Free flap is now a routinely performed operation and an essential part of reconstructive surgery. End-to-Side (ETS) anastomosis is an assistant dependent microvascular procedure that remains to be technically challenging with steep learning curve. This is a novel technique created by the senior author of this paper. It is a technique of sequential ETS micro-venous anastomosis using widely available vessel loops and an additional single vascular clamp. The surgical technique is described in detail, and in-depth literature review has been conducted and presented. The vessel loop provides superior protection to the vessel over vascular clamps, and achieves equisegmental internal jugular vein occlusion for sequential (proximal to distal) venous anastomosis. Utilizing a second single vascular clamp with the maneuver described reveals and maintains an accessible position to the posterior wall of the anastomosis, which enables the surgeon to operate independently with this unique technique.
Video. Chang’s technique of sequential end-to-side microvascular anastomosis
End-to-End (ETE) microvascular anastomosis is the first-line option for most microsurgeons in free flap surgery. It is less technically demanding and also surgical assistant independent. However, due to frequent encounter of vessel calibre mismatch for both width and thickness, as well as the presence of vessel depleted recipient regions [1] due to surgical ablation, trauma or pre-operative radiotherapy, End-to-Side (ETS) microvascular anastomosis can serve as an excellent alternative option.
In contrast to ETE anastomosis, ETS anastomosis is technically more challenging with steeper learning curve. It is also a difficult operation to be performed independently. In head and neck surgery, the trunk of internal jugular vein (IJV) is commonly preserved. Thus, instead of searching for suitable veins for ETE venous anastomosis, ETS anastomosis to IJV is a more reliable approach. ETS is also recommended in the event of significant size discrepancy. Direct venous drainage of pedicle veins into a vein with greater calibre, such as IJV, may result in more desirable outcome compared to ETE anastomosis between two veins with significant size discrepancy [2].
This paper aims to describe a novel technique of sequential ETS micro-venous anastomoses using three vessel loops for IJV occlusion and a single vascular clamp to retract and hold the anastomoses sites in position, thus gaining access to posterior wall and perform the operation independently.
Two pedicle veins from a donor anterolateral thigh flap were isolated from the vascular bundles up to 3 cm in length from their point of ligations. A single microvascular clamp was applied on each pedicle vein to prevent venous backflow that may disrupt the microsurgical field. Main trunk of internal jugular vein (IJV) was also isolated from its surrounding connective tissues. Three 5 cm vessel loops (blue) were used for two segmental IJV occlusions (proximal and distal), using right angle forceps for their guided pass to create figure of 8 configurations. Each vessel loop was then retracted with mosquito forceps as soon as the appropriate tension was set for segmental IJV occlusion (Figure 1). Limited adventitiectomy was performed at the end of each pedicle vein as well as IJV surface under the microscope to prevent unintentional plication of venous adventitia into lumen of the anastomosis site.
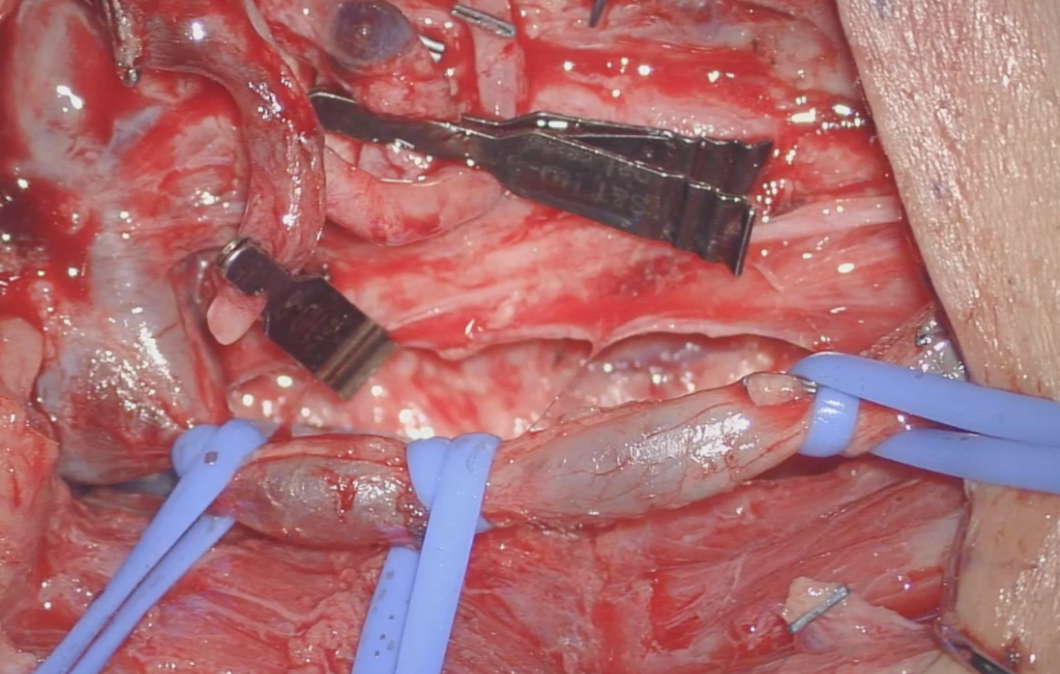
Figure 1. Using Vessel Loops x 3 to occlude venous drainage back to IJV and provide 2 IJV segments for End-to-Side Anastomosis.
