In Belgium, the incidence of dog bite injuries stands at 22 per thousand for children under the age of fifteen, a demographic particularly vulnerable to severe facial trauma. While prompt microsurgical replantation within the craniofacial region is linked to enhanced recovery outcomes, its adaptation for pediatric care presents distinct challenges. This report examines the case of a 2.5-year-old girl who sustained a severe full-thickness avulsion of the lower lip, measuring 2 x 1.5 cm, due to a dog bite. Successful microsurgical intervention involved retrieving the right inferior labial artery for an end-to-end anastomosis with the arterial stump of the amputated segment. Venous congestion was managed with leech therapy, which facilitated complete motor and sensory recovery, including the restoration of normal speech and oral continence. Accompanying this case, a review of microsurgical lip replantation in children aged 12 and under was conducted through PubMed and Google Scholar, using keywords such as "lip amputation," "lip avulsion," "lip replantation," and "lip reimplantation." This review identified 17 cases and underscored that ischemia times up to 6 hours do not preclude successful replantation in children, given their reduced susceptibility to ischemia-reperfusion injury. Finding an appropriate vein for anastomosis proves difficult, resulting in a reliance on artery-only anastomosis in 41% of cases, equating to seven patients. Nonetheless, a notable 82% of cases, totaling fourteen patients, achieved complete replant survival. In conclusion, this study underscores the long-term success of microsurgical replantation for severe lower lip avulsion in pediatric patients, highlighting significant functional and aesthetic benefits. It stresses the necessity for specialized centers, comprehensive postoperative surveillance, and effective venous drainage strategies to improve outcomes. The findings reveal gaps in long-term data, reinforcing the need for standardized treatment protocols and specialized follow-up to optimize treatment efficacy and address frequent venous congestion in this vulnerable age group.
In Belgium, there is a reported annual incidence of 22 dog bite injuries per 1000 children under the age of 15, with most incidents occurring at home with familiar dogs [1]. This age group is especially susceptible to severe facial injuries from such encounters, emphasizing the importance of robust treatment protocols [2,3]. Maintaining a functional oral sphincter is critical for normal development in children, and adhering to the "replace like with like" principle in microsurgical replantation in the head and neck area not only preserves essential functions but also delivers superior aesthetic outcomes [4–8]. Despite the challenges posed by smaller arteries and less defined labial veins in pediatric patients [4,9,10], replantation is recommended as the preferred method. This preference is supported by observations of less severe ischemia-reperfusion injuries in younger patients, which contribute to more favorable recovery results [11].
Significant gaps persist in longitudinal follow-up studies concerning pediatric patients after lip replantation, with scarce data on the post-surgical functional and aesthetic outcomes. This dearth of information underscores critical concerns regarding the long-term efficacy of these surgeries and the ongoing quality of life for the affected individuals.
This paper details a case of a 2.5-year-old patient who experienced a severe lower lip avulsion, impacting more than two-thirds of the lip, following a dog bite. The focus of this study is on assessing long-term surgical outcomes for such pediatric injuries, which present substantial challenges, requiring refined surgical approaches and elaborate postoperative care plans. Complementing the case analysis, this article includes a comprehensive review of the literature on pediatric lip avulsions and microvascular repair techniques. The intent is to contextualize this individual case within a broader spectrum of similar incidents, critically examining the variety of available treatment methodologies and their respective outcomes in young patients. Through meticulous evaluation, this study aims to critique and enhance current medical protocols, identifying key areas for innovation in pediatric facial reconstructive surgery.
A 2.5-year-old girl was admitted following a dog bite that resulted in a severe full-thickness avulsion of her lower lip, affecting over two-thirds of the lip area and causing considerable tissue damage. This condition necessitated sophisticated microsurgical intervention.
On admission, the extent of the injury was immediately apparent, and the initial state of the injury is captured in Figure 1A. The amputated segment of the lower lip, measuring 2 x 1.5 cm, was successfully retrieved as a single tissue unit and is shown in Figure 1B. Crucially, both oral commissures were preserved.
Microscopic inspection revealed the presence of the small arterial stump of the inferior labial artery embedded within the avulsed orbicularis oris muscle, and its corresponding part was located in the wound bed.

