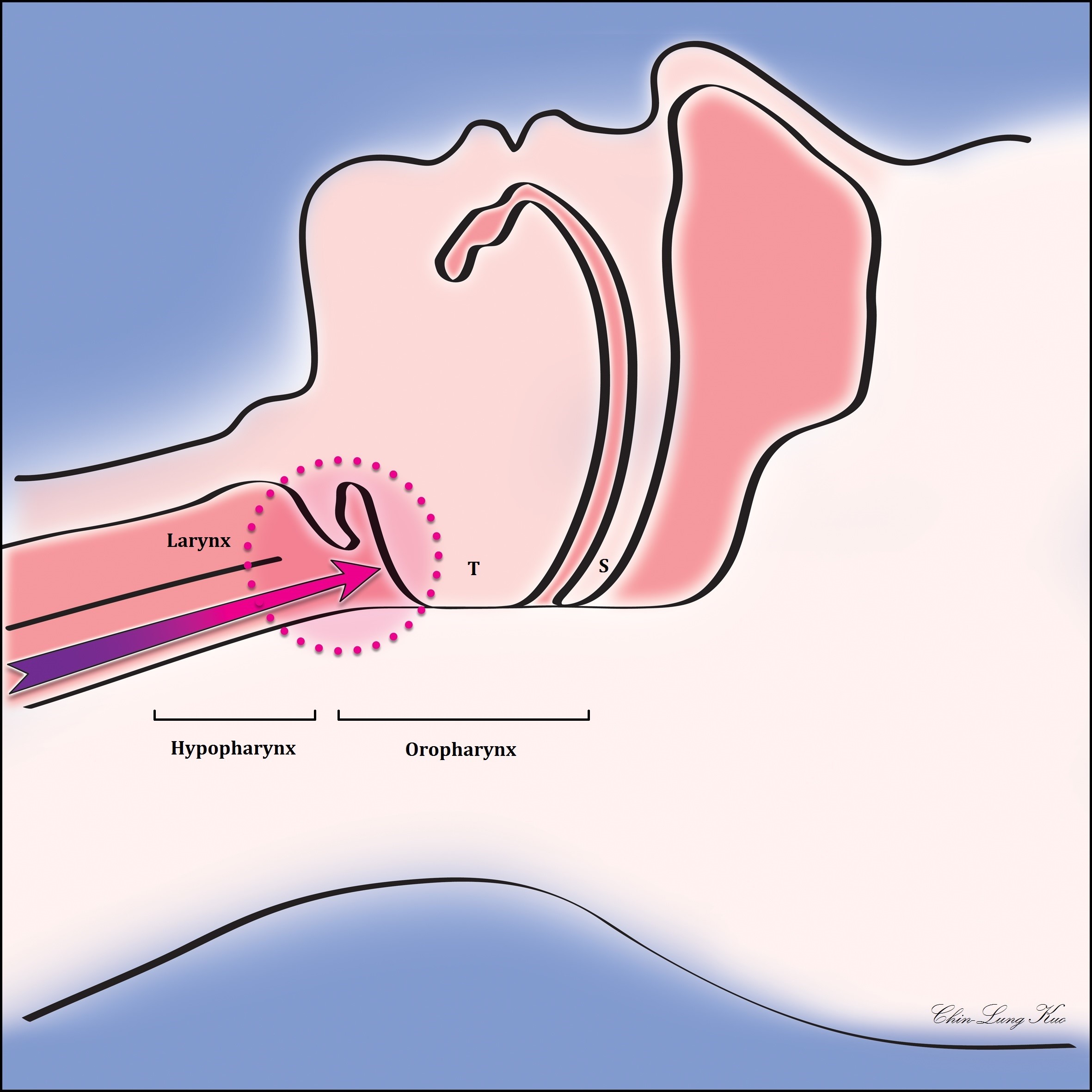
Refluxing, though, does not stop at the esophagus (Figure 1); the gastric acid continues upwards to the pharynx, larynx, oral cavity, and nasal cavity, which can cause certain discomfort, such as a foreign body sensation in the throat, difficulties swallowing, and hoarseness after awakening. The author has had several patients who have come to the clinic complaining about an inability to cough out phlegm in their throat, no matter what they do. For some relief, they constantly clear their throat, but this relief is only temporary. An otolaryngoscopic examination would show that their laryngeal mucosa has become extremely swollen due to gastric acid burn. Other patients have complained about coughing for months. Yet, chest X-rays and visits to pulmonologists would show nothing remarkable.