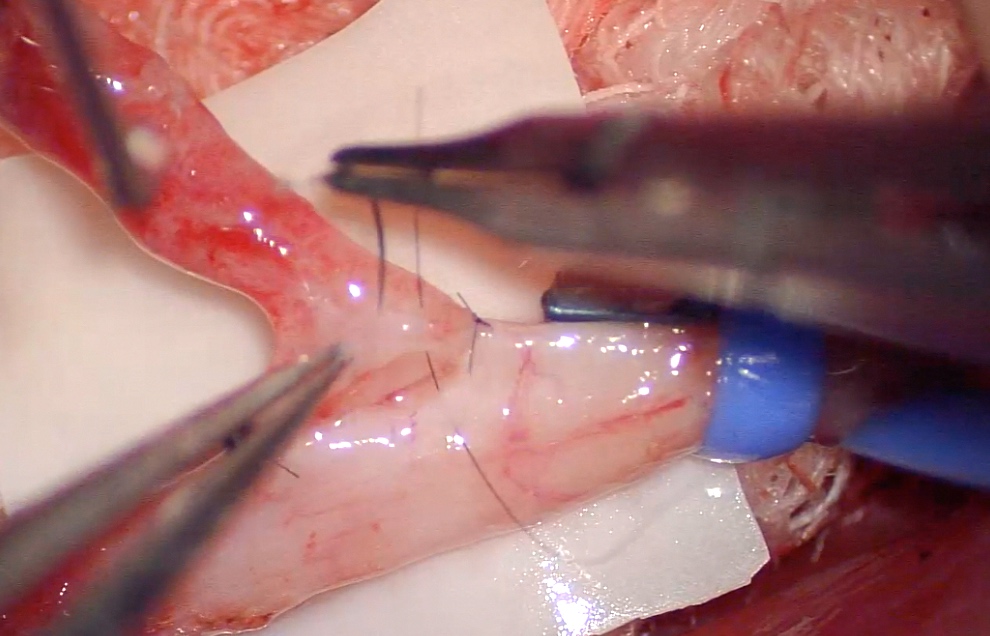
The aim was to set a slight tension between pedicle veins and IJV in the anastomoses design to avoid vessel redundancy, and consequently prevent vessel kinking. Once the adequate tension was set, a parallel incision was made over the proximal segment of occluded IJV sized to the diameter of the pedicle vein. Two anchor sutures were placed over 3 and 9 o'clock of the IJV (Figure 2). Continuous looping technique was used from right to left for the anterior wall anastomosis (Figure 3).
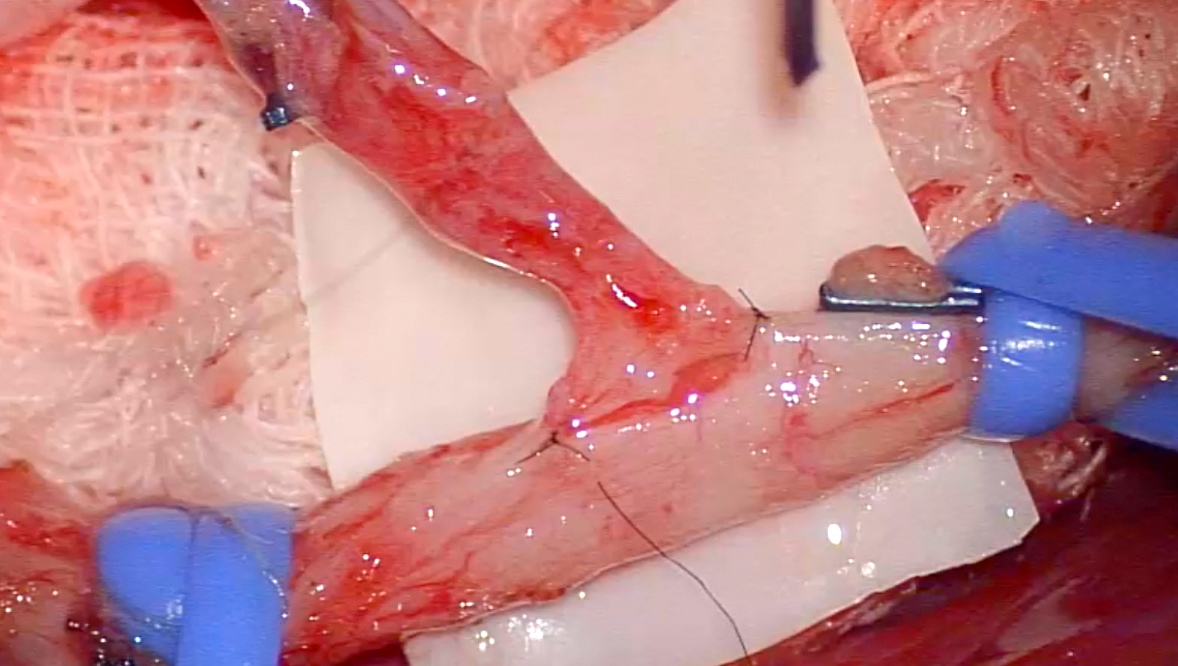
Figure 2. Two anchoring sutures placed over 3 and 9 o’clock.