Figure 1. (A) A 2.5-year-old female presents with a significant full-thickness avulsion of the lower lip, comprising over two-thirds of the area, due to a canine assault. (B) The amputated tissue, recovered as a cohesive unit, measures 2 x 1.5 cm. The integrity of both oral commissures is preserved. (C) Microscopic examination uncovers the diminutive arterial stump of the inferior labial artery embedded within the avulsed orbicularis oris muscle. Its counterpart in the wound bed is also discerned. A meticulous isolation of the artery extends 3 mm within the excised tissue, paralleled by a careful dissection in the wound's recipient bed. (D) A post-operative overview demonstrates the successfully reattached segment of the lip, where each anatomical layer has been sutured distinctively.
Surgical Procedure
During the operation, meticulous care was taken to isolate the artery over a 3 mm segment in both the amputated part and the recipient wound bed, as shown in Figure 1C. An end-to-end microsurgical anastomosis was carefully performed with interrupted Ethilon 11/0 sutures. Upon releasing the vascular clamp, successful reperfusion and visible capillary refill were observed, confirming the restoration of arterial inflow; however, no veins were identified post-restoration. The anatomical layers, comprising both muscle and mucosa, were individually and meticulously sutured using Vicryl 7/0. Closure of the surgical wounds was achieved using Ethilon 8/0 sutures, as illustrated in Figure 1D. It is notable that no nerves were retrieved during the procedure.
Postoperative Care
Following the surgical intervention, the young patient was intubated for 11 days to ensure stable breathing. To mitigate the risk of thrombosis and infection, she was administered low molecular weight heparin for 8 days and a course of intravenous antibiotics (amoxicillin/clavulanic acid) spanning 12 days. Anticipating complications from venous congestion, medicinal leech therapy was employed for 5 days, during which the child required blood transfusions totaling 4 units of packed red blood cells, adhering to a dosage of 10ml/kg. Nutritional support was provided through nasogastric tube feedings and parenteral nutrition until she was capable of adequate oral intake. Her recovery progressed smoothly, and on the 19th day post-surgery, she was transferred from the pediatric intensive care unit to the pediatric ward. The patient was subsequently discharged on the 23rd day, marking a significant milestone in her recovery journey.
Outcome and Follow-up
The replanted segment of the lip experienced complete recovery. Throughout a comprehensive seven-year follow-up period, the patient fully regained motor and sensory functions. This restoration was demonstrated through her maintained oral continence, normal speech, and ability to whistle. Sensory recovery was specifically verified by a two-point discrimination test on the lip, which measured at 2 mm (Figure 2). Additionally, supplementary video material is available at https://doi.org/10.24983/scitemed.imj.2024.00183, providing further visual documentation of the extensive recovery process. This detailed follow-up underscores the long-term success of the surgical intervention and postoperative care.

Figure 2. Sequential evaluation over seven years of functional and sensory restitution following reconstructive surgery for a full-thickness avulsion of the lower lip in a young patient. (A) At rest, the lip exhibits symmetrical alignment. (B) Volitional movement reveals intact motor function, coupled with preserved oral continence during a smile. (C) Whistling, a demonstration of muscular dexterity and recovery. The patient achieves complete sensory reacquisition, with a two-point discrimination threshold refined to 2 mm, and full motor restoration is documented, including unimpaired speech.
Video This visual documentation traces the remarkable course of recovery in a young individual over a span of seven years subsequent to undergoing reconstructive surgery for a severe lower lip avulsion. The captured footage offers a comprehensive assessment, spotlighting the subject's restored functionalities and the enduring efficacy of the surgical intervention. Throughout the observation, the subject exhibits refined muscular control, as evidenced by skillful whistling, displays complete muscular mobility with maximal mouth opening, and maintains symmetrical lip positioning during periods of relaxation. Moreover, voluntary movements are showcased, underscoring preserved motor proficiency and sustained oral continence across a gamut of facial expressions, including smiles. This documentary not only serves as a testament to the subject's perseverance but also underscores the profound and enduring dividends of advanced reconstructive surgical techniques. It furnishes a compelling illustration of medical progress and the transformative potential of expert surgical interventions in reinstating functionality and enhancing overall quality of life.