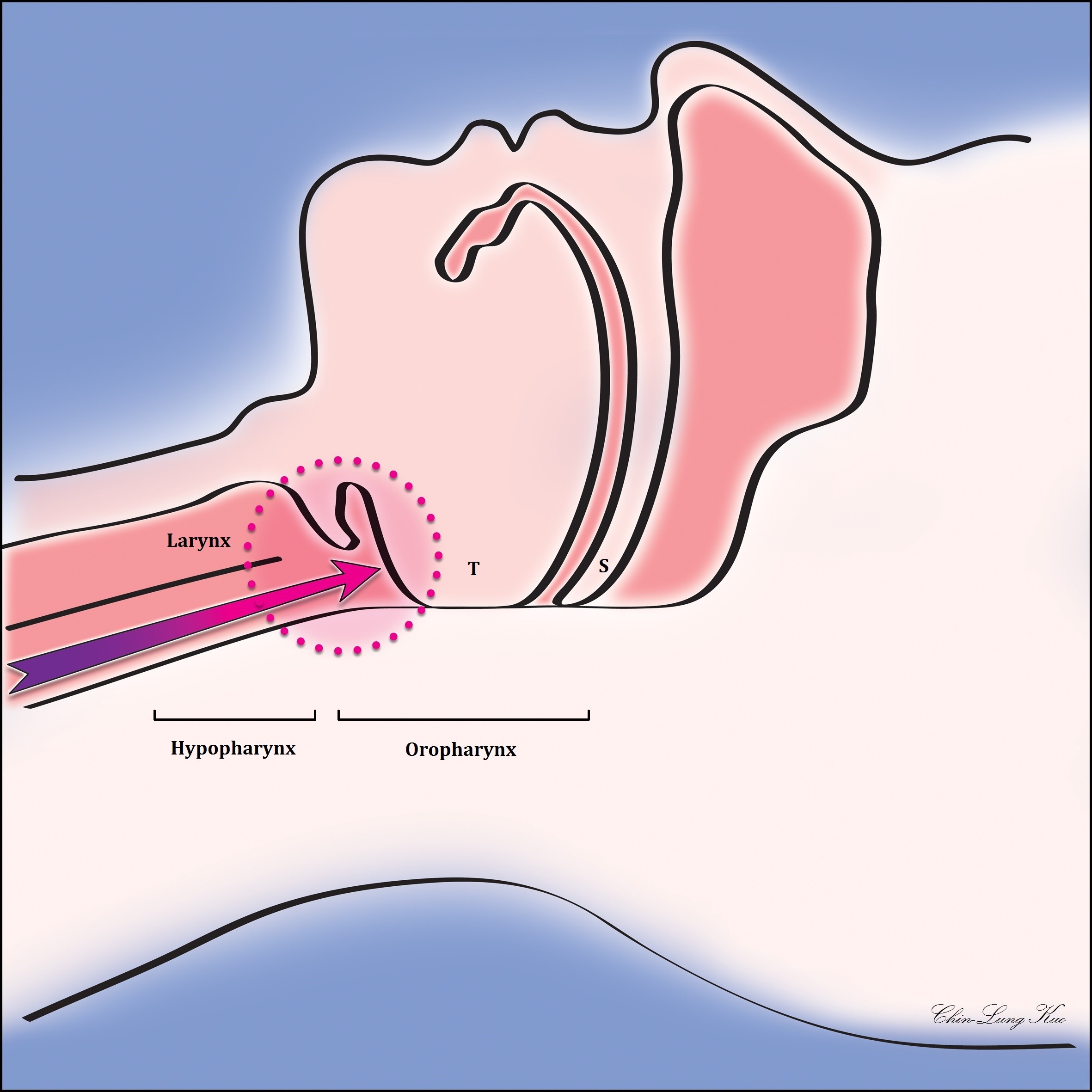
Figure 1. Possible mechanisms of gastric acid-induced hypopharyngeal and oropharyngeal cancer. When sleeping on your back, gastric acid is prevented from flowing up to the oral cavity, nasal cavity, and nasopharynx due to the tongue touching the oropharynx; however, the gastric acid remains in the oropharynx and hypopharynx. After 7-8 hours of sleep, the oropharynx and hypopharynx may become extremely irritated. In the long term, this may increase the chances of oropharyngeal and hypopharyngeal cancers. (T represents the tongue, and S indicates the soft palate)
When the author tells patients that the cause of their discomfort may be acid reflux, 6 out of 10 patients would say, “But I don't have acid reflux!” or “Doctor, you must be wrong! I just had a gastroscopy last month and the gastroenterologist said I was fine!” Indeed, otolaryngologists and gastroenterologists may differ in the management of the acid reflux related disorders [2,3]. The fact is that the patients may have laryngopharyngeal reflux (LPR) rather than gastroesophageal reflux disease (GERD). In GERD, the reflux of gastric