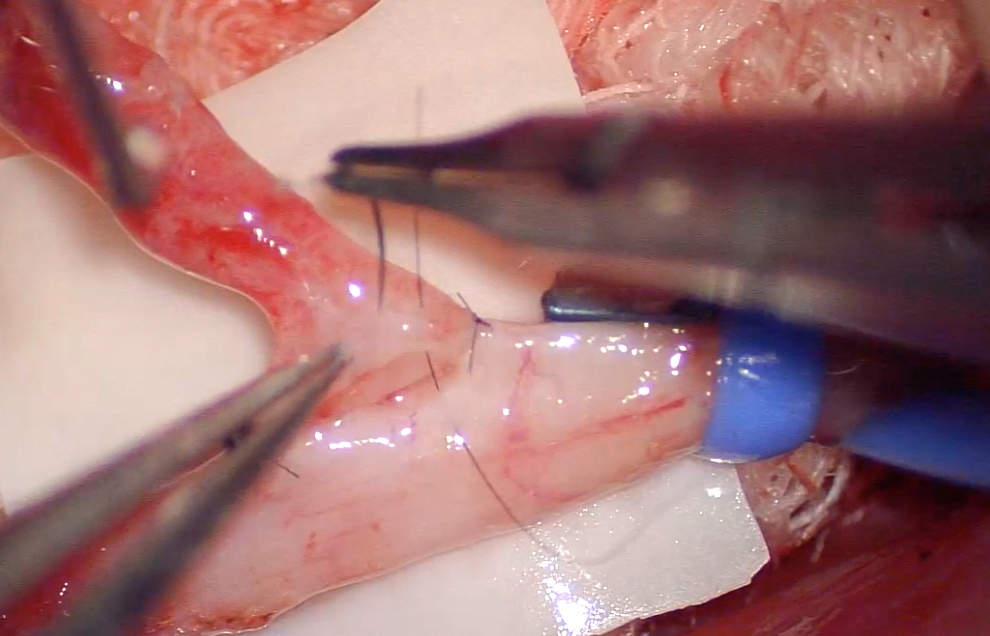
Figure 3. Demonstrating right to left continuous looping technique used for anterior wall anastomosis.
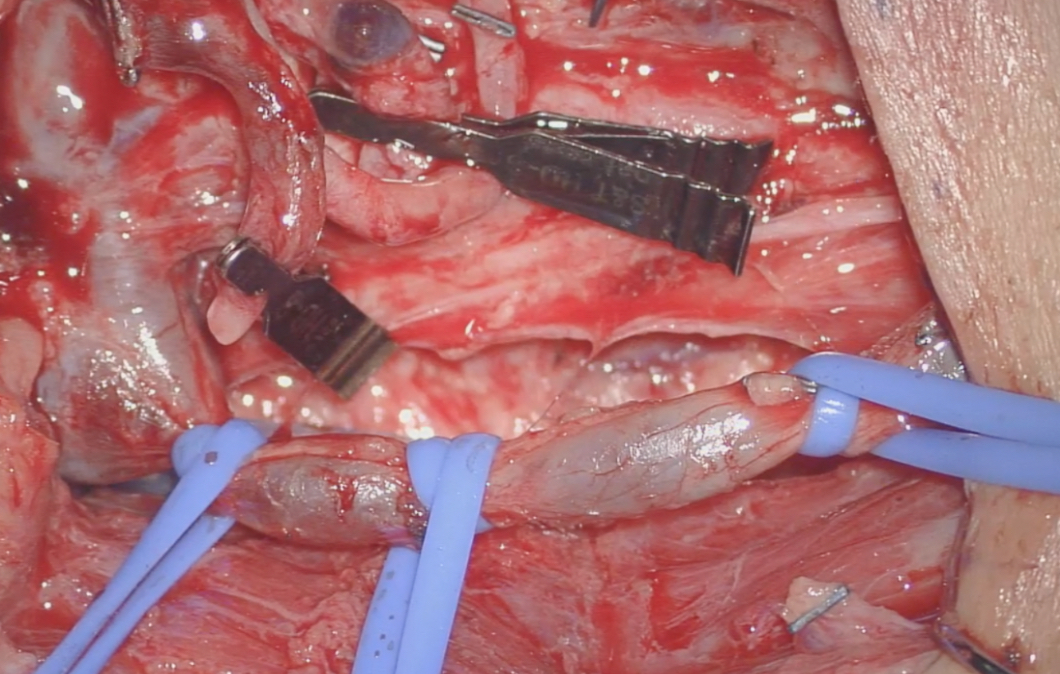
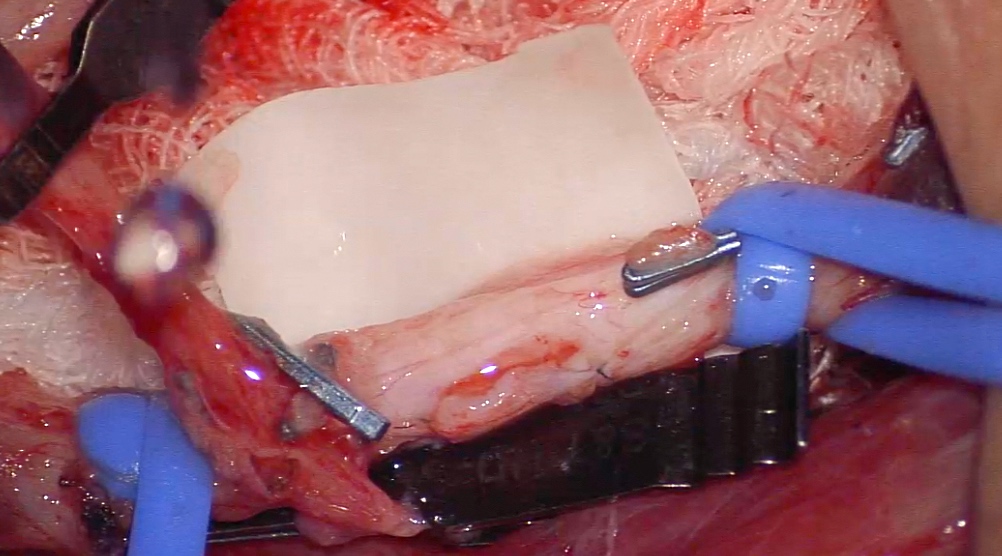
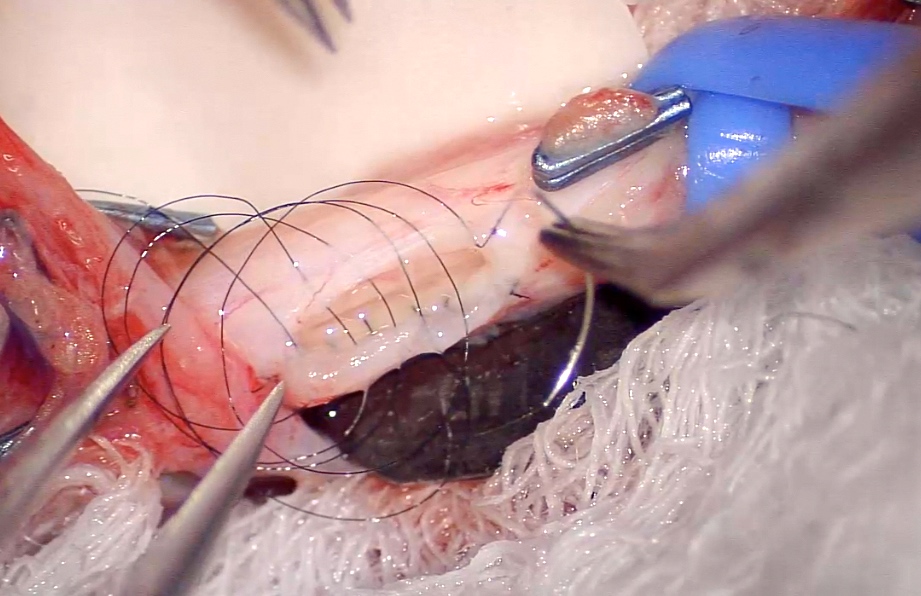
A second single microvascular clamp was applied close to the junction of anastomosis to retract the pedicle vein at 180 degrees angle laterally along the long axis of IJV to expose the posterior wall. The microvascular clamp was then