The sinonasal region is frequently associated with malignancies, but adenocarcinomas are extremely rare, especially the non-intestinal type. The symptoms of a disease are usually non-specific, making a diagnosis difficult until the disease has reached a late stage. Radiographic studies are essential for determining the stage of the disease and planning the surgical procedure. The endonasal surgical approach has gained popularity in recent years. This case report describes the case of a 49-year-old male who suffered from left nasal obstruction, headaches, recurrent epistaxis, low visual acuity, and proptosis. A magnetic resonance image revealed a contrast-enhancing bulky lesion that occupied the left sinonasal cavity up to the level of the choana. The patient was subjected to an endoscopic procedure employing a centripetal technique, which allowed the medial wall of the orbit and the anterior base of the skull to be preserved while the tumor was completely removed. Upon review of the pathology report, the tumor was identified as a high grade non-intestinal adenocarcinoma. Tumors of this type are more common in men and can affect anyone from teenagers to older adults. A nasal obstruction is the most common symptom, but swelling and facial deformity may also be present. This tumor is characterized by a solid pattern and is an invasive cancer that has an aggressive nature. The level of pleomorphism is moderate to severe, with a high mitotic index and atypical mitoses as well as necrosis. There is CK7 positivity in the immunohistochemistry pattern, while CK20 and CDX-2 are negative. The diagnosis poses a number of challenges. An immunohistochemical study and a histological examination are essential in order to confirm these findings. An accurate classification of the disease is critical for determining its prognosis.
There is a variety of tumors commonly occurring in the sinonasal region; however, it is rare for adenocarcinomas to develop there. Sinonasal adenocarcinomas can be divided into salivary-type and non-salivary-type adenocarcinomas. The latter are further classified into two types of adenocarcinomas, namely intestinal and non-intestinal types. Sinonasal adenocarcinomas of the non-salivary type are rare cancers. They are believed to account for only 13% of all reported cases of sinonasal carcinoma [1-3].
The classification of adenocarcinoma is extremely critical since it determines both the behavior of the tumor as well as the prognosis of the patient. Observations have shown that patients suffering from low-grade adenocarcinomas experience longer-lasting symptoms, have less pain, and are not affected by deformities. A high-grade lesion, on the other hand, has more extensive involvement of the paranasal sinuses, which indicates that the tumor is more invasive [4].
Usually, sinonasal adenocarcinomas are diagnosed late in the disease process, when the disease has already advanced. This is due to the aggressive nature of the disease and its uncertain clinical status. As a result, imaging examinations are an essential part of the diagnostic process, as they provide additional information regarding the staging and planning of surgical procedures [5].
The surgical approach aims to completely and carefully remove the entire lesion in order to ensure a successful outcome. The surgery can be performed through a variety of external approaches, but endoscopic surgery has gained special prominence in many centers in recent years because of its similar oncological results, lower incidences of complications, and lower mortality rates compared to other surgical procedures [5-7]. Radiotherapy is primarily used as a palliative or complementary treatment for cancer in the post-operative period [5,8]. In spite of its positive effects, chemotherapy has lost favor due to its poor reproducibility of therapeutic effects, which has contributed to its decline in popularity. It is evident that surgery is the most beneficial treatment option, regardless of whether it is combined with radiotherapy or used alone [5]. Adjuvant radiotherapy is recommended for high-grade tumors and tumors with a T3 or T4 stage [9].
Although the patient suffered from an extremely aggressive and rare condition, there was a successful outcome in this case. In light of this, it is likely that a well-performed surgery resulting in the complete removal of the lesion, as in this case, will lead to a satisfactory outcome. It has been noted in the literature that there are several knowledge gaps concerning cases similar to this. In an effort to fill some of those gaps, we present this case to provide some insight into these types of cases.
