Objective: This meta-analysis evaluates the efficacy of drainless versus drain-based deep inferior epigastric perforator (DIEP) flap techniques in breast reconstruction, focusing on postoperative complications and outcomes. It aims to provide evidence-based recommendations to optimize surgical strategies and improve patient results.
Methods: Adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we searched PubMed, ScienceDirect, Scopus, and Google Scholar on June 12, 2024, for interventional studies that reported on complications in DIEP flap reconstructions with and without drains. We included peer-reviewed, full-text articles published in English, without restrictions on the year of publication. A random-effects meta-analysis was performed to compute pooled risk ratios and incidences with 95% confidence intervals (CIs). Heterogeneity was evaluated using I². The study protocol was registered in the PROSPERO database under registration number CRD42024588015.
Results: This analysis incorporated four studies published between 2015 and 2024, with a total of 603 participants. Of these, 303 underwent procedures with drains, while 300 underwent reconstructions without drains. The pooled incidence of hematoma was 0.01 (95% CI: 0.00 to 0.52) for the group with drains and 0.00 (95% CI: 0.00 to 1.00) for the group without, with no events reported in the latter, thus precluding risk ratio calculations. The pooled incidence of seroma was 0.04 (95% CI: 0.01 to 0.12) in the group with drains compared to 0.05 (95% CI: 0.02 to 0.15) in the group without drains. This resulted in a pooled risk ratio of 1.39 (95% CI: 0.06 to 33.44), with moderate heterogeneity (I² = 55%, p = 0.11). The pooled incidence of wound dehiscence was 0.09 (95% CI: 0.00 to 0.84) in the group with drains and 0.12 (95% CI: 0.00 to 0.92) in the group without, yielding a pooled risk ratio of 1.23 (95% CI: 0.94 to 1.61), with no heterogeneity (I² = 0%, p = 0.96). Infection rates, reported in only one study, showed a higher incidence in the group with drains (7.8%) compared to the group without (4.8%), though the data were insufficient for pooled analysis.
Conclusion: This DIEP-specific meta-analysis reveals that, while definitive superiority of drainless techniques is not established, these approaches can achieve outcomes comparable to traditional drain-based methods. These methods represent a viable and safe option in appropriate clinical settings, underscoring the need for individualized clinical decisions based on patient comfort, resource availability, and logistical considerations. Continued research is critical to further assess long-term outcomes, infection risks, cost-effectiveness, and patient-reported outcomes to provide robust evidence-based recommendations for optimal management of DIEP flap donor sites.
Flap techniques that utilize abdominal tissue for breast reconstruction include the latissimus dorsi (LD), superficial inferior epigastric artery (SIEA), transverse rectus abdominis myocutaneous (TRAM), and deep inferior epigastric perforator (DIEP) flaps [1]. The LD flap is known for its limited volume for implant coverage and a high risk of seroma formation [2]. In contrast, the SIEA flap, similar to the DIEP flap, frequently encounters problems with vascularization due to its dependence on small-caliber blood vessels [2].
The TRAM flap offers better cosmetic outcomes and improved vascularization but requires extensive preoperative preparation. It is also associated with several risks, including abdominal muscle weakness, an increased risk of hernia, prolonged recovery periods, and heightened postoperative complications [1].
DIEP Flap Advantages
The DIEP flap has become the preferred technique for breast reconstruction, particularly following mastectomy, due to its superior outcomes [3]. This method involves transferring skin, fat, and the inferior epigastric perforator artery from the abdominal region while preserving muscle integrity. It surpasses other methods by providing improved cosmetic results, fewer complications, reduced recovery times, minimal breast scarring, and a lower likelihood of requiring secondary surgeries [3].
Postoperative Complications
Despite its advantages, the DIEP flap can still lead to several potential postoperative complications, such as hematoma, seroma, wound dehiscence, and infection. The most common issue, seroma, involves the accumulation of serous fluid in the dead space created during surgery. This complication results from an acute inflammatory response to surgical trauma, which is exacerbated by impaired lymphatic and vascular drainage [4].
While the initial inflammatory response is critical for wound healing, persistent seroma formation can delay this process, increase the risk of infection, and sometimes necessitate medical intervention. To mitigate seroma risks, surgeons often employ drains that create negative pressure [5]. However, recent studies have indicated that drainless methods, such as progressive tension sutures (PTS), can effectively prevent fluid accumulation. These studies report outcomes between drainless and drained DIEP flaps that are comparably effective [6,7]. This growing body of research adds to the extensive discourse surrounding the DIEP flap, which has been a significant focus in the surgical literature since its first description in 1989 [8].
Research Gap
Although the DIEP flap has been extensively discussed in the literature, systematic reviews or meta-analyses that thoroughly examine differences in postoperative complications between drainless and drain-based approaches are scarce. Prior attempts to address these comparisons include a conference abstract by Wong and Chansiriwongs [9], which analyzed drain versus drainless donor-site closure techniques in DIEP flap reconstruction across 580 patients. This study reported no significant differences in seroma, hematoma, or wound dehiscence. However, the abstract format lacked methodological transparency and detailed statistical analysis, such as pooled effect estimates, and as of April 2025, it remains unpublished in a peer-reviewed journal.
Another study by Khan et al. reviewed 327 patients undergoing abdominal flap reconstruction, including both DIEP and TRAM flaps [10]. This broader scope, along with limited heterogeneity reporting, outdated literature (search ended in August 2020), and a modest sample size, diminishes the relevance of its conclusions to DIEP-specific practices. These studies illustrate persistent gaps in the literature, highlighting the need for DIEP-focused meta-analyses that can clarify contradictory findings, standardize complication definitions, and reinforce the evidence base regarding the necessity of drainage.
Study Aim
This study aimed to conduct the first comprehensive meta-analysis dedicated exclusively to comparing postoperative outcomes between drainless and drain-based DIEP flap reconstructions. The analysis was rigorously designed to elucidate the impacts of different drainage strategies on the outcomes of DIEP flap surgeries, thereby guiding clinical decision-making. The objective was to leverage robust, peer-reviewed data to derive recommendations that could significantly enhance patient care in breast reconstruction.
Study Design
We conducted this systematic review in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11]. Our methodology ensures transparency, reproducibility, and strict adherence to scientific standards for evaluating postoperative outcomes of DIEP flap reconstruction.
Protocol Registration
We prospectively registered the study protocol in PROSPERO, the International Prospective Register of Systematic Reviews (registration number: CRD42024588015). This registration confirmed our compliance with established methodological standards, thus enhancing the credibility, transparency, and reproducibility of our research. By adhering to these best practices, we aimed to minimize potential biases and ensure alignment with rigorous scientific standards.
Eligibility Criteria
We applied the Population, Intervention, Comparison, and Outcome (PICO) framework to structure the selection criteria for this study. The population consisted of patients who underwent DIEP flap reconstructions. We focused on comparing two groups for our intervention and comparison: patients receiving drainless DIEP flap reconstructions and those undergoing reconstructions with drains. Our primary focus was on evaluating postoperative complications, including hematoma, seroma, infection, and wound dehiscence.
Exclusion Criteria
We excluded studies that were duplicate publications, earlier versions of studies without new findings, or studies from the same cohort with differing follow-up durations where only the publication with the longest follow-up was included. We also excluded articles that were inaccessible, published in non-peer-reviewed journals, lacked primary data, involved fewer than five subjects, did not focus on patients undergoing DIEP flap reconstruction, failed to investigate drainless techniques, or did not report on postoperative complications. We considered only peer-reviewed studies published in English, imposing no restrictions on the publication year to ensure a comprehensive data set.
Literature Search Strategy
On June 12, 2024, we conducted a comprehensive literature search using PubMed, ScienceDirect, and Scopus. The objective was to identify interventional studies comparing postoperative complications between drainless and drain-based techniques in DIEP flap breast reconstruction. To enhance the efficiency of the search in Scopus, we employed the Publish or Perish software (version 8.6.4198.8332).
We used a combination of controlled vocabulary and free-text terms relevant to breast reconstruction, DIEP flaps, drainage strategies, and postoperative outcomes. Boolean operators were applied to structure the search. The strategy was tailored to each database, considering platform-specific syntax and indexing. We restricted the search to English-language publications and applied no limitations on publication year to ensure comprehensive coverage.
Screening and Selection of Studies
We imported search results from PubMed, ScienceDirect, and Scopus into Rayyan, a web-based platform tailor-made for the systematic screening of reviews (for more information, visit https://www.rayyan.ai). This platform proved essential in identifying and manually removing potential duplicates, streamlining the initial stages of our systematic review.
Following the deduplication phase, Christian S and Suteja RC, who acted as independent reviewers, meticulously screened titles and abstracts to assess the eligibility of the studies. They engaged in thorough discussions to resolve any discrepancies, ensuring the selection process remained both objective and consistent.
In the subsequent phase, Suteja RC endeavored to retrieve the full texts of the studies that had passed the initial eligibility screening. Studies that were not accessible were systematically excluded. Thereafter, both reviewers conducted in-depth reviews of the full texts, rigorously applying the predefined inclusion and exclusion criteria. They collaboratively resolved any disagreements that arose during this phase, thereby maintaining the methodological integrity of the study selection process.
Data Extraction and Synthesis
Christian S and Suteja RC, two independent researchers, manually extracted data from the eligible studies and recorded this information in standardized Microsoft Excel spreadsheets (Microsoft Corporation, Redmond, Washington, USA). They resolved any discrepancies or uncertainties through discussions to guarantee accuracy and consistency in the data compilation.
The data extraction encompassed study characteristics, subject demographics, surgical details, and outcome measures. Specifically, the study characteristics included the first author's name, year of publication, and the country of the study. Subject demographics covered the number of participants, their ages, body mass index (BMI), and smoking status. Surgical details were centered around the reconstruction approach utilized in each study, while the outcome measures focused on the evaluation methods employed and the incidence of reported complications, such as hematoma, seroma, infection, and wound dehiscence.