contents is limited to the esophagus. In LPR, the reflux of gastric content affects the larynx and pharynx. Despite occasional cross-diagnoses of GERD and LPR, there are essential differences. GERD is accompanied by acidity and heartburn (retrosternal burning), which is rarely encountered in LPR patients. In GERD, reflux and acidity typically occur during the night (nocturnal refluxers). In LPR, reflux typically occurs during the day (daytime refluxers). LPR symptoms occur when patients are in an upright position during periods of physical exertion (e.g., bending over, Valsalva, and exercise), whereas GERD reflux occurs while patients are lying down [4].
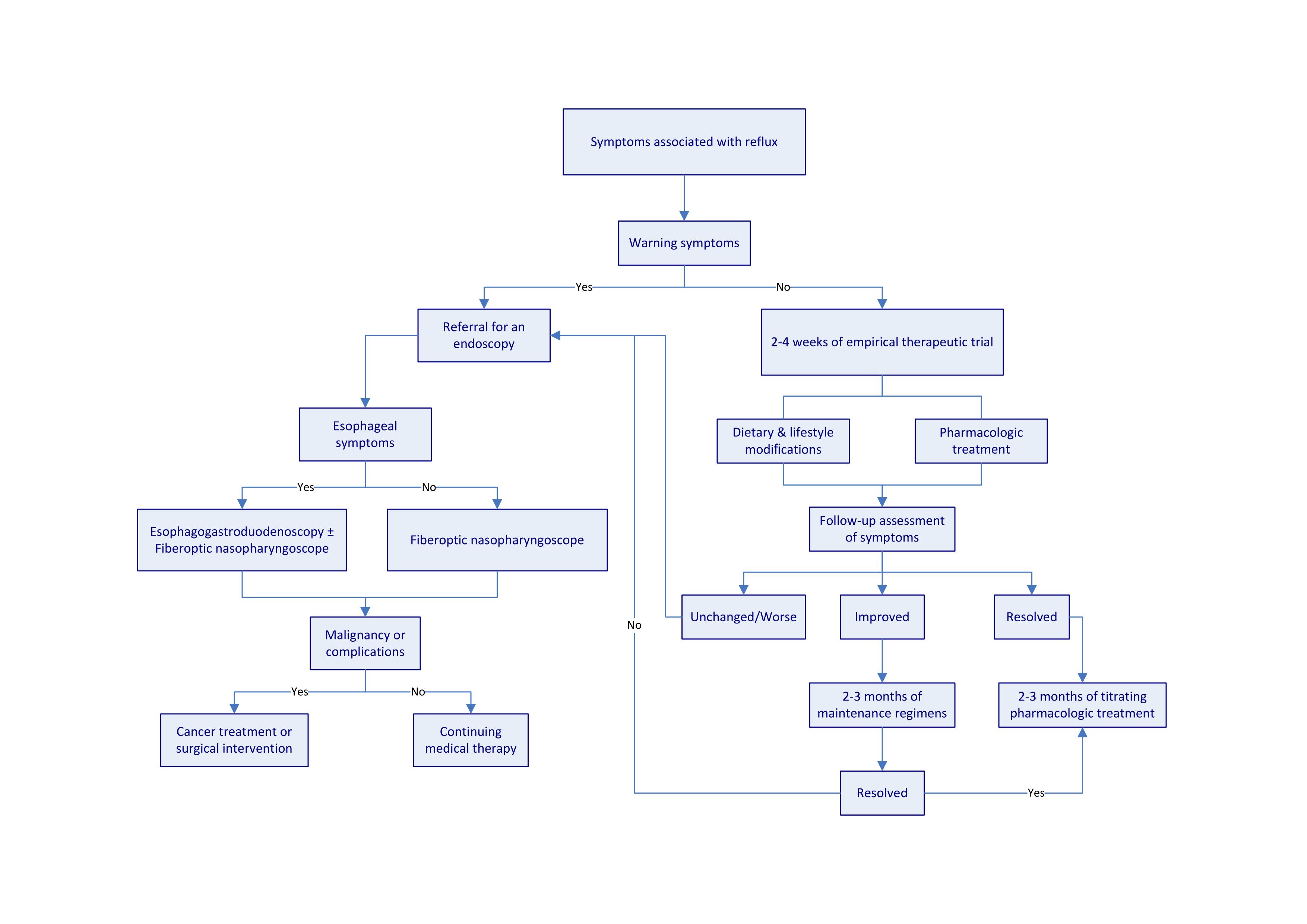
The author developed the algorithm shown in Figure 2, with the aim of streamlining the assessment and management of reflux disorders, including LPR and GERD [4]. The mainstay of medical treatment for acid related disorders includes H2-receptor antagonists and proton pump inhibitors. Prokinetic agents and mucosal cytoprotectants (e.g., sucralfate) may provide additional benefits. As there is nothing the author can say to the above-mentioned