A comprehensive literature search focusing on microvascular lip replantation in children was conducted up until October 2023, utilizing the electronic databases PubMed and Google Scholar. The search employed specific keywords: "lip amputation," "lip avulsion," "lip replantation," and "lip reimplantation." Additionally, the bibliographies of retrieved articles were scrutinized to identify any cases not previously detected through the initial search. The inclusion criteria were strict, considering only studies involving children younger than 12 years of age and excluding those that described replantation as a composite graft without vascular anastomosis. The collected data encompassed a variety of variables where available, including the age of the patients, the cause and location of the avulsion, ischemia times, the use of anticoagulant and antibiotic therapies, specifics of vascular anastomoses, the employment of leech therapy, and the duration of follow-up alongside outcomes and any complications. Due to a small sample size, the analysis was confined to descriptive statistics, providing foundational insights into the efficacy and challenges of lip replantation procedures in the pediatric demographic.
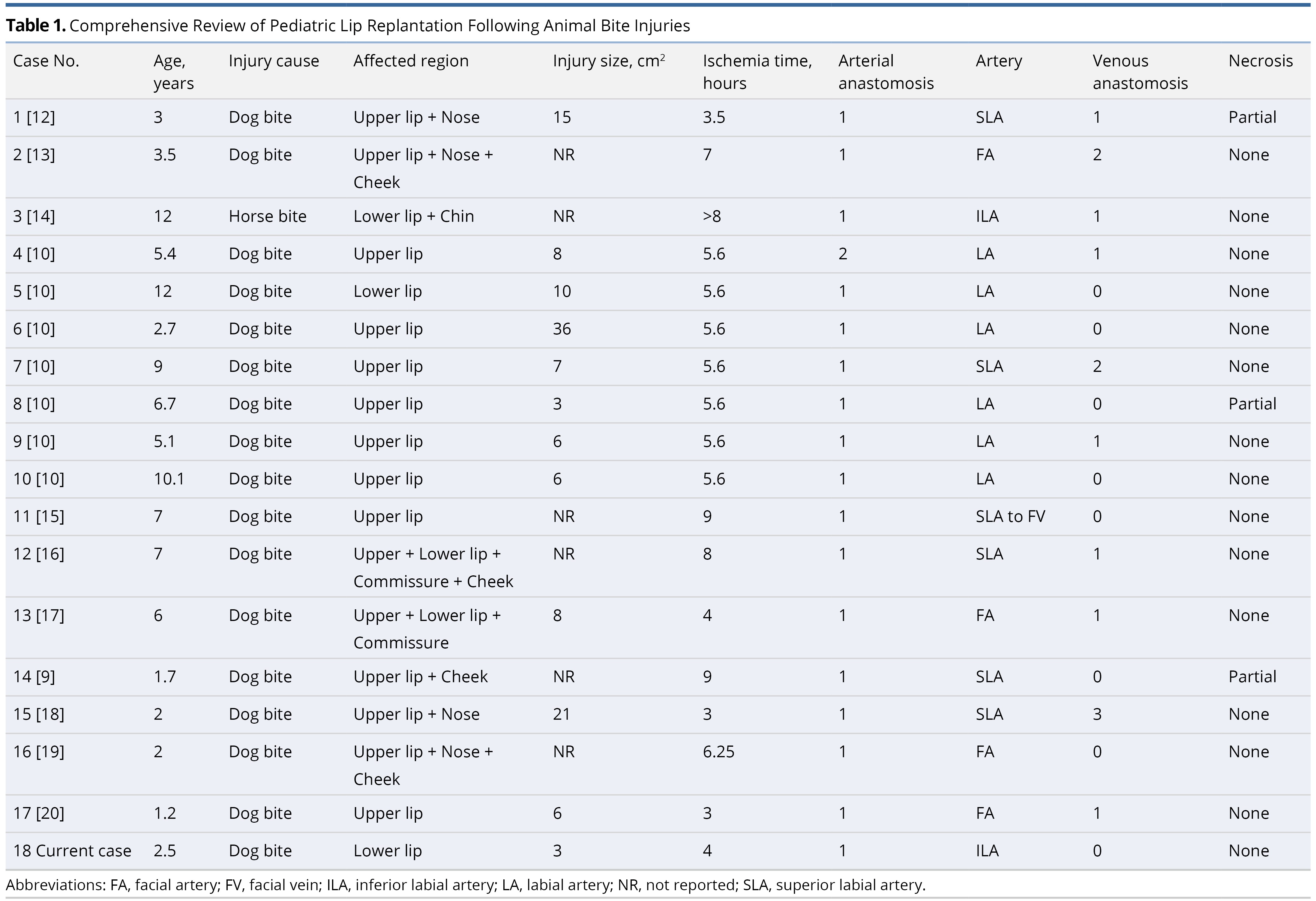
Overview of Pediatric Lip Replantation
A focused review of the literature revealed 17 cases of microsurgical lip replantation in children aged 12 years and younger (Table 1) [9,10,12–20]. The average age of these patients was 5.7 years, which aligns with findings that younger children are more susceptible to facial injuries from dog bites [1]. The youngest patient in these studies was only 14 months old at the time of surgery [20]. Each case involved avulsions of the lip rather than the crush or cutting lesions more typical in adult incidents. Such injuries in children often affect longer segments of the intima, significantly complicating the replantation process [7]. This overview underscores the unique surgical challenges posed by pediatric lip avulsions and highlights the need for specialized approaches in these delicate cases.