secured in position with gauze or surrounding tissues (Figure 4). Left to right continuous looping technique was used for posterior wall anastomosis (Figure 5).
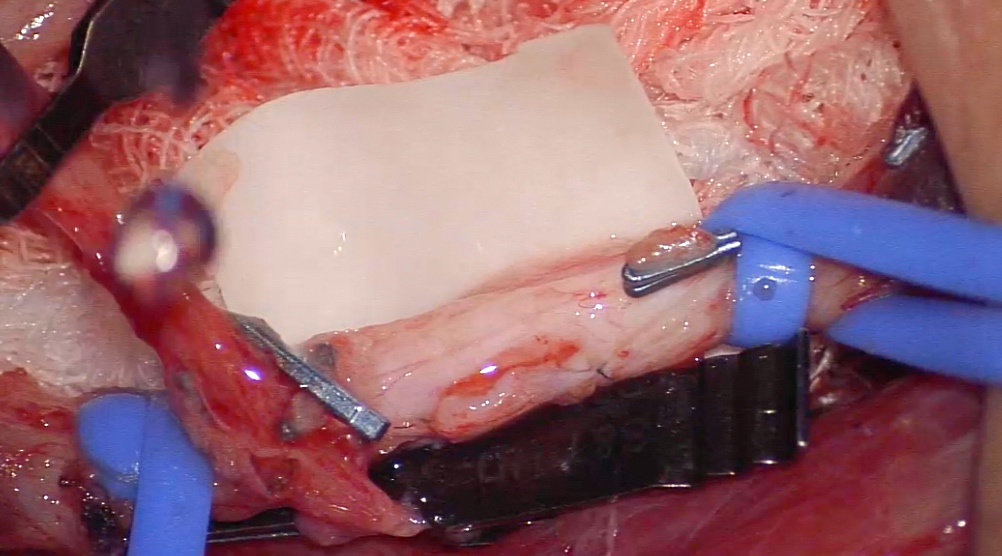
Figure 4. Maintaining an adequate position with the vascular clamp for posterior wall anastomosis, which omits any additional aid from the surgical assistant.
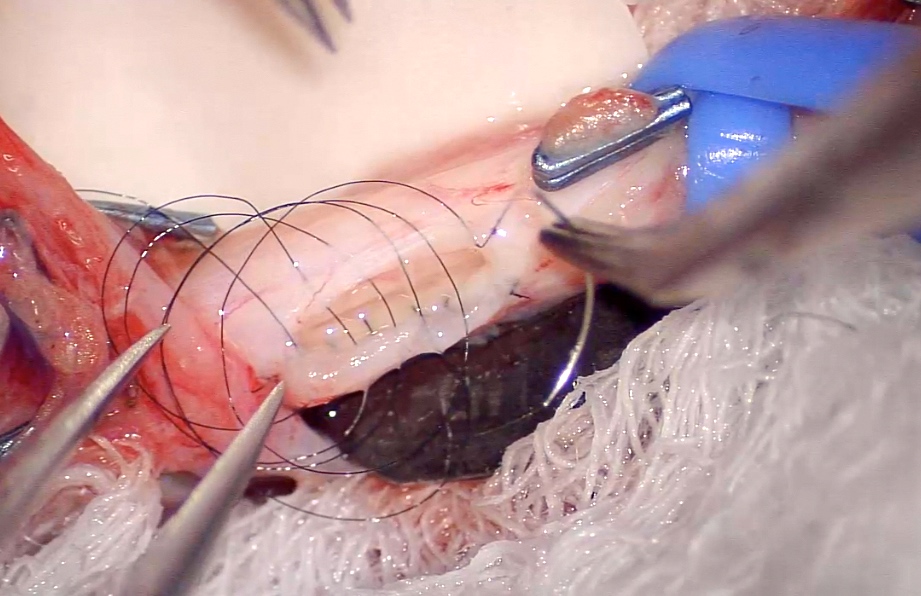
Figure 5. Demonstrating left to right continuous looping technique used for posterior wall anastomosis.