responses of the patients except, “Take my prescription for two weeks, and then let's see,” the author requests that they refrain from drinking coffee and tea, and eating spicy and sweet foods. More importantly, they should avoid lying down within two hours of eating (for instance, some people lie down for a nap after lunch, and some eat a midnight snack before bed) because the stomach needs two hours to empty food after meals. Once the stomach is empty, it secretes less acid, all of which reduces the pressure in the stomach and decreases the likelihood of gastric acid flowing up the esophagus, pharynx, larynx, oral cavity, and nasal cavity. After the patients have taken the “wonder drug” for two weeks, over half say that their symptoms have improved.
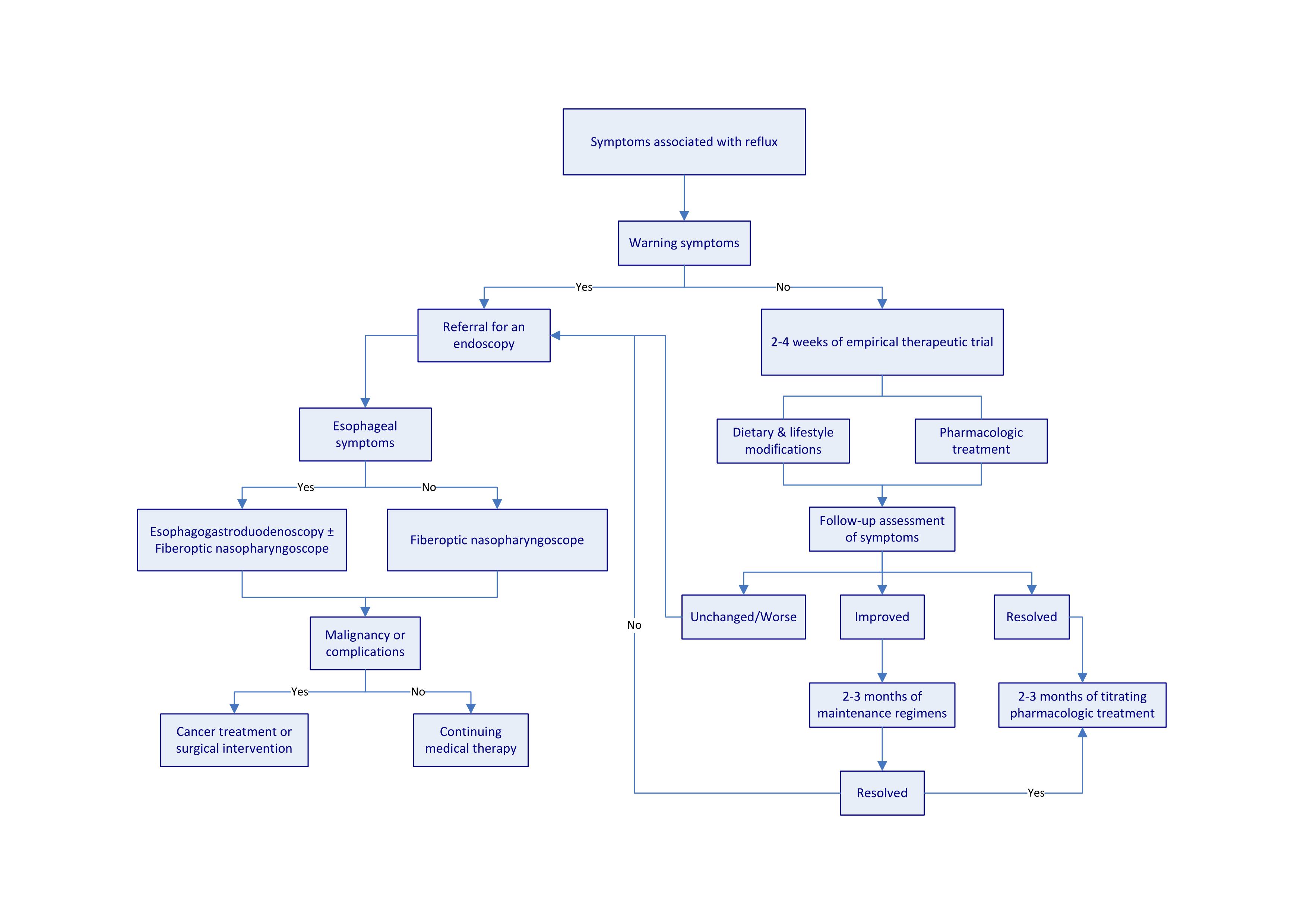
Figure 2. Algorithm for assessment and management of reflux disease. Warning symptoms include dysphagia and chest pain. These symptoms are suggestive of complications or malignancies. Patients with these symptoms require a referral to specialists for an endoscopic examination. Chest X-rays may be required to exclude the possibility of lung disorders for patients presenting with chronic cough.
Although many people know of acid reflux, few know that gastric acid can reach the oropharynx, larynx, oral cavity, and nasal cavity. This condition is called LPR and its symptoms are slightly different from those of GERD, which is more commonly known as acid reflux [5]. This is why some patients do not have GERD symptoms, such as heartburn, but have LPR symptoms, such as a foreign body sensation in the throat, difficulties swallowing, hoarseness after awakening, and a chronic dry cough of unknown origin [6].
Even though LPR and GERD have slightly different symptoms, the pathological mechanisms are similar; both involve gastric acid burning the mucosa of the upper aerodigestive tract. In histology, mucosal changes associated with acid have been confirmed [7]. It is therefore reasonable to assume that if gastric acid corroding the esophagus for a long period of time may cause esophageal cancer [1], then the long-term corrosion of mucosal regions in the head and neck such as the pharynx, larynx, oral cavity, and nasal cavity would also increase the risk of cancerous lesions.