For instances where multiple publications originated from the same patient cohort, we included only the data from the publication with the longest follow-up period to ensure consistency across the dataset. When different publications presented unique follow-up data at various time points, we selected the most comprehensive dataset to avoid duplication of data.
Outcome Variables
In this study, we categorized postoperative outcomes into major and minor complications based on their clinical relevance and the consistency of data reporting. We identified hematoma, seroma, infection, and wound dehiscence as major complications due to their frequent occurrence in studies and significant impact on surgical recovery. We quantitatively analyzed these complications to assess and compare rates between drain-based and drainless DIEP flap reconstructions.
We also documented minor complications, such as delayed wound healing, fat necrosis, abdominal bulge, and umbilical necrosis, when data were available. However, we excluded these from the meta-analysis due to their sporadic reporting and heterogeneous outcome definitions across studies. This selective approach allowed us to focus our statistical synthesis, ensuring the reliability of our findings while capturing a broad spectrum of clinical insights from the literature.
Statistical Analysis
We conducted a random-effects meta-analysis to estimate pooled proportions with a 95% confidence interval (CI). We analyzed the pooled risk ratios of complications between drain-based and drainless DIEP flap reconstructions using the generalized linear mixed model (GLMM) method. To assess heterogeneity across studies, we calculated the I² statistic and categorized heterogeneity as low (I² < 25%), moderate (I² = 26–75%), or high (I² > 75%). Forest plots were generated to visualize effect estimates and heterogeneity levels.
We evaluated potential publication bias using funnel plots and Egger’s test. Additionally, we performed a subgroup analysis to further compare outcomes between drain-based and drainless groups. All statistical analyses were conducted using RStudio (version 2023.6.2+561, R Foundation for Statistical Computing, Vienna, Austria).
Risk of Bias Assessment
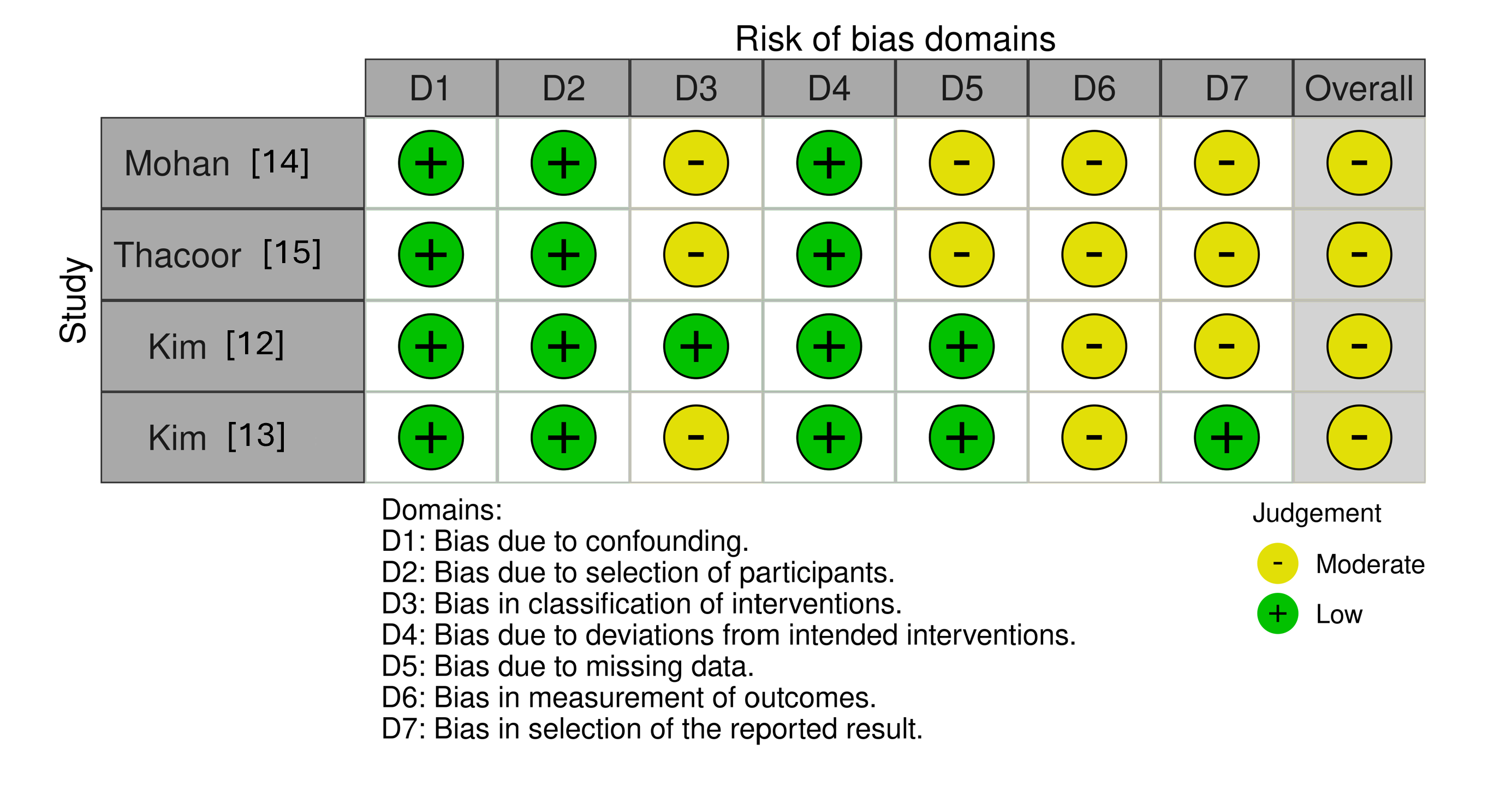
We assessed the risk of bias in all included studies using validated tools tailored to the specific study designs. Two independent reviewers, Christian S and Suteja RC, utilized the Cochrane Risk of Bias 2 tool (RoB 2) for randomized controlled trials, and the Risk Of Bias In Non-randomized Studies of Interventions tool (ROBINS-I) for observational studies. The ROBINS-I tool systematically evaluates bias across seven domains: confounding, participant selection, classification of interventions, deviations from intended interventions, missing data, outcome measurement, and selection of reported results.
Any disagreements between reviewers were resolved through discussion or, when necessary, consultation with a third reviewer. We employed the Robvis tool to create visual representations of the risk of bias assessments, including traffic light plots and summary plots. These visual aids enhance the transparency and standardization of our judgments, making our methodological assessment clear and accessible.
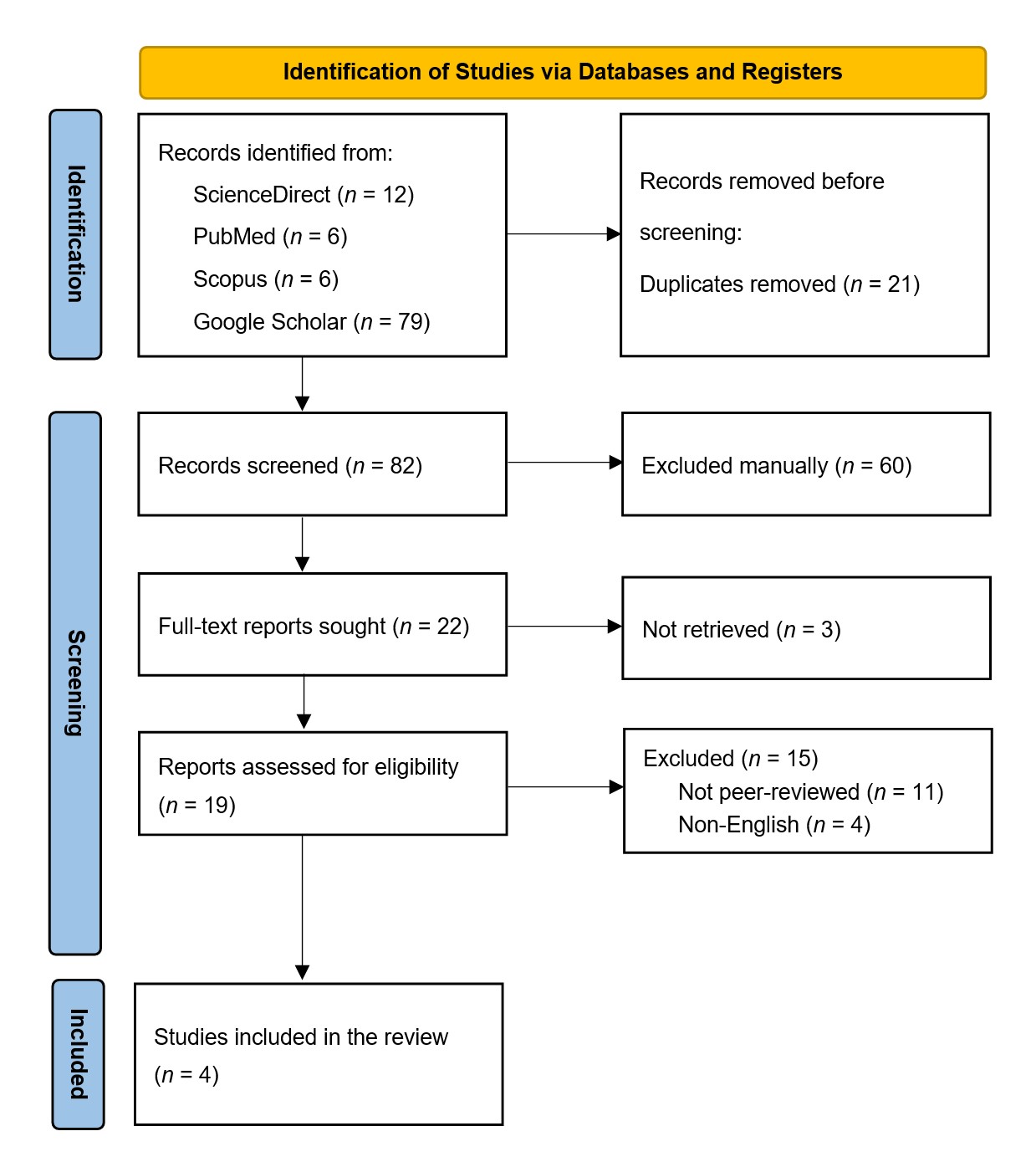
Study Selection
The PRISMA flow diagram that illustrates the study selection process appears in Figure 1. We initially identified 103 studies from various sources: 12 from ScienceDirect, 6 from PubMed, 6 from Scopus, and 79 from Google Scholar. After removing 21 duplicates, we screened 82 studies by reviewing titles and abstracts to check their alignment with the defined objectives, population, interventions, comparisons, and outcomes. We excluded studies that did not directly relate to the research question, targeted different populations, or utilized inappropriate study designs, resulting in the removal of 60 studies.