A 49-year-old male presented to the clinical office three months ago with left nasal obstruction, headaches, recurrent epistaxis, decreased visual acuity, and ipsilateral orbital cellulitis. A physical examination revealed that he had proptosis as well as a friable vegetative lesion that had obliterated the left nasal cavity. A magnetic resonance imaging of the paranasal sinuses (Figure 1A) revealed that a massive expansive lesion had occupied the left nasal cavity up to the level of the choanae, measuring 9.0 x 4.8 x 2.1 cm and displaying contrast enhancement. We decided not to perform an initial biopsy prior to surgery due to the high risk of bleeding and the intention to resect the lesion en bloc.
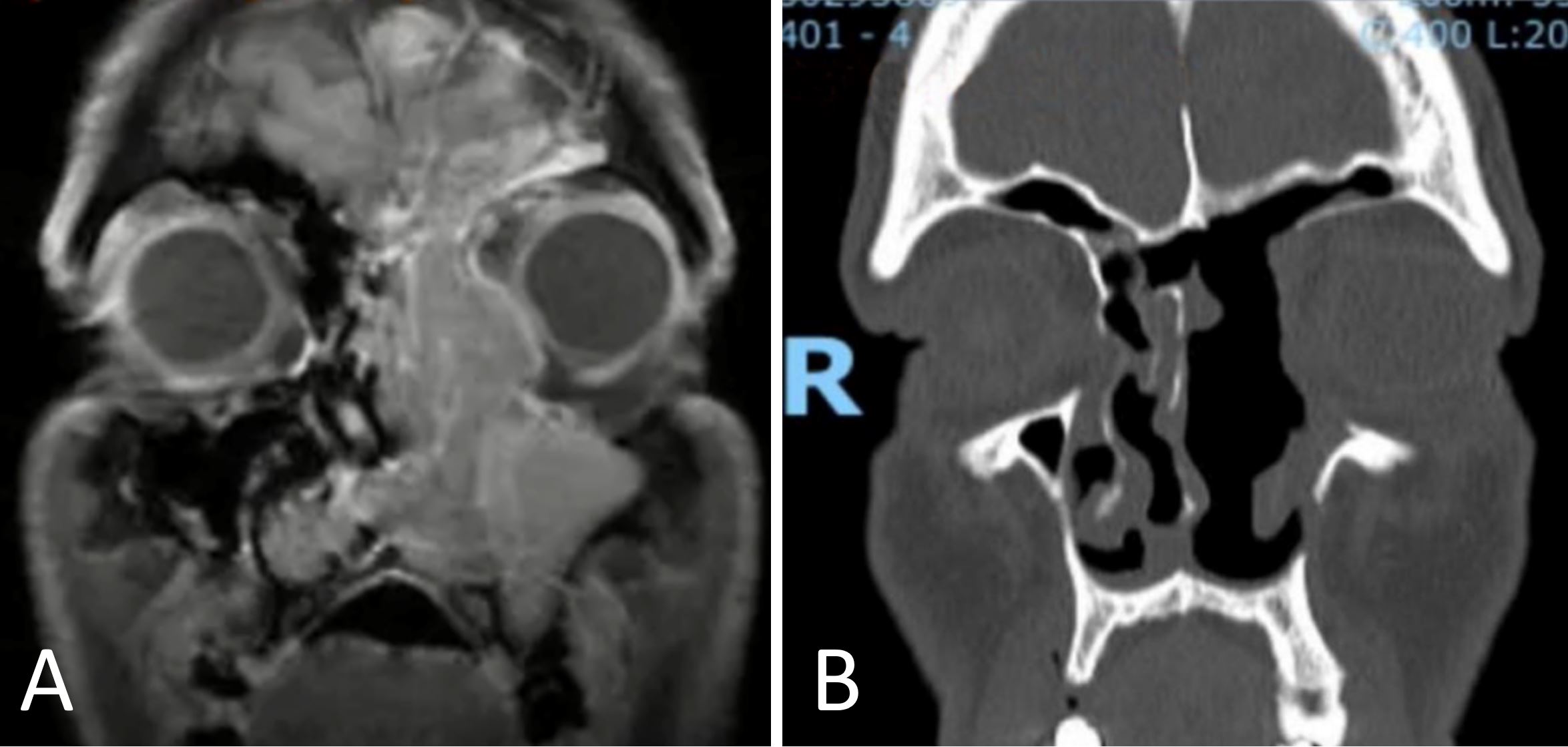
Figure 1. An imaging study displaying preoperative magnetic resonance imaging (A) and postoperative computed tomography (B).