Challenges in Pediatric Vascular Anastomosis
The average ischemia time reported in pediatric lip replantation cases is 5.9 hours, typically within the 6-8 hour range considered tolerable for muscle tissue preservation. Notably, in the case discussed, the cold ischemia time was only 4 hours, comfortably within this safe range, although durations of up to 9 hours have also been managed without complications [9]. This suggests that extending ischemia times beyond six hours does not necessarily preclude successful replantation in children, as ischemia-reperfusion injuries are generally milder in this demographic [9].
Ischemia-reperfusion injuries in children are predominantly mediated by neutrophils. Studies have documented age-related impairments in neutrophil activity in human neonates, where neutrophil migration to injured tissue is less effective, and oxidative burst activity is significantly reduced [11]. Additionally, mast cells, which also play a significant role in ischemia-reperfusion injuries, are known to increase in number with age, adding another layer of complexity in adult cases [21]. These factors potentially contribute to the better outcomes observed in younger patients undergoing replantation [9]. However, the understanding of these mechanisms in the pediatric population remains incomplete, warranting further research into age-related differences in ischemia-reperfusion injury responses.
Finding a suitable vein for anastomosis remains a substantial challenge in pediatric replantation cases, exacerbated by the smaller vessel sizes, which decrease in diameter from lateral to medial [5,7,10]. Despite these challenges, our findings and additional literature confirm that replantation is indeed feasible in very young patients, highlighting the importance of specialized surgical techniques and careful planning in managing these delicate procedures.