We further excluded three studies due to the unavailability of their full texts. Additionally, we excluded 11 studies for lacking peer review, an essential factor in ensuring the credibility and reliability of the findings. We also excluded four studies published in non-English languages, adhering to the review's restriction to English-language publications. Ultimately, only four studies met all eligibility criteria and were included for further synthesis and analysis [12–15].
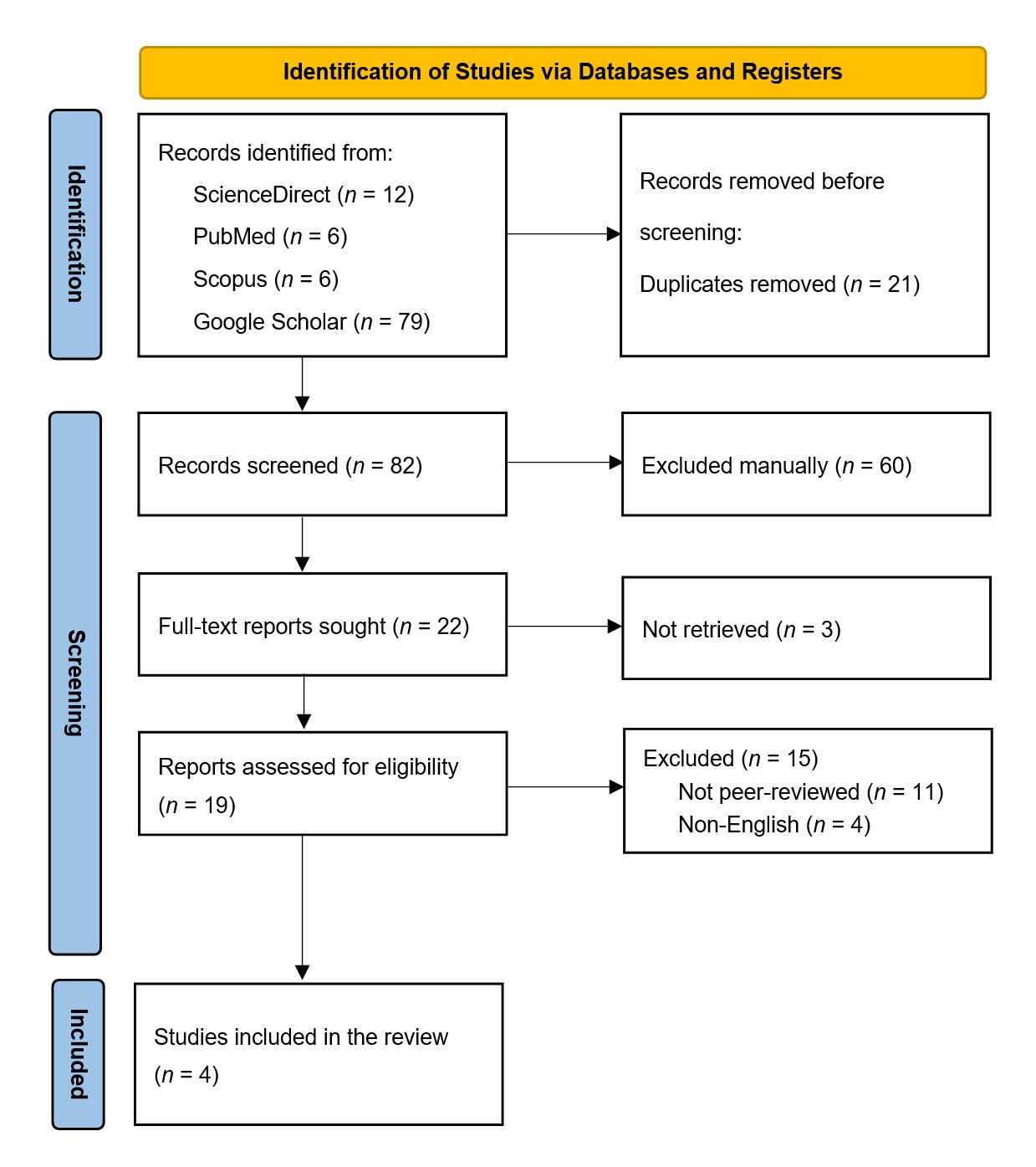
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of study selection. This diagram illustrates the process by which studies are identified and selected. The database search initially identifies 103 records, including 12 from ScienceDirect, 6 from PubMed, 6 from Scopus, and 79 from Google Scholar. After 21 duplicates are removed, screeners review the titles and abstracts of 82 records, and 60 are excluded for not aligning with the study’s objectives, population, interventions, comparisons, and outcomes. Efforts to retrieve full-text reports for 22 records result in 3 not being obtained. Of the 19 reports assessed for eligibility, 15 are excluded due to lack of peer review or because they are published in languages other than English. Ultimately, 4 studies meet all eligibility criteria and are included in the systematic review.
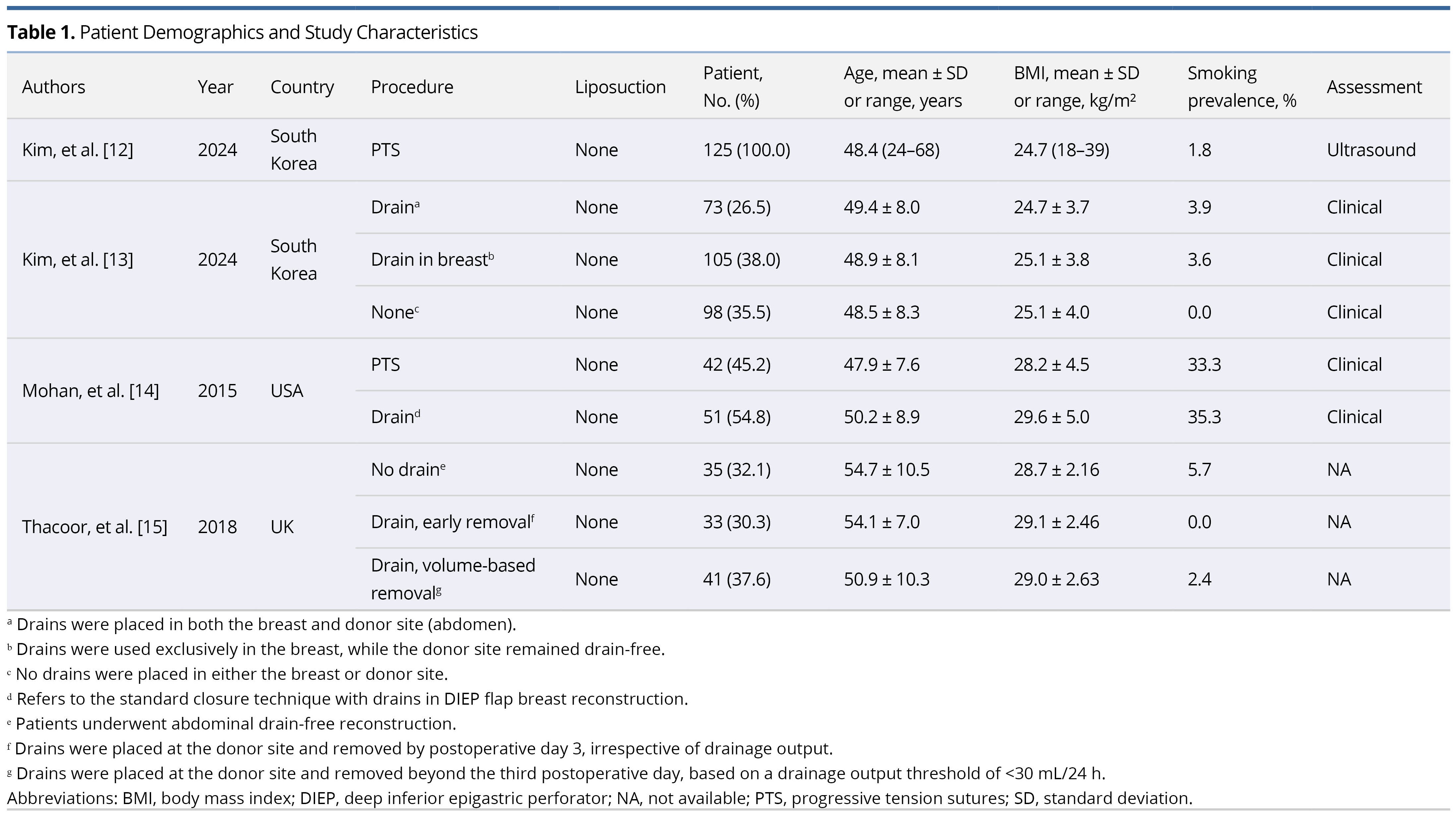
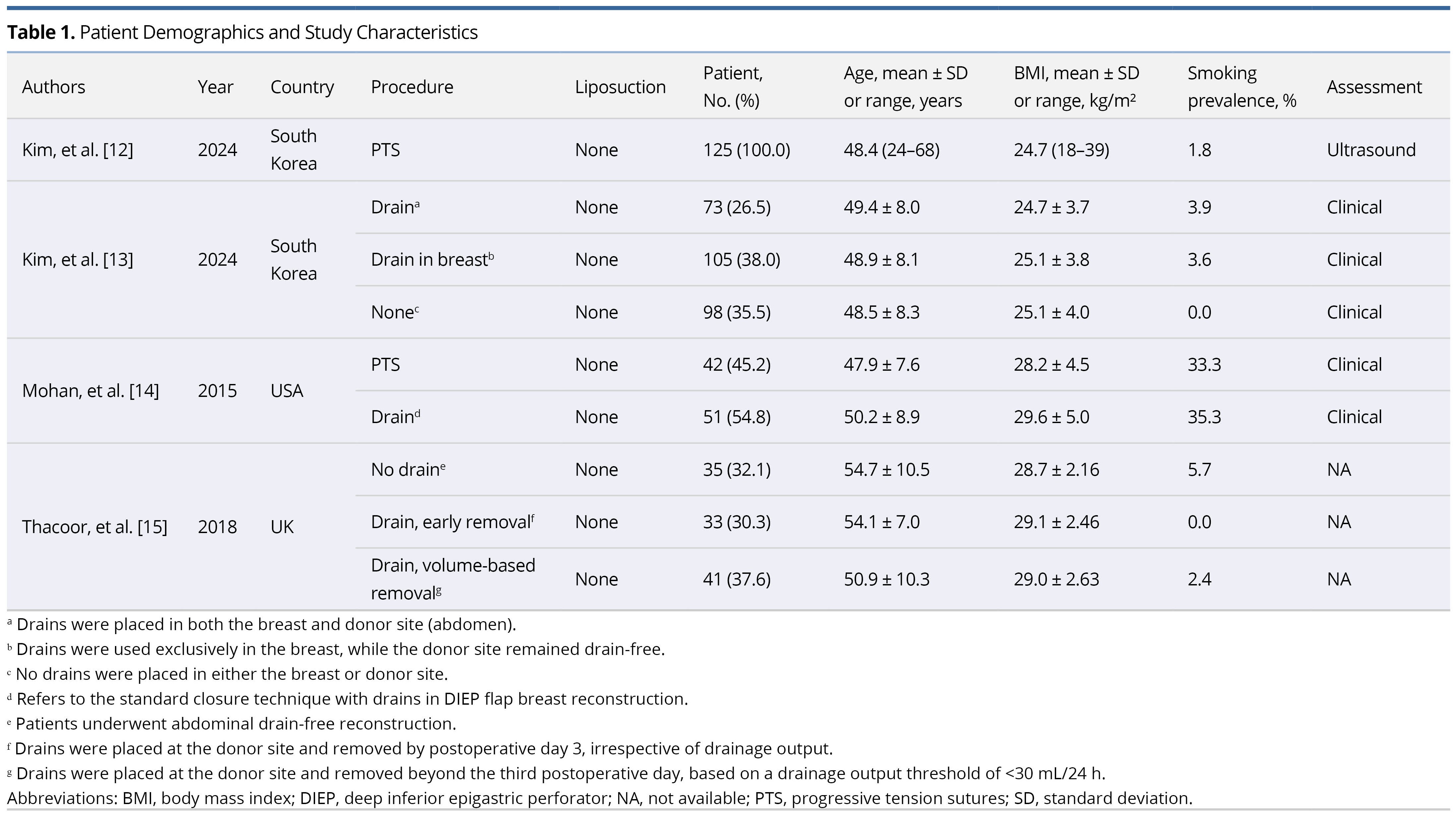
Study Profile and Demographics
This analysis incorporated data from 603 participants across four studies published between 2015 and 2024 (Table 1). Conducted in three countries, these studies included two based in South Korea, one in the United States, and one in the United Kingdom. The international scope of the studies enhances the generalizability of the findings, although variations in surgical techniques, healthcare infrastructure, and perioperative protocols may introduce outcome variability.
Standardized surgical procedure
Each study employed DIEP flaps for breast reconstruction. Among the participants, 300 underwent drain-based procedures, and 303 experienced drainless techniques. Variations in drain management included the use of drains at the breast or donor site, early removal, and volume-based thresholds. In contrast, drainless groups utilized techniques like PTS or direct closure without any drainage. Notably, none of the cohorts used adjunctive liposuction, ensuring consistency in donor-site management and facilitating reliable comparisons between surgical approaches.