The patient underwent an endoscopic procedure employing a centripetal technique. With this technique, the medial orbital wall and anterior base of the skull were preserved, while the lesion was completely removed. Following the operation, with open paranasal sinuses, there was no periorbital disease. However, a small leak of cerebrospinal fluid was noted within the ethmoidal fovea that was promptly closed using a free middle turbinate flap.
An immunohistochemical analysis (Figure 2) revealed a high-grade non-intestinal adenocarcinoma with 51 mitoses per 10 high-power field, positivity for CK7 and P16 antibodies and negativity for CK20, CDX2 and Ki-67 antibodies with a proliferative index of 70%. It was determined that the patient had a stage pT3N0M0 and was referred to the oncology and radiotherapy departments.
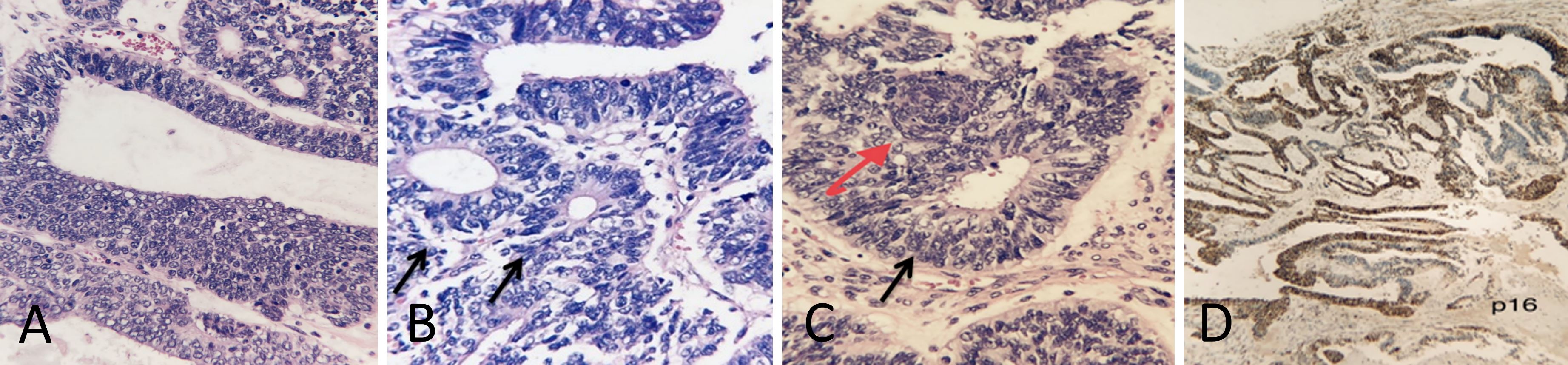
Figure 2. (A) In high-grade non-intestinal adenocarcinomas, glandular formation, marked cellular proliferation, and cellular atypia are evident (x10). (B) This is a high-grade non-intestinal adenocarcinoma characterized by glandular formation and some areas with Flexner-type rosettes (black arrows) and nuclear pleomorphism (x10). (C) The image shows a high-grade non-intestinal adenocarcinoma with a Morular-like metaplasia (red arrow), rosettes-like formation (black arrow), and nuclear atypia (x10). (D) A multi-focal and strong positivity is observed for p16 (x4).