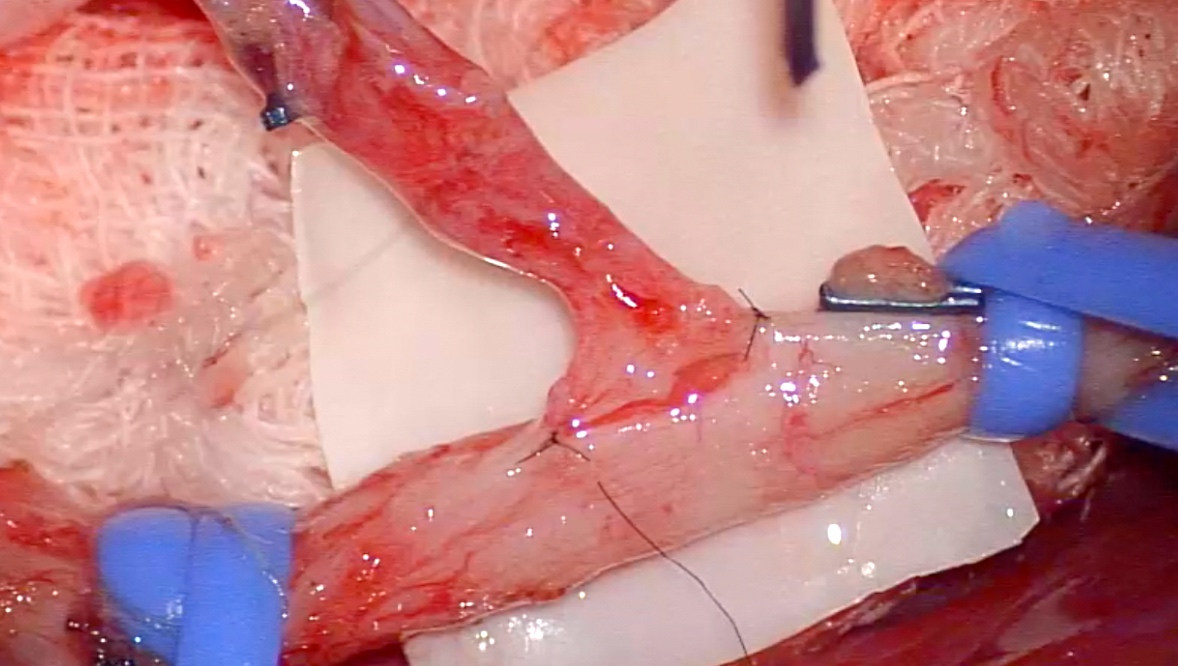
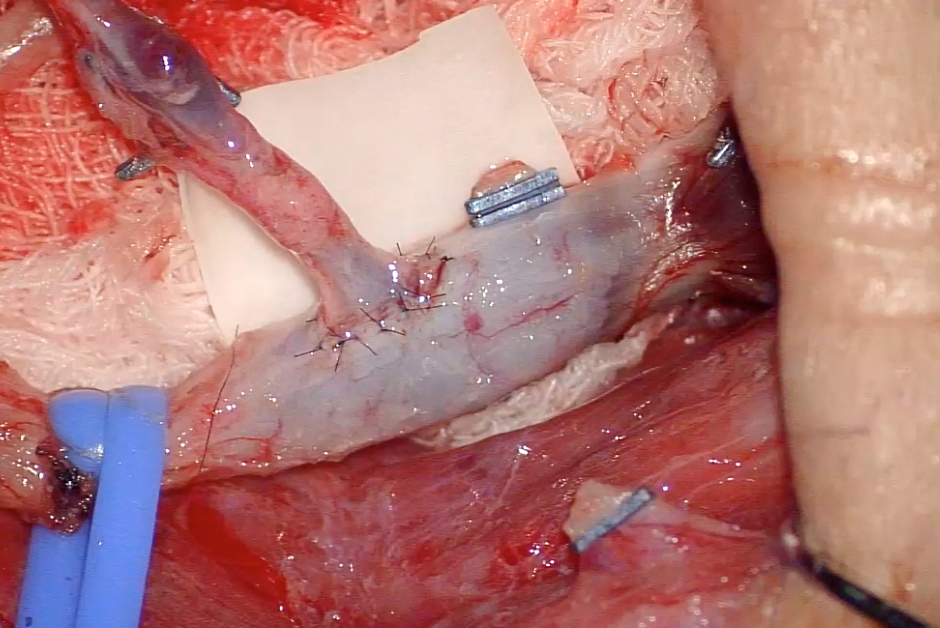
Once the anastomosis was completed, most proximal vessel loop was released. Retrograde blood flow from IJV was used for checking anastomosis leak. The proximal and distal single microvascular clamps were released sequentially to establish first venous drainage of the flap (Figure 6). Same steps were repeated for distal IJV end-to-side anastomosis achieving sequential end-to-side venous anastomoses.