Age distribution
Participant ages across the studies ranged from 24 to 68 years, predominantly clustering between 47.9 and 54.7 years. This age distribution is typical for patients undergoing autologous breast reconstruction, supporting the comparability of patient demographics across studies.
BMI distribution
Mean BMI values ranged from 24.7 to 29.6 kg/m² across the studies, placing most participants in the normal to overweight categories, with some approaching the obesity threshold. This consistency in BMI supports the comparability of surgical outcomes by minimizing confounding related to body composition.
Smoking prevalence
Generally, smoking prevalence was low across the studies, with most cohorts reporting rates from 0.0% to 5.7%. However, Mohan’s 2015 study [14] reported significantly higher rates, with 33.3% in the PTS group and 35.3% in the drain-based group, suggesting population-specific differences or unique recruitment characteristics.
Patient grouping
Kim et al. [12] studied 125 patients undergoing PTS. In a subsequent analysis, Kim et al. [13] categorized 276 patients into three distinct groups: 73 (26.5%) received drainage at both the breast and donor sites, 105 (38.0%) had drains only at the breast, leaving the donor site drain-free, and 98 (35.5%) had no drains at either site. Mohan et al. [14] evaluated 93 patients; 42 (45.2%) underwent PTS, while 51 (54.8%) had standard closures with drains during DIEP flap breast reconstruction. Thacoor et al. [15] included 109 patients, distributed as follows: 35 (32.1%) underwent abdominal drain-free reconstruction, 33 (30.3%) had donor-site drains removed by the third postoperative day regardless of output, and 41 (37.6%) had donor-site drains removed after the third day, contingent on a drainage output threshold of less than 30 mL per 24 hours.
Evaluation methods
The methods of evaluation varied among the studies. One study employed ultrasound imaging as the primary assessment tool [12], while two others relied solely on clinical evaluations [13,14]. The assessment method for the remaining study was unspecified [15].
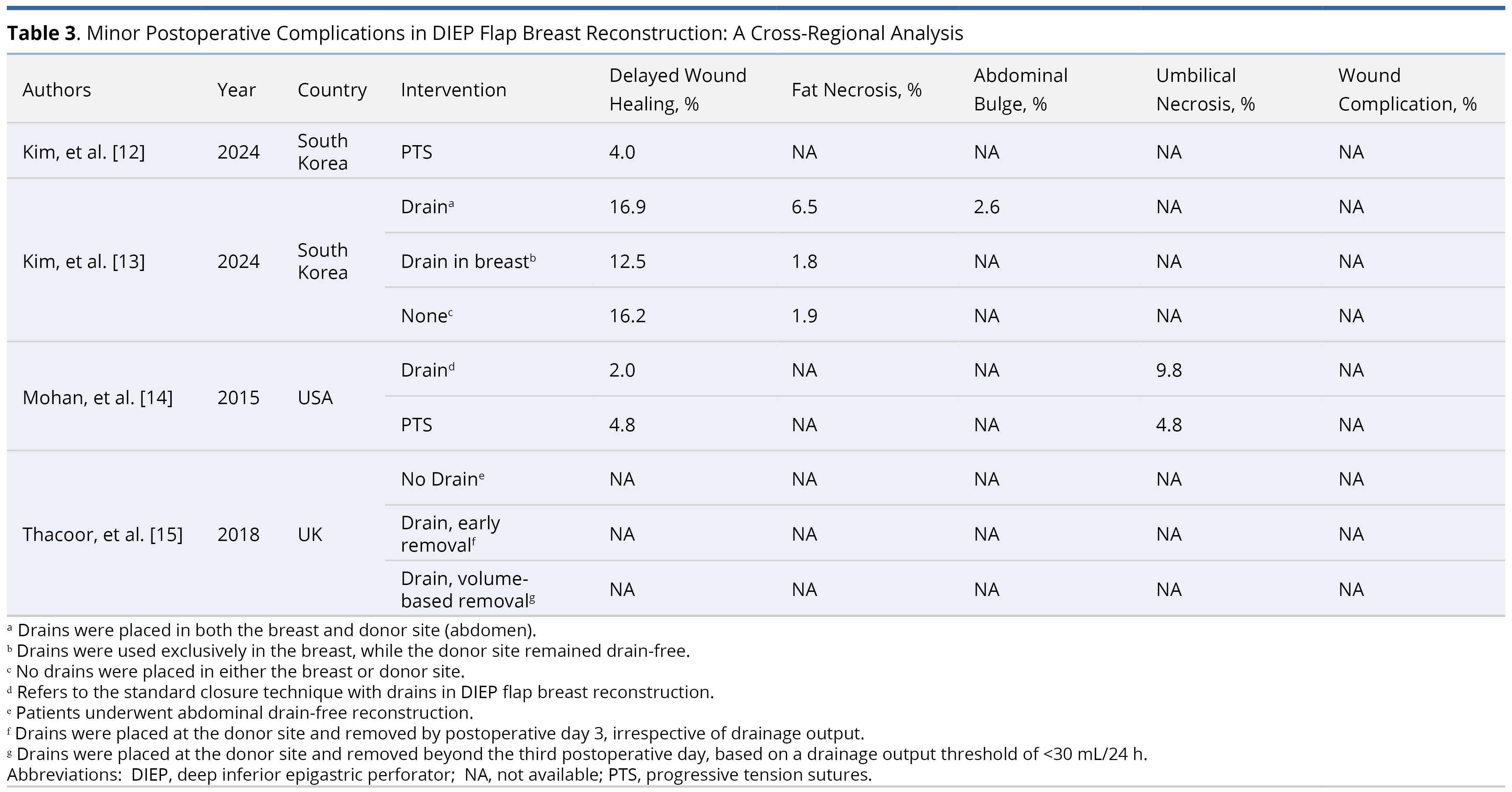
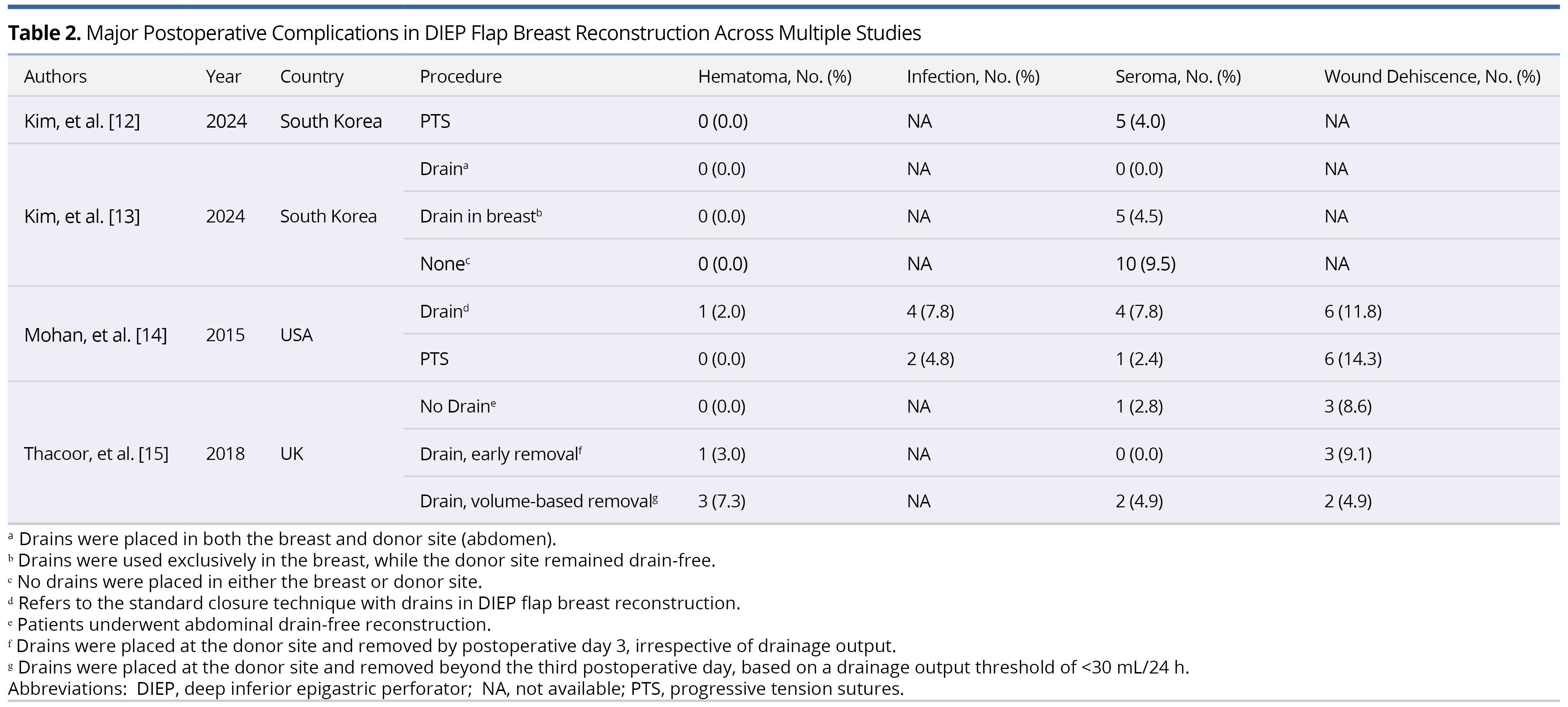