Radiotherapy was administered as adjuvant therapy, but chemotherapy was not indicated. A total of 25 radiotherapy sessions were performed on him with a total dose of 50 Gy. It was decided to use intensity modulated radiotherapy because it is capable of administering higher and more effective doses to tumors with fewer side effects when compared to conventional radiotherapy. There were no significant side effects associated with radiotherapy. The patient underwent a periodic follow-up procedure with serial computed tomography scans on a quarterly basis. There was no evidence of recurrence of the disease after 30 months of treatment, and he continues to follow up with an outpatient physician on a regular basis.
Only a few reports of high-grade sinonasal adenocarcinomas of the non-intestinal type have been published [1,10]. Males are more susceptible to the disease, and it can impact individuals of all ages, from adolescents to the elderly [1,4,10]. As shown in this case, nasal obstruction is the most common symptom, which may be accompanied by swelling or facial deformities. The most common sites of involvement are the nasal cavity and maxillary sinuses [1,7,10,11], although there are instances, such as this one, in which it can extend to other sinuses as well. Adenocarcinomas of the intestinal type have been associated with occupational exposures to wood dust, leather, and flour, whereas there are no risk factors identified for high-grade non-intestinal adenocarcinomas [10].
Even with aggressive treatment, high-grade tumors have a poor prognosis, with a survival rate of only 20% after three years [4,9]. Historically, the average 5-year survival rates of sinonasal carcinomas have been reported to be 28% in the 1960s and 51% in the 1990s, respectively [3]. A recent study by Turner et al. showed that there were some incremental improvements that approached statistical significance [3]. Based on these findings, it has been estimated that the 5-year relative survival rate has increased from approximately 49.7% for patients diagnosed in 1973 to 56.4% for patients diagnosed in 2001. Based on the analysis of 418 patients by Choussy et al., a 5-year overall survival rate of 64% was reported [12].
In a study performed by Bhayani et al., 66 patients were examined, 31 of whom had non-intestinal adenocarcinoma, and a 5-year overall survival rate of 65.9% was reported [13]. Among 24 patients studied by Orvidas et al., 58% had non-intestinal adenocarcinomas, and the 5-year overall survival rate was 58% [14]. The study conducted by Chen et al. is the only one to independently analyze non-intestinal adenocarcinoma [15]. In an analysis of 300 cases of non-intestinal adenocarcinoma, the authors reported a disease-specific survival rate of 71.2% with no statistically significant differences in survival when compared with 25 cases of intestinal adenocarcinoma. In a study of low-grade and high-grade sinonasal non-intestinal-type adenocarcinomas, the 5-year overall survival rate and the disease-specific survival rate were 100% and 100% for G1 tumors, respectively; 87.5% and 87.5% for G3 tumors, respectively; while the 5-year recurrency-free survival rate was 91.7% for G1 tumors and 88.9% for G3 tumors [9].
As far as the nasal cavity and the paranasal sinuses are concerned, adenocarcinomas can be classified as salivary gland, intestinal, or non-intestinal types of low or high grade [10,16]. The non-intestinal type uses these nomenclatures due to the lack of morphological characteristics and immunohistochemical patterns observed in salivary gland adenocarcinomas or intestinal type adenocarcinomas [4,17,18].
Upon macroscopy, non-intestinal tumors may have flat or exophytic appearances, and their color may range from white to violaceous, and they may contain areas that are friable and/or solid, depending on the type of tumor [10,18]. In the case described, macroscopically, there was an irregular outline associated with exophytic growth, violaceous color, and areas that were sometimes friable and sometimes solid.
Low-grade non-intestinal adenocarcinoma is an encapsulated tumor with a pattern of glandular or papillary growth. It presents low to moderate pleomorphism in the cell structure, with occasional mitoses, but not with atypical mitoses or necrosis [1,17,18].
In contrast, high-grade non-intestinal adenocarcinoma is an invasive tumor that has a solid pattern, containing glandular or papillary foci; some of the tumors exhibit blastomatous characteristics of teratocarcinoma [10,17], may form Flexner rosettes, and may exhibit morular squamous metaplasia, as shown in Figures 2A and 2B, respectively in this report. There is a moderate to severe level of pleomorphism, and the mitotic index is high (more than 5 mitotic figures per 10 high-power fields), characterized by both atypical mitosis and necrosis [4,10,18]. It is imperative to distinguish between salivary gland-type adenocarcinoma, intestinal-type adenocarcinoma, and metastatic adenocarcinoma when making the differential diagnosis [18].