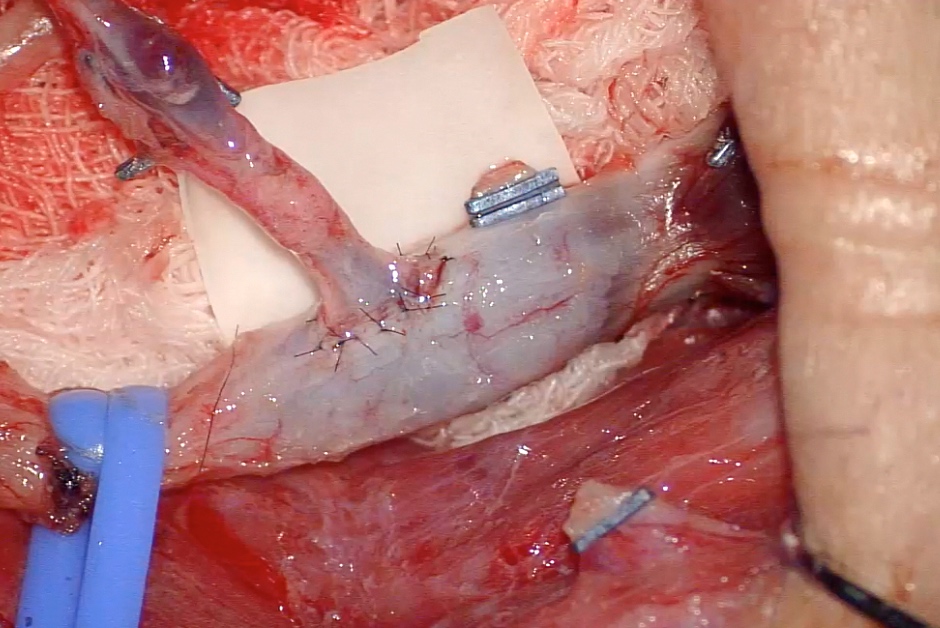
Figure 6. Sequential release of proximal and distal single vascular clamp to establish venous drainage of the flap.
The senior author Dr. Tommy Nai-Jen Chang had performed more than 30 ETS micro-venous anastomoses using this technique, with 100% success rate to date. This technique shares the same potential drawback of all forms of ETS anastomoses, as such, if ETS anastomosis revision is needed, it is more difficult than ETE anastomosis revision.
Both experimental [2-4] and clinical studies [1,5] indicate that the patency rates of venous ETE and ETS microvascular anastomoses are the same. Bas et al. [2] conducted an animal study using rat models to compare ETE and ETS microvascular anastomoses in the setting of significant vessel calibre discrepancies. The result showed a superior endothelial healing with ETS over ETE anastomosis, which was demonstrated histologically and electro-microscopically. The better the endothelium heals post anastomosis, the decreased platelet aggregation, and therefore the reduced thrombus formation and anastomosis failure.
ETS anastomosis may disrupt haemodynamics of the free flap at the site of the anastomosis theoretically. The concern was derived from potential interruption of laminated blood flow through intima propria as ETS invariably anastomosed with a sharp angle [2]. This phenomenon is presumed to be worsened in the low pressured venous system. Such intravascular haemodynamic disturbances, however, do not translate into a higher risk of anastomosis failure clinically [1,5]. Similar to Godina’s advocacy of using ETS for arterial microvascular anastomosis [6], Acland [4,7], Ueda [1], and Samaha [5] advocated the use of ETS venous microanastomosis in the setting of vesselless recipient sites, more importantly, in the presence of significant vessel size discrepancies. In our experience, ETE anastomosis should be avoided if the recipient vein is injured (from trauma/ ablation surgery/ radiation), or consists of thin walls (anterior jugular vein), or has tortuous course (superior thyroid vein). ETS should be considered in the absence of proximal veins and the veins that are poorly located for ETE, where performing anastomosis would result in vessel redundancy.
Several surgical techniques were described in the literatures aiming to simplified ETS anastomosis procedure and flattened the learning curve. Nakagawa et al. [8] modified ETS technique to maximize the exposure of posterior wall by rotating the pedicle vessel by 90 degrees clockwise after placing one anchoring suture from pedicle vessel to IJV. Yazici [9] utilized traditional triangulation method for ETS micro anastomosis. On the other hand, surgical instruments and materials had been developed since late 1970s to assist ETS anastomosis. Weinrib [10] and Karamursel [11] used external metal ring to facilitate their ETS anastomosis. Sacak [12] used two-suture fish-mouth end-to-side microvascular anastomosis with fibrin glue. Baek [13] practiced ETS anastomosis with specially designed “triple vascular clamp”, where the third clamp was used to anchor the pedicle vessel in the desirable position and angle. Recently developed anastomosis coupling devices were also trialled in ETS anastomosis clinical practice, as reported by Chernichenko and DeLacure et al. [14,15].
In Chang’s Technique of ETS micro-venous anastomosis, the utilization of three vessel loops for IJV occlusion, instead of a double vascular clamp, has got several advantages. It creates equisegmental occlusions of IJV (proximal and distal) that are independent to each other. This setup allows sequential micro-venous anastomosis without repositioning the recipient vessel (IJV) and instruments, thus saving significant surgical time. If proximal anastomosis is performed first, independent release of proximal segment of IJV is possible while distal segment remains occluded. This provides early venous drainage and restoration of normal intra-flap haemodynamics while having an undisrupted sequential ETS anastomosis for the second vein. Applying vessel loop on IJV is comparatively more vessel-protective than any forms of vascular clamp [16]. Similar to vascular clamps, complete venous occlusions of selected segments of IJV were also achieved. Vessel loops occluded IJV circumferentially and minimised IJV to its least form. This increases the surgical accessibility significantly and optimizes surgical visibility. It provides a safer and more spacious operating field, allows greater surgical manoeuvrability, and may prevent unnecessary injury to IJV.