Postoperative Complications Across Studies
Tables 2 and 3 summarize postoperative complications identified in four studies conducted between 2015 and 2024. These studies were performed in South Korea, the United States, and the United Kingdom, and examined both major and minor adverse outcomes following DIEP flap breast reconstruction. This dataset provides a basis for examining complication profiles across varying surgical practices and institutional protocols.
Among the major complications, we observed substantial variability in the incidence of hematoma, infection, seroma, and wound dehiscence (Table 2). Hematoma rates ranged from 0% to 7.3%, with higher rates (3.0–7.3%) observed in groups employing volume-based or early drain removal protocols, suggesting a potential association between drain use and hematoma formation. Infection was documented in only one study [14], which reported a higher rate in the drain group (7.8%, 4 cases) compared to the PTS group (4.8%, 2 cases). The absence of reported infection rates in other studies limits the ability to draw broader conclusions. Seroma incidence ranged from 0% to 9.5%, peaking in a no-drain group, indicating a possible increased risk with drain omission. Wound dehiscence rates ranged from 4.9% to 14.3%. The highest rate (14.3%) was observed in a group using PTS [14], while early drain removal was associated with a 9.1% rate [15]. Data on wound dehiscence were not reported in two studies, limiting the ability to make broader comparisons [12,13].
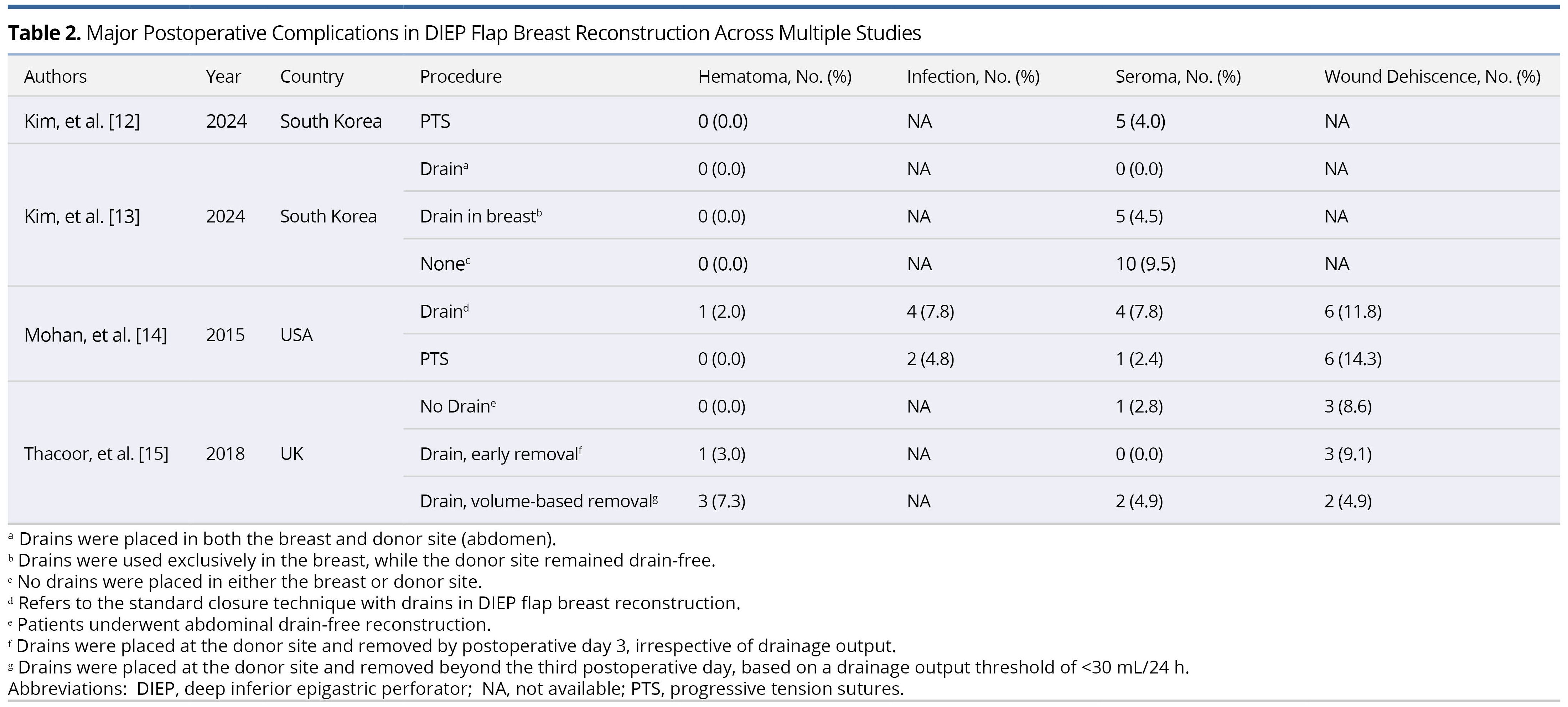
Minor complications were also recorded (Table 3), comprising delayed wound healing, fat necrosis, abdominal bulge, umbilical necrosis, and other wound-related complications. Delayed wound healing ranged from 2.0% to 16.9%, with the highest rate observed in patients who received drains at both the breast and donor sites [13]. Notably, PTS groups demonstrated lower rates (4.0–4.8%). Fat necrosis ranged from 1.8% to 6.5%, with the highest rate in the drain group [13], although most studies failed to report this outcome, the ability to draw broader conclusions remains limited. Abdominal bulge (2.6%) [13] and umbilical necrosis (4.8–9.8%) [14] were each reported in only one study and were more frequent in drain groups. No other wound-related complications were reported in any of the included studies.