An immunohistochemical pattern of high-grade non-intestinal adenocarcinoma shows a strong and diffuse positivity for CK7 [16,17]. There may be some cases where p16 is positive (as shown in Figure 2D in our case report), which necessitates the detection of HPV strains with a high likelihood of causing neoplasia. Rarely, neuroendocrine markers such as synaptophysin and chromogranin exhibit weak or focal positivity [17]. They are negative for CK20 and CDX-2, which differentiates them from intestinal type adenocarcinoma and defines the final diagnosis in this case [16,18].
When adenocarcinomas are detected at an early stage, surgical treatment can be used alone, resulting in a 5-year survival rate of 83.4%. Among patients with more advanced stages of the disease, the 5-year survival rate is 66.6% when surgery and radiotherapy are combined. Radiotherapy alone was not found to have a significant benefit in terms of 5-year survival when compared with no treatment [19].
There are some key insights that can be gained from this case. To begin with, high-grade, non-intestinal sinonasal adenocarcinomas are uncommon and aggressive. It is common for patients to experience nasal obstruction as one of the most prominent symptoms. A complete resection of the tumor may result in better outcomes, which can be achieved through endoscopic access. A nonspecific clinical presentation usually results in a delayed diagnosis. A positive immunohistochemistry finding was observed for CK 7 and a negative finding for CK20 and CDX-2. In this case, we learned that high-grade non-intestinal adenocarcinoma is an exclusion diagnosis, because the histopathological characteristics are used to identify and exclude other forms of adenocarcinoma, including those of the intestinal and salivary types. A multidisciplinary assessment is also essential for the effective management of patients. The purpose of this case report is to emphasize that surgery with meticulous resection is essential to ensure a better outcome.
This is an uncommon case of high-grade non-intestinal sinonasal adenocarcinoma that represents a challenging diagnosis. It is imperative to distinguish it from other sinonasal tumors since it has a significantly different prognosis. For a definitive diagnosis, a detailed anamnesis is required, a radical endoscopic resection to achieve a total excision is necessary, and satisfactory immunohistochemistry results are required.
Received date: May 01, 2022
Accepted date: August 18, 2022
Published date: September 22, 2022
The manuscript has not been presented at any meetings on the topic.
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The authors obtained permission from the participants in the human research prior to publishing their images or photographs.
This research has received no specific grant from any funding agency either in the public, commercial, or not-for-profit sectors.
There are no conflicts of interest declared by either the authors or the contributors of this article, which is their intellectual property.
It should be noted that the opinions and statements expressed in this article are those of the respective author(s) and are not to be regarded as factual statements. These opinions and statements may not represent the views of their affiliated organizations, the publishing house, the editors, or any other reviewers since these are the sole opinion and statement of the author(s). The publisher does not guarantee or endorse any of the statements that are made by the manufacturer of any product discussed in this article, or any statements that are made by the author(s) in relation to the mentioned product.
© 2022 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). In accordance with accepted academic practice, anyone may use, distribute, or reproduce this material, so long as the original author(s), the copyright holder(s), and the original publication of this journal are credited, and this publication is cited as the original. To the extent permitted by these terms and conditions of license, this material may not be compiled, distributed, or reproduced in any manner that is inconsistent with those terms and conditions.
Gehrke V, Beraldin BS, Lubianca Neto JF, Barra MB, Viga JDC, Vieira MZDD, Houdali ISHM, Rocha Filho MAM. A rare case of high-grade non-intestinal sinonasal adenocarcinoma. Arch Otorhinolaryngol Head Neck Surg 2022;6(2):2. https://doi.org/10.24983/scitemed.aohns.2022.00165