Artery-Only Anastomosis Techniques
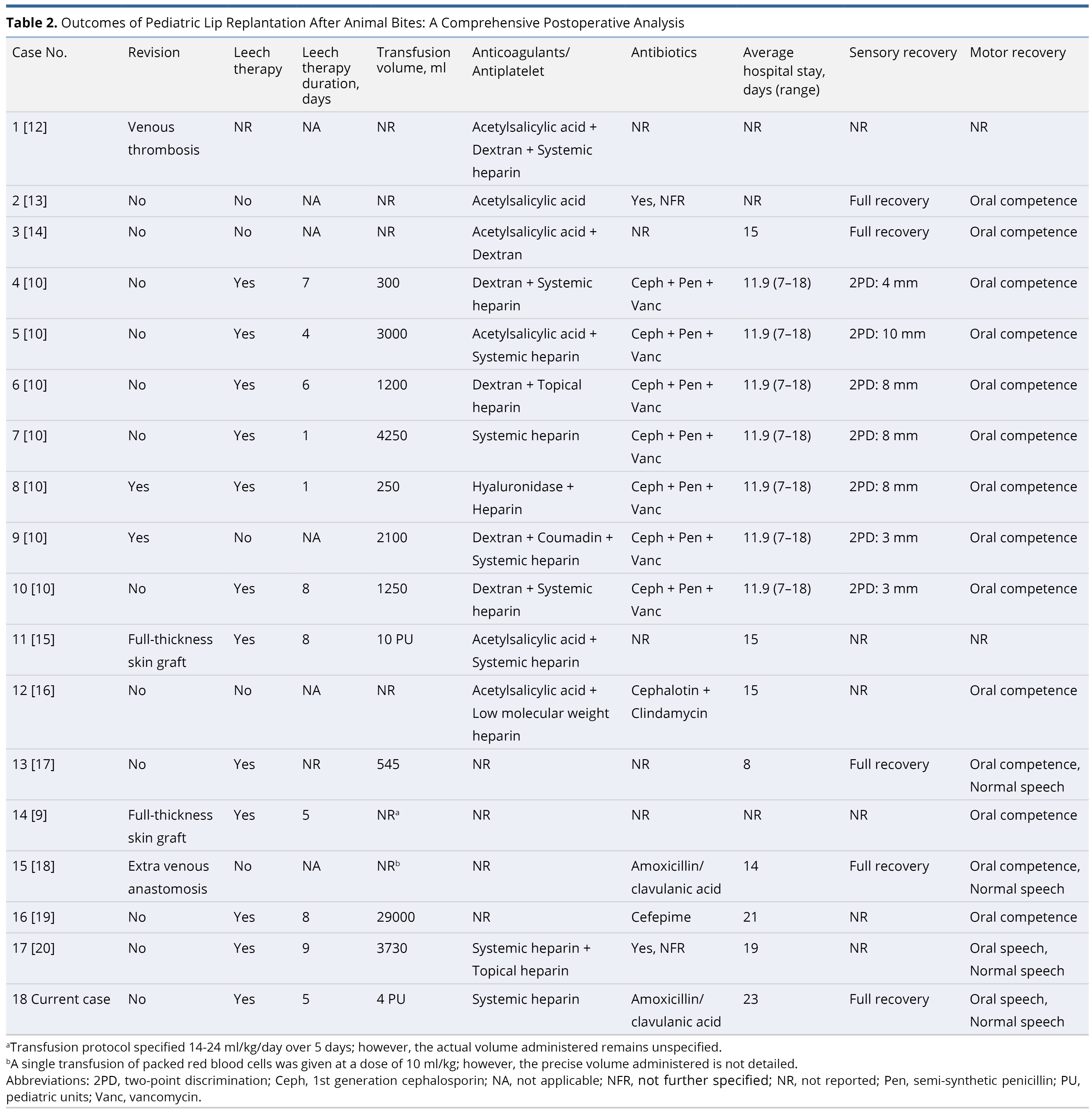
In our review, 41% of the seventeen documented cases of pediatric lip replantation reported employing artery-only anastomosis [5,10,22]. In scenarios lacking venous anastomosis, securing an alternative method for venous drainage becomes critical for the viability of the replanted tissue. The strategies adopted typically involve a multimodal approach aimed at alleviating venous congestion, which includes both topical and systemic anticoagulation combined with leech therapy.
Among these cases, a substantial proportion received anti-thrombotic therapy: 18% were treated with anti-platelet medication alone, another 18% with only anticoagulants, while a significant 44% received a combination of both treatments. Notably, two of the three patients who experienced partial necrosis were undergoing treatment with systemic heparin. The use of anticoagulants in such surgeries, particularly to prevent clot formation and maintain blood flow in free flap surgeries, remains a controversial topic with limited supporting evidence [22–24]. This issue is even more pronounced in the pediatric population, where research on the effectiveness and safety of anticoagulants in microvascular anastomosis is scarce, highlighting a critical gap in current medical literature and underscoring the need for further investigation.