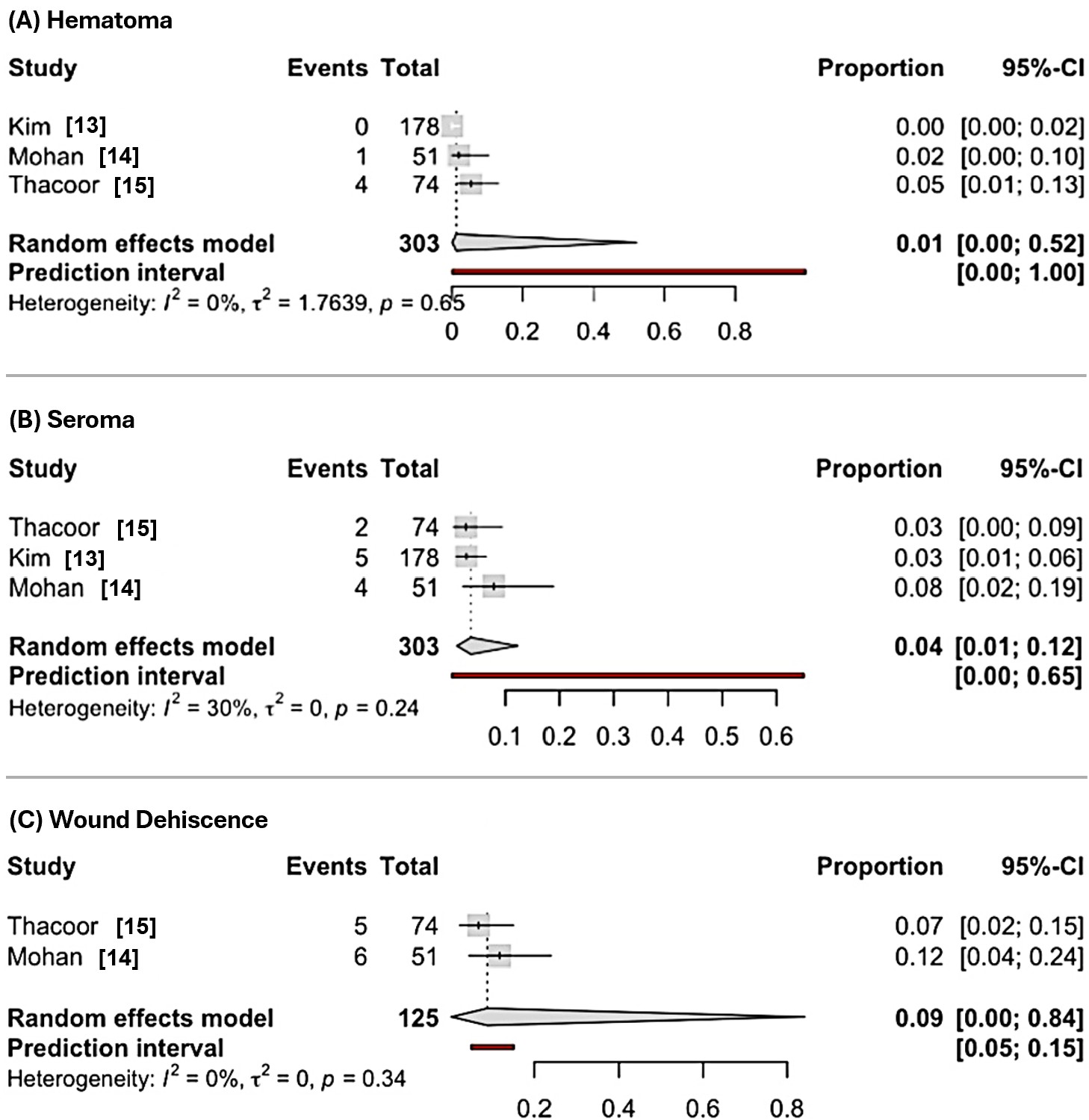
Hematoma Incidence Analysis
This meta-analysis evaluated the incidence of hematoma in DIEP flap breast reconstruction, involving a total of 603 participants across seven studies. In the drain-based group, which included data from three studies with 303 subjects (Figure 2A), the pooled incidence of hematoma was 0.01 (95% CI: 0.00 to 0.52) using a random effects model, with no heterogeneity observed (I² = 0%, p = 0.65). A random effects model was chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05).
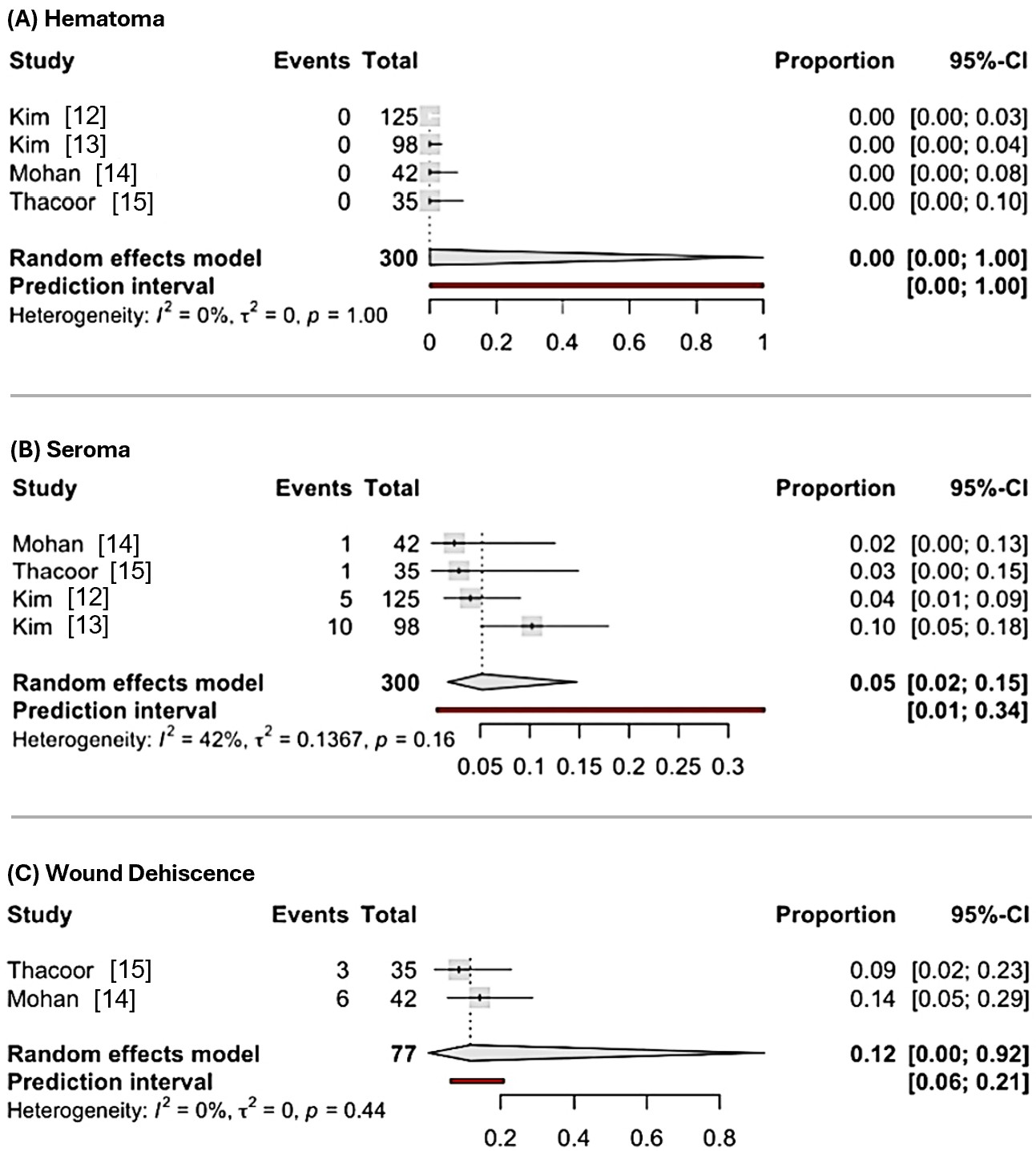
Conversely, the drainless group, comprising data from four studies with 300 subjects (Figure 3A), had a pooled hematoma incidence of 0.00 (95% CI: 0.00 to 1.00) using a random effects model, also with no heterogeneity (I² = 0%, p = 1.00). A random effects model was selected for consistency in analysis, despite the lack of statistical significance in heterogeneity (p > 0.05).
A risk ratio analysis for hematoma incidence was not conducted, as all studies in the drainless DIEP flap reconstruction group reported zero hematoma events, indicating an extremely low event rate within this cohort.