Similar to Chang’s Technique, ETS anastomosis technique presented by Hall et al. [17] utilizes a single clamp on the pedicel vein, and uses it to retract and reveal the posterior wall by turning the clamp over and hooking behind the pedicle vessel that is held in place between the double clamps. In Chang’s Technique, a second single microvascular clamp is applied close to the anastomosis junction to retract the pedicle vein at 180 degrees angle laterally along the long axis of IJV to expose the posterior wall. Microvascular clamp is then secured in position with gauze or surrounding tissues. This maneuver self-retracts the anastomosis junction of the posterior wall, which allows the surgeon to perform ETS micro-venous anastomosis independently, and serves as the greatest advantage of this technique over others. Although this technique is created and practiced based on head and neck cases, it is also applicable in reconstruction regions where medium to large recipient vessel is present for ETS anastomosis, particularly if sequential venous anastomosis is specified. This technique, however, is difficult to apply to anastomosis regions with narrow surgical field as the maneuver generally requires sufficient space. Anastomosis to venous comitant of posterior tibial and peroneal artery, for example, will present itself as a great challenge if this technique is used.
This novel technique of sequential ETS micro-venous anastomosis is a modified technique from its classical form. The unique use of vessel loops provides protection to the vessel, while it achieves equisegmental IJV occlusion for sequential (proximal to distal) venous anastomosis. This method not only saves precious operating time from repetitive positioning of instruments and recipient vessel (IJV), but also creates a safer operating field for the microsurgeons. Utilizing a second single vascular clamp over the anastomosis junction provides an anchoring point for self-retraction by revealing and maintaining an accessible position to the posterior wall, once it is turned at 180 degrees laterally. This maneuver allows the surgeon to have full control of the surgical field and perform ETS micro-venous anastomosis confidently and independently.
Received date: April 07, 2017
Accepted date: June 05, 2017
Published date: July 02, 2017
None of the authors have financial interests in any of the products, devices, or drugs mentioned in this manuscript.
© 2017 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Video Chang’s technique of sequential end-to-side microvascular anastomosis
The authors describe various patient and breast-related factors that influence surgical outcomes while also addressing some techniques and principles for aesthetic microsurgical reconstruction.
VSG is a type of bariatric surgery that is accepted as the simplest but most efficient surgical modality to treat morbid obesity. A mouse model of VSG has been widely utilized to investigate the underlying mechanisms of VSG. There are numerous microsurgical techniques for VSG in mice, and we report herein a modified technique with 2 disposable micro-clamps to simplify the surgery.
The incidence of high-grade sinonasal adenocarcinomas of non-intestinal origin is extremely rare. In this case report, the authors present a very rare case of high-grade non-intestinal sinonasal adenocarcinoma presenting with a challenging diagnosis. Because of its significantly different prognosis, this study provides a detailed explanation of how the authors differentiate it from other sinonasal tumors. In addition, they describe how a radical endoscopic resection was applied in order to achieve a total excision.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
The PLOSEA technique detailed in this study addresses the significant challenge of managing large vessel size discrepancies in microvascular surgery with an innovative and accessible method. By partially obliterating the larger vessel lumen before anastomosis, the technique reduces risks of thrombosis and misalignment, simplifying the procedure without sacrificing effectiveness. This advancement is particularly valuable as it allows surgeons with varying levels of experience to perform complex reconstructions with greater confidence and improved patient outcomes. A key feature is the inclusion of a detailed video demonstration, providing a dynamic and comprehensive visual guide that surpasses traditional static images. This video meticulously elucidates each procedural step, enhancing understanding and facilitating the practical application of the technique. Emphasizing technical precision, patient safety, and surgical efficiency, this study offers a compelling narrative for medical professionals. The transformative impact of the PLOSEA technique on surgical practice underscores its importance, presenting a novel approach that can enhance the quality of care and expand the capabilities of microsurgeons worldwide.
This systematic review and meta-analysis provide a pragmatic evaluation of drain-free versus drain-based DIEP flap techniques for breast reconstruction, challenging the traditional reliance on drainage. By analyzing postoperative outcomes, the study highlights the potential for refining surgical strategies to enhance patient comfort and recovery without compromising safety. The findings offer a neutral perspective, suggesting that clinical practice may not necessarily depend on the use of drains. This revelation prompts medical professionals to reassess existing surgical approaches and may catalyze a paradigm shift in postoperative care. Presented with clear narrative and rigorous data analysis, the article encourages readers to consider the broader implications of surgical innovations on patient care protocols.
This report presents the first documented case of parotid NUT carcinoma with an NSD3::NUTM1 fusion, characterized by rapid metastasis and patient death five weeks post-surgery. This outcome challenges prior reports suggesting favorable survival for non-thoracic NSD3::NUTM1 tumors, indicating potential parotid-specific aggression. By integrating 13 previously published cases with the current case, the article provides a comprehensive clinicopathological reference for this rare malignancy. While further validation is required, the findings advocate for targeted NUT immunohistochemistry and molecular profiling in undifferentiated parotid tumors. BET inhibitors show therapeutic potential, underscoring the need for early recognition and precision-based care.