Prior research examined the effects of reflux disease on the laryngeal mucosa, and the results showed an association between acid reflux and carcinoma of the larynx [8-11]. However, there is a paucity of literature examining the effects of reflux disease on the pharyngeal mucosa while controlling for covariates. Hence, the author used the National Health Insurance (NHI) database in Taiwan to analyze the medical information from a million individuals from 1998 to 2010. From the data, the author found nearly 40,000 adults (39,845 adults over the age of 20) diagnosed with GERD and compared the probability of these patients contracting head and neck cancer with that of the general population using the standardized incidence ratio [12].
The results showed that patients that had been diagnosed with GERD were 1.59 times more likely to develop head and neck cancer than the general population (p<0.001). In terms of gender, males diagnosed with GERD were 1.70 times more likely to develop head and neck cancer than males in the general population (p<0.001). With respect to age, patients under the age of 60 diagnosed with GERD were 1.06 to 3.03 times more likely to develop head and neck cancer than general individuals under the age of 60 (p<0.01). Finally, in terms of tumor type, patients that had been diagnosed with GERD were a respective 3.96 times and 3.58 times more likely to develop hypopharyngeal cancer and oropharyngeal cancer than the general population (p<0.001). These results obtained from the NHI database of Taiwan form the first population-based epidemiological evidence analyzing the relationship between acid reflux and the laryngopharyngeal cancers.
In this era that emphasizes big data, the advantage of large databases is that they have relatively higher statistical validity. An increasingly popular research model in medicine is to analyze big data and use the power of data to create application value. Despite the inherent advantage of high validity, large databases also have limitations. Although our study found that patients diagnosed with GERD have a statistically higher chance of developing subsequent head and neck cancer, we still could not prove a causal relationship between GERD and head and neck cancer. Previous research has established that smoking and drinking alcohol are all risk factors in GERD and head and neck cancer. Unfortunately, the NHI database does not include details regarding these two risk factors; therefore, we must exercise caution in this correlation between GERD and head and neck cancer. Many of the patients in our study possibly smoked or drank alcohol, which could have caused their incidence ratios of GERD and head and neck cancer to be higher than those of the general population.
Nevertheless, establishing a relationship between a benign disorder (i.e., acid reflux disorders) and a malignant disease (i.e., oropharyngeal, hypopharyngeal, or laryngeal cancers) still has a certain influence on clinical practice [11-14]. Clinicians need to remain vigilant with patients with acid reflux disorders and rule out the possibility and presence of head and neck cancer although co-existence does not necessarily mean that a causal relationship exists. If such patients have persistent laryngopharyngeal symptoms, such as a sore throat, difficulties swallowing, tightness in the throat, a foreign body sensation in the throat, a chronic cough, hoarseness after awakening, or a constant need to clear their throat, then clinicians should consider the possibility of oropharyngeal and hypopharyngeal cancer being present and refer the patients to an otolaryngologist for a detailed otolaryngoscopic examination.
Received date: January 07, 2020
Accepted date: February 05, 2020
Published date: February 19, 2020
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This study was sponsored by grants from Medical Affairs Bureau Ministry of National Defense (MAB-107-099) and Taoyuan Armed Forces General Hospital (AFTYGH No. 10507, AFTYGH No. 10626, and AFTYGH No. 10734).
The author reports no financial or other conflict of interest relevant to this article, which is the intellectual property of the author.
© 2020 The Author. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Using a safe and controlled simulation environment, authors develop an effective and realistic oropharyngeal bleeding mass scenario that was well received by participants in preparing them for real life scenarios.
Dysphagia is an important consequence of cancer treatment and has overarching implications on quality of life. Using the FOIS, we demonstrated that swallowing function may be worse in the long term in patients with OPSCC undergoing triple therapy, although this finding did not reach statistical significance. This study emphasizes the importance of diligent selection in patients undergoing TORS to avoid poor functional swallowing outcomes, particularly in those that may need adjuvant chemoradiation therapy. A study with a larger sample size may determine the significance of these trends.
Kuo CL. Acid reflux increases susceptibility to laryngopharyngeal and oropharyngeal cancers. Arch Otorhinolaryngol Head Neck Surg 2020;4(1):2. https://doi.org/10.24983/scitemed.aohns.2020.00123