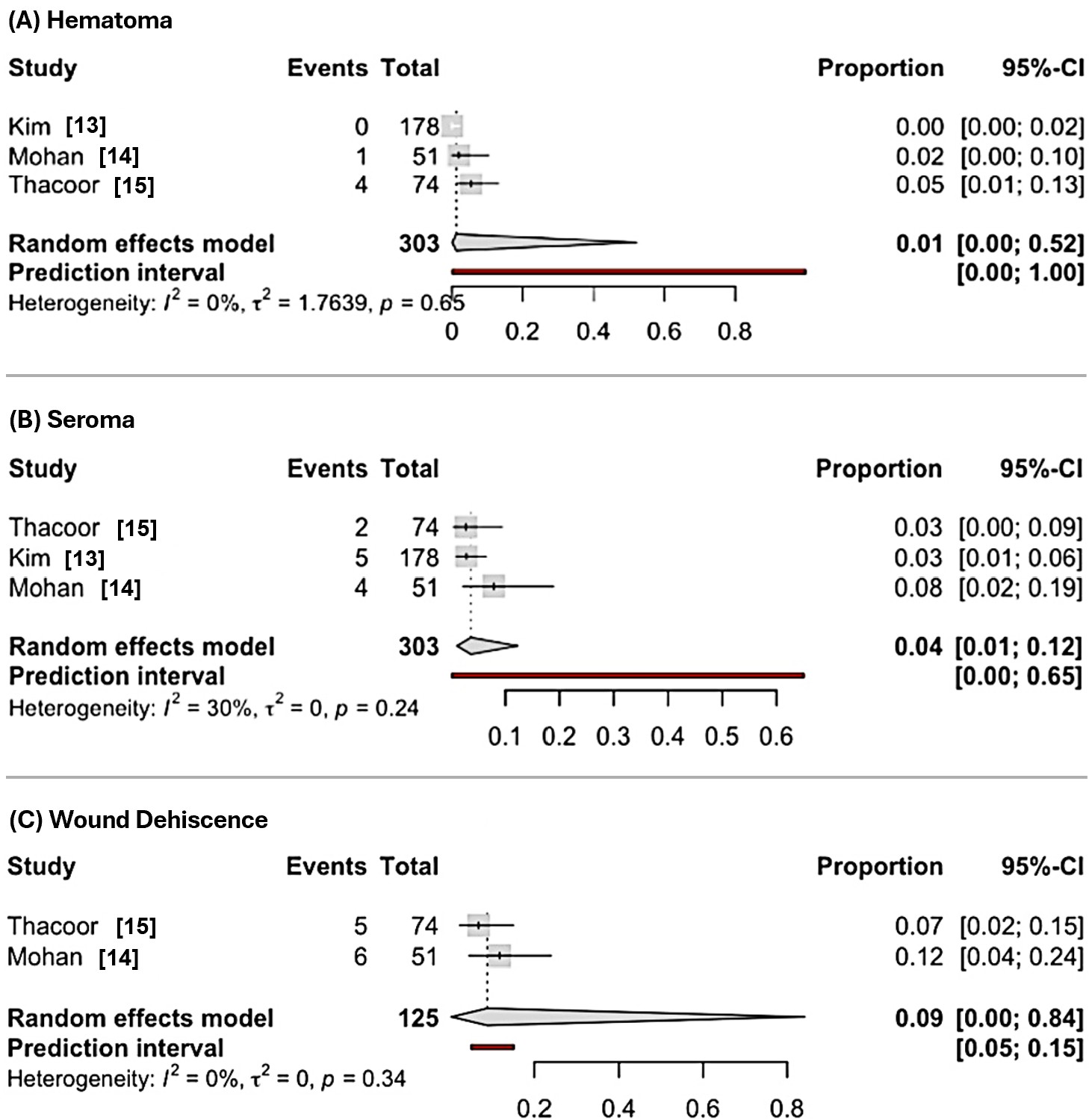
Figure 2. Forest plots of pooled incidence rates of postoperative complications following DIEP flap reconstruction. (A) Pooled incidence of hematoma shows a proportion of 0.01 (95% CI: 0.00–0.52) using a random effects model, based on 303 subjects across three studies, with no heterogeneity (I² = 0%, p = 0.65). A random effects model is chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05). (B) Pooled incidence of seroma shows a proportion of 0.04 (95% CI: 0.01–0.12) using a random effects model, based on 303 subjects across three studies, with moderate heterogeneity (I² = 30%, p = 0.24). A random effects model is selected to account for the observed heterogeneity, despite the lack of statistical significance (p > 0.05). (C) Pooled incidence of wound dehiscence shows a proportion of 0.09 (95% CI: 0.00–0.84) using a random effects model, based on 125 subjects across two studies, with no heterogeneity (I² = 0%, p = 0.34). A random effects model is chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05). Abbreviations: DIEP, deep inferior epigastric perforator; CI, confidence interval.
Seroma Incidence Analysis
We also analyzed the incidence of seroma in DIEP flap breast reconstruction among the same cohort of 603 participants. The drain-based group, which included data from three studies with 303 subjects (Figure 2B), exhibited a pooled seroma incidence of 0.04 (95% CI: 0.01 to 0.12) using a random effects model, with moderate heterogeneity (I² = 30%, p = 0.24). A random effects model was selected to account for the observed heterogeneity, despite the lack of statistical significance (p > 0.05).
The drainless group, based on four studies with 300 subjects (Figure 3B), displayed a pooled seroma incidence of 0.05 (95% CI: 0.02 to 0.15) using a random effects model, with moderate heterogeneity (I² = 42%, p = 0.16). A random effects model was chosen to account for the observed heterogeneity, despite the lack of statistical significance (p > 0.05).
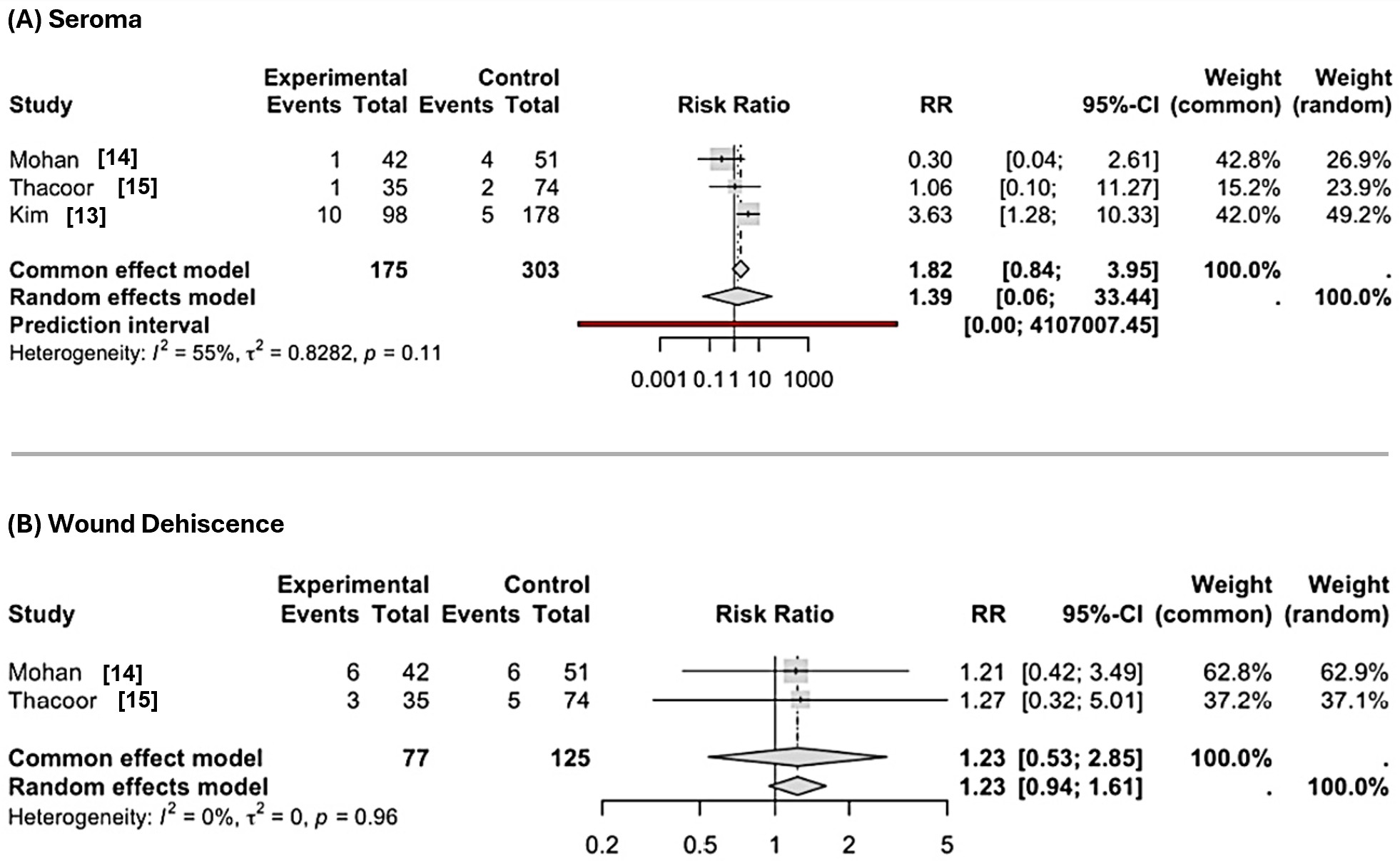
The pooled RR for seroma incidence was calculated to compare the effectiveness of seroma management between the drain-based and drainless DIEP flap reconstruction techniques. As illustrated in Figure 4A, the pooled RR was 1.82 (95% CI: 0.84–3.95) using a common effect model and 1.39 (95% CI: 0.06–33.44) using a random effects model, based on 175 experimental (drainless) and 303 control (drain-based) subjects across three studies, with moderate heterogeneity (I² = 55%, p = 0.11). A random effects model was chosen as the primary analysis due to the presence of moderate heterogeneity, despite the lack of statistical significance (p > 0.05).