AI is rapidly evolving from a supportive tool into a core component of medical decision making and evidence synthesis, reshaping how clinicians interpret information at the point of care. Yet, while much of medical AI research emphasizes algorithmic performance and explainability, it seldom addresses the more practical question: how should physicians evaluate an AI recommendation in real-world, high-risk situations when fluent outputs can conceal critical errors. This Perspective offers a clinician-centered framework that treats AI outputs as provisional, testable hypotheses rather than definitive conclusions. By guiding users through premise verification, terminological precision, evidence appraisal, and causal analysis, it provides a structured defense against hallucinations, selective reporting, and data poisoning, using otolaryngology as a high-stakes, multimodal model. By placing clinical judgment at the center of AI use, this work shifts the field from passive automation toward safer, more accountable decision support grounded in patient safety.
The authors present a novel synthetic vascular model for microanastomosis training. This model is suitable for trainees with intermediate level of microsurgical skills, and useful as a bridging model between simple suturing exercise and in vivo rat vessel anastomosis during pre-clinical training.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
This article presents a case study on the successful replantation of a pediatric lower lip after a dog bite, focusing on artery-only microanastomosis. It highlights the challenges and effective strategies in pediatric microvascular surgery, particularly emphasizing the importance of specialized surgical techniques and thorough postoperative care. Alongside the case study, an extensive literature review supports the feasibility of artery-only anastomosis and the traditional yet critical use of leech therapy for managing venous congestion. This research is vital for medical professionals specializing in pediatric surgery, offering key insights into improving both functional and aesthetic outcomes for young patients. Additionally, it identifies gaps in long-term research and stresses the need for ongoing studies to refine treatment protocols, making it an indispensable resource for enhancing patient care and outcomes in pediatric reconstructive surgeries.
Authors proposed a simple innovative technique that helps in achieving a clear surgical field at the time of venous repair by diverting the venous bleeding through a glove finger and at the same time preventing venous congestion of the flap.
The PLOSEA technique detailed in this study addresses the significant challenge of managing large vessel size discrepancies in microvascular surgery with an innovative and accessible method. By partially obliterating the larger vessel lumen before anastomosis, the technique reduces risks of thrombosis and misalignment, simplifying the procedure without sacrificing effectiveness. This advancement is particularly valuable as it allows surgeons with varying levels of experience to perform complex reconstructions with greater confidence and improved patient outcomes. A key feature is the inclusion of a detailed video demonstration, providing a dynamic and comprehensive visual guide that surpasses traditional static images. This video meticulously elucidates each procedural step, enhancing understanding and facilitating the practical application of the technique. Emphasizing technical precision, patient safety, and surgical efficiency, this study offers a compelling narrative for medical professionals. The transformative impact of the PLOSEA technique on surgical practice underscores its importance, presenting a novel approach that can enhance the quality of care and expand the capabilities of microsurgeons worldwide.
This article explains the technique of end-to-side vein anastomosis by means of representative photos and a video. This is indeed an infrequent procedure in Microsurgery since the anatomical areas, like the neck, are usually rich in vascular network. The essence of the uniqueness of this procedure should be the placement of an additional vascular clamp in order to have an easy access to the posterior wall for placing the sutures. In my opinion, this is a useful method, although the originality is somewhat doubtful. There are some important aspects of the manuscript that need to be addressed:
It is written that the author has already performed this technique on more than 30 patients. Is it possible to give a description of these cases, location of the anastomosis, donor vein, and also submit this paper to another journal that accepts original papers and not only case reports?
ResponseBased on the response of the senior author, unfortunately, the data is untraceable. However, in all the cases this technique was used – pedicle vein(s) anastomosed to the internal jugular vein in end-to-side fashion– with 100% success rate. Regretfully, we are unable to present the case series in this paper.
The heading INDICATION should be rewritten as OBJECTIVE.
Response Thank you for pointing out this. Unfortunately, that section described the aim of this article instead of the indication of the technique. Thus we felt using “objective” as the title would be more appropriate.
This article explains the technique of end-to-side vein anastomosis by means of representative photos and a video. This is indeed an infrequent procedure in Microsurgery since the anatomical areas, like the neck, are usually rich in vascular network. The essence of the uniqueness of this procedure should be the placement of an additional vascular clamp in order to have an easy access to the posterior wall for placing the sutures. In my opinion, this is a useful method, although the originality is somewhat doubtful. There are some important aspects of the manuscript that need to be addressed:
It is written that the author has already performed this technique on more than 30 patients. Is it possible to give a description of these cases, location of the anastomosis, donor vein, and also submit this paper to another journal that accepts original papers and not only case reports?
ResponseBased on the response of the senior author, unfortunately, details of the patients and data are untraceable, and hence unable to be presented. Regretfully, we are unable to present the case series in this paper. Nevertheless, all cases that received sequential ETS anastomosis with Chang’s Technique were free flap reconstruction in head and neck region post oncological ablation between 2010 and 2017. Venous choices for the anastomosis are pedicle veins (most commonly venous comitantes of descending or oblique branch of lateral circumference artery) to internal jugular vein. The post-operative anastomosis patency rate was 100% and none of them needed any re-exploration for vascular complications.
The heading INDICATION should be rewritten as OBJECTIVE.
Response Thank you for your comment. Changing the heading from “indication” to “objective” is certainly more appropriate for the section of the writing and will guide the audience in a more assertive manner. Corresponding changes are being made based on your suggestion.
Hsieh YH, Lee CH, Kwon SH, Chang TNJ. Chang’s technique of sequential end-to-side microvascular anastomosis: Technique of sequential end-to-side anastomosis. Int Microsurg J 2017;1(1):4. doi:10.24983/scitemed.imj.2017.00021