Medicinal Leeches in Venous Congestion Relief
In scenarios of artery-only anastomosis, medicinal leeches have been consistently utilized to alleviate venous congestion, as outlined in Table 2. This method of venous drainage was also employed in our specific case study. Notably, even among cases that successfully achieved venous anastomosis, four out of ten still required the use of leech therapy. One significant concern with this approach is the substantial blood loss involved; all patients required blood transfusions, with one extreme case necessitating as much as 29 liters of blood [19]. This rate of transfusion contrasts sharply with adult cases, where typically only about one-third of patients undergoing leech therapy need transfusions [25]. In our observations, the duration of leech therapy across cases averaged 5.7 days, a period typically necessary for neoangiogenesis to effectively proceed [5]. This highlights both the utility and the complexities of using leeches in managing venous congestion in pediatric microsurgical procedures.
Risks of Leech Therapy in Pediatric Patients
The use of medicinal leech therapy in pediatric patients is associated with significant risks and potential complications. Notably, this therapy often leads to considerable blood loss, frequently requiring transfusions, and increases the risk of infection, underscoring the critical need for vigilant monitoring and proactive antibiotic prophylaxis. The increased need for blood transfusions in young patients demands careful consideration due to the inherent risks involved. Additionally, while not widely reported, the need for sedation during leech therapy, particularly for facial applications, is a realistic possibility and should be carefully considered. Effective communication with patients and their families is essential to navigate these complexities and manage expectations appropriately. Given these challenges, further investigation into alternative, non-traditional methods of venous drainage for this demographic is recommended to enhance safety and efficacy.
Postoperative Antibiotic Protocols
The application of postoperative antibiotics follows specific regional guidelines, with Belgian and Dutch protocols recommending the use of amoxicillin-clavulanic acid for a period of 5-14 days following facial injuries from dog bites [3]. Additionally, the role of antibiotic prophylaxis is particularly emphasized in cases involving medicinal leech therapy, as supported by multiple articles and guidelines that advocate for its use to prevent potential infections [26–28].
In the scope of the literature reviewed, antibiotics were recorded as part of the treatment strategy in approximately 71% of the cases, equating to twelve instances. This highlights a general adherence to recommended practices in the majority of instances. However, there is a notable gap in documentation for the remaining cases; the reports do not specify whether antibiotics were used or omitted. This lack of explicit reporting underscores the need for more thorough documentation and adherence to standardized treatment protocols to ensure comprehensive patient care and infection control in postoperative management.
Replantation Outcome Analysis
No instances of complete flap failure were reported in the reviewed cases. However, three cases did experience partial flap failure, accounting for 18.8% of the cases, with one being attributed to iatrogenic causes. Impressively, 82% of the cases, or fourteen patients, achieved complete survival of the replanted lips, an outcome that stands out positively when compared to general survival rates in head and neck replantation [7]. It is important to note, however, that there is a potential for these results to be influenced by publication bias.
Typically, normal two-point discrimination for the upper and lower lip is measured at 3 ± 1.1 mm using a static sharp object [29]. Walton et al. have recommended that at least 1 cm of moving two-point discrimination is necessary for adequate protective sensibility, noting that their pediatric studies averaged 6 mm [10]. While some studies have not confirmed sensitive recovery, fifteen out of seventeen cases successfully attained full oral continence, a crucial objective in the reconstruction of the oral stoma [4].
Research Limitations and Potential Bias
This article acknowledges several limitations that may impact the interpretation of its findings. Most notably, there exists a significant risk of publication bias, with the possibility that the documented results are biased toward successful outcomes, potentially underrepresenting less favorable results. The conclusions drawn from this review are based on a relatively small cohort of cases, which necessitates caution in generalizing the findings, especially regarding extended ischemia times where individual responses can vary. The complexities of ischemia-reperfusion injury in children are not yet fully understood, adding another layer of uncertainty. Additionally, research into the efficacy and safety of anticoagulants and leech therapy in pediatric patients is still limited, highlighting an urgent need for more comprehensive, controlled studies to develop more definitive clinical guidelines.
Key Lessons from Pediatric Replantation Studies
The insights derived from these studies offer several important lessons for clinical practice. First, surgeons are urged to consider microsurgical replantation as a preferred option when feasible, due to its proven superior functional and aesthetic results in pediatric cases. Second, the importance of meticulous post-operative monitoring cannot be overstated, and having effective alternatives for venous drainage at hand is crucial to manage potential complications. Lastly, it is critical to recognize that surgical replantation in children is a high-risk procedure that demands not only technical expertise but also effective communication with both the patient and their family throughout the treatment journey to ensure optimal outcomes and patient satisfaction.
This study demonstrates the successful long-term effects of microsurgical replantation for severe lower lip avulsion in pediatric patients, with a particular emphasis on significant functional and aesthetic benefits. Supported by an extensive literature review, the findings affirm consistent treatment efficacy in this age group, while also exposing notable gaps in long-term data. These insights underscore the necessity for standardized treatment protocols, specifically tailored to pediatric patients, and emphasize the importance of prolonged follow-up. Despite potential challenges, such as costs and medical complications, replantation of substantial avulsed lip segments remains the preferred treatment for children younger than 12, due to its superior outcomes. Efforts to enhance surgical results in pediatric cases include potential transfers to specialized centers and the development of alternative methods for venous relief, designed specifically to address the frequent venous congestion observed in children.
Received date: November 30, 2023
Accepted date: March 14, 2024
Published date: May 06, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.


Video This visual documentation traces the remarkable course of recovery in a young individual over a span of seven years subsequent to undergoing reconstructive surgery for a severe lower lip avulsion. The captured footage offers a comprehensive assessment, spotlighting the subject's restored functionalities and the enduring efficacy of the surgical intervention. Throughout the observation, the subject exhibits refined muscular control, as evidenced by skillful whistling, displays complete muscular mobility with maximal mouth opening, and maintains symmetrical lip positioning during periods of relaxation. Moreover, voluntary movements are showcased, underscoring preserved motor proficiency and sustained oral continence across a gamut of facial expressions, including smiles. This documentary not only serves as a testament to the subject's perseverance but also underscores the profound and enduring dividends of advanced reconstructive surgical techniques. It furnishes a compelling illustration of medical progress and the transformative potential of expert surgical interventions in reinstating functionality and enhancing overall quality of life.
A novel technique of sequential ETS micro-venous anastomoses using three vessel loops for IJV occlusion and a single vascular clamp to retract and hold the anastomoses sites in position.
The authors present a novel synthetic vascular model for microanastomosis training. This model is suitable for trainees with intermediate level of microsurgical skills, and useful as a bridging model between simple suturing exercise and in vivo rat vessel anastomosis during pre-clinical training.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
This case report and literature review focus on pediatric lower lip replantation using artery-only micro-anastomosis. The study discusses a 2.5-year-old girl who suffered a dog bite resulting in a full-thickness lower lip avulsion exceeding two-thirds of the lip. The right inferior labial artery was retrieved from the wound bed, and an end-to-end anastomosis was performed. Venous drainage was managed using leech therapy. The patient achieved full motor and sensory recovery with normal speech and oral continence. The literature review identified 17 cases of microsurgical lip replantation in children aged 12 or younger, with 41% involving artery-only anastomosis. The overall reported survival rate for complete replantation was 82%. The study concludes that microsurgical replantation should be the first choice for avulsed lip segments in patients under 12 years old, with artery-only anastomosis being a viable option. Consideration of transferring patients to tertiary centers for replantation is encouraged. The article, as it stands, raises several critical concerns that may hinder its suitability for publication.
This article exerts a significant impact within the realm of microsurgical replantation, specifically focusing on pediatric lower lip avulsion cases and the utilization of artery-only micro-anastomosis techniques. Through a compelling case report and comprehensive literature review, it illuminates a compelling approach to intricate surgical procedures in young patients. Notably, the study underscores the feasibility of artery-only anastomosis and the critical importance of swift action in avulsed lip segments. While the article demonstrates expertise in its execution, a few specific considerations must be addressed and resolved to ensure its publication's full potential.
Ceulemans A, Sommeling C, Luyten P, Van Landuyt K, Stillaert F. Longitudinal success of artery-only microanastomosis in pediatric lower lip replantation: A seven-year case study and review of the literature. Int Microsurg J 2024;8(1):2. https://doi.org/10.24983/scitemed.imj.2024.00183