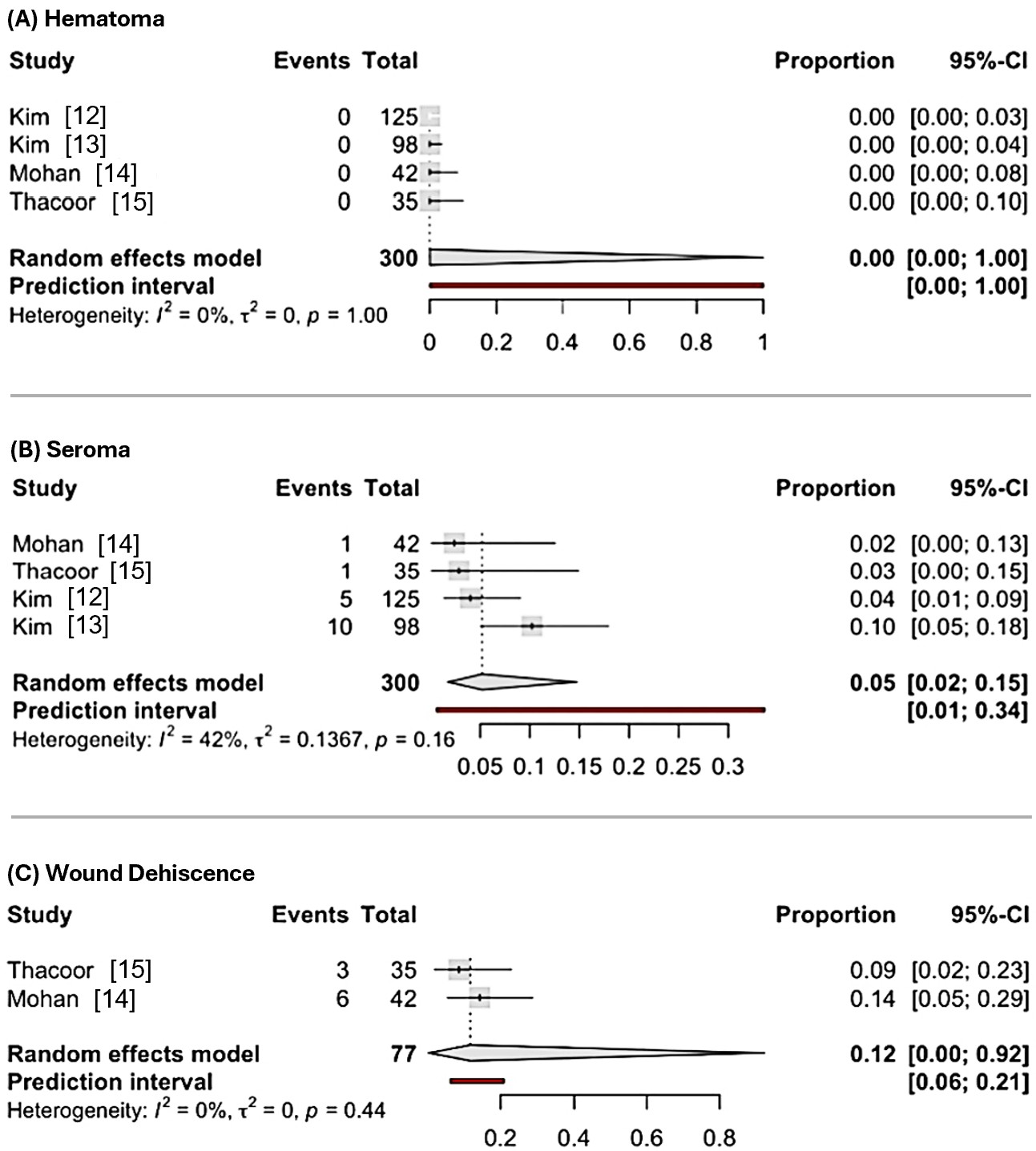
Figure 3. Forest plots of pooled incidence rates of postoperative complications following drainless DIEP flap reconstruction. (A) Pooled incidence of hematoma shows a proportion of 0.00 (95% CI: 0.00–1.00) using a random effects model, based on 300 subjects across four studies, with no heterogeneity (I² = 0%, p = 1.00). A random effects model is chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05). (B) Pooled incidence of seroma shows a proportion of 0.05 (95% CI: 0.02–0.15) using a random effects model, based on 300 subjects across four studies, with moderate heterogeneity (I² = 42%, p = 0.16). A random effects model is selected to account for the observed heterogeneity, despite the lack of statistical significance (p > 0.05). (C) Pooled incidence of wound dehiscence shows a proportion of 0.12 (95% CI: 0.00–0.92) using a random effects model, based on 77 subjects across two studies, with no heterogeneity (I² = 0%, p = 0.44). A random effects model is chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05). Abbreviations: DIEP, deep inferior epigastric perforator; CI, confidence interval.
Wound Dehiscence Incidence Analysis
This meta-analysis assessed the incidence of wound dehiscence in DIEP flap breast reconstruction among 202 participants across four studies. The drain-based group, comprising data from two studies with 125 subjects, exhibited a pooled incidence of wound dehiscence of 0.09 (95% CI: 0.00 to 0.84) using a random effects model, with no heterogeneity (I² = 0%, p = 0.34) (Figure 2C). A random effects model was chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05).
Conversely, the drainless group, involving data from two studies with 77 subjects, reported a pooled incidence of 0.12 (95% CI: 0.00 to 0.92) using a random effects model, also with no heterogeneity (I² = 0%, p = 0.44) (Figure 3C). A random effects model was selected for consistency in analysis, despite the lack of statistical significance in heterogeneity (p > 0.05).
The pooled RR for wound dehiscence was calculated to compare the incidence between drain-based and drainless DIEP flap reconstruction techniques, as depicted in Figure 4B. The pooled RR was 1.23 (95% CI: 0.53–2.85) using a common effect model and 1.23 (95% CI: 0.94–1.61) using a random effects model, based on 77 experimental (drainless) and 125 control (drain-based) subjects across two studies, with no heterogeneity (I² = 0%, p = 0.96). A random effects model was chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05).
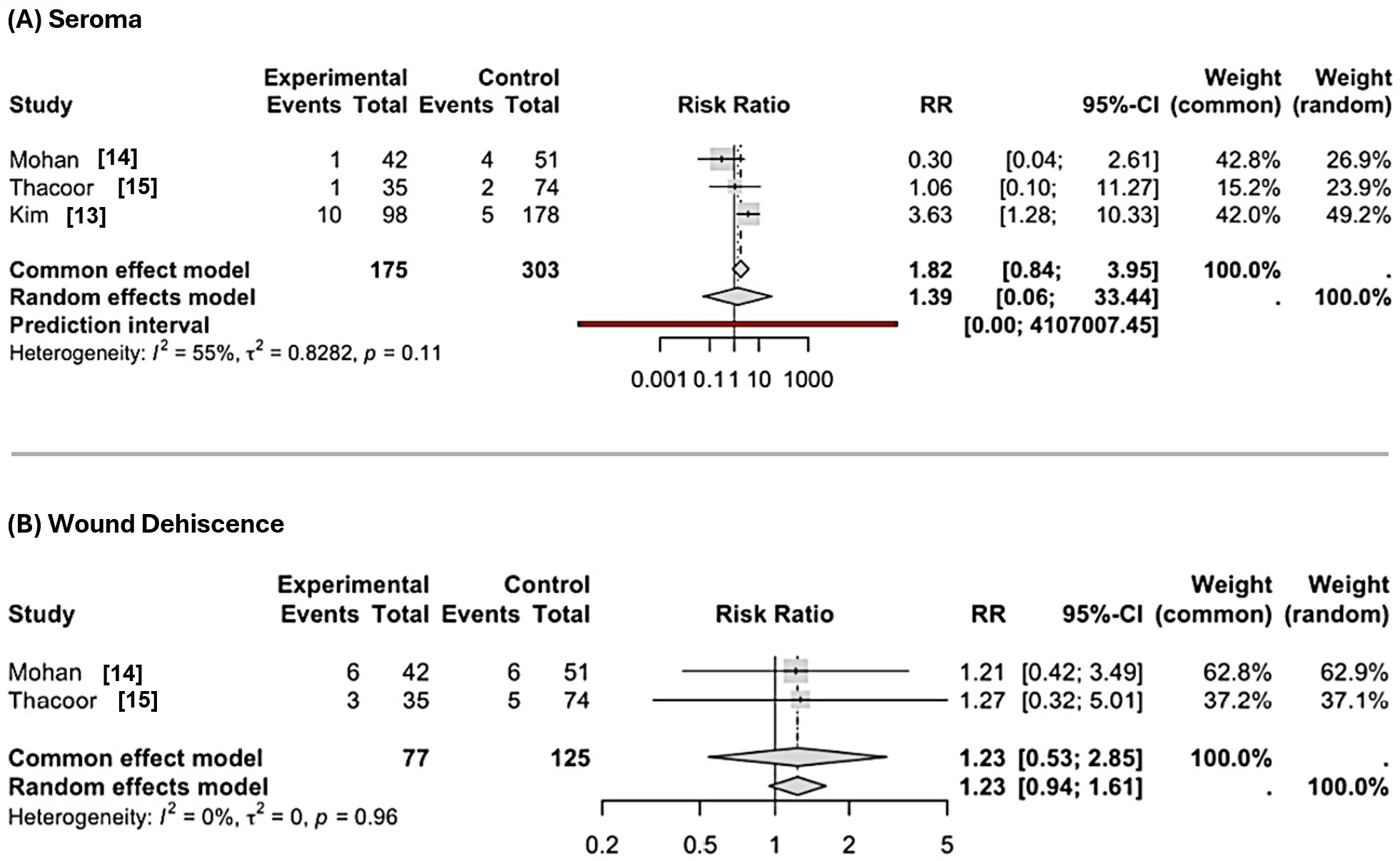
Figure 4. Forest plots of pooled risk ratios for postoperative complications following drainless versus drained DIEP flap reconstruction. (A) Pooled risk of seroma presents an RR of 1.82 (95% CI: 0.84–3.95) using a common effect model and 1.39 (95% CI: 0.06–33.44) using a random effects model, based on 175 experimental and 303 control subjects across three studies, with moderate heterogeneity (I² = 55%, p = 0.11). A random effects model is chosen as the primary analysis due to the presence of moderate heterogeneity, despite the lack of statistical significance (p > 0.05). (B) Pooled risk of wound dehiscence shows an RR of 1.23 (95% CI: 0.53–2.85) using a common effect model and 1.23 (95% CI: 0.94–1.61) using a random effects model, based on 77 experimental and 125 control subjects across two studies, with no heterogeneity (I² = 0%, p = 0.96). A random effects model is chosen as the primary analysis to account for potential heterogeneity, despite the absence of statistical significance (p > 0.05). Abbreviations: DIEP, deep inferior epigastric perforator; CI, confidence interval; RR, risk ratio.
Infection Incidence Analysis
Among the studies reviewed, only Mohan et al. reported infection rates, documenting four cases (7.8%) in the drain-based group among 51 patients and two cases (4.8%) in the drainless group among 42 patients [14]. The absence of infection data from other studies precluded a pooled incidence or risk ratio analysis, thereby preventing any statistically meaningful comparison between the two techniques regarding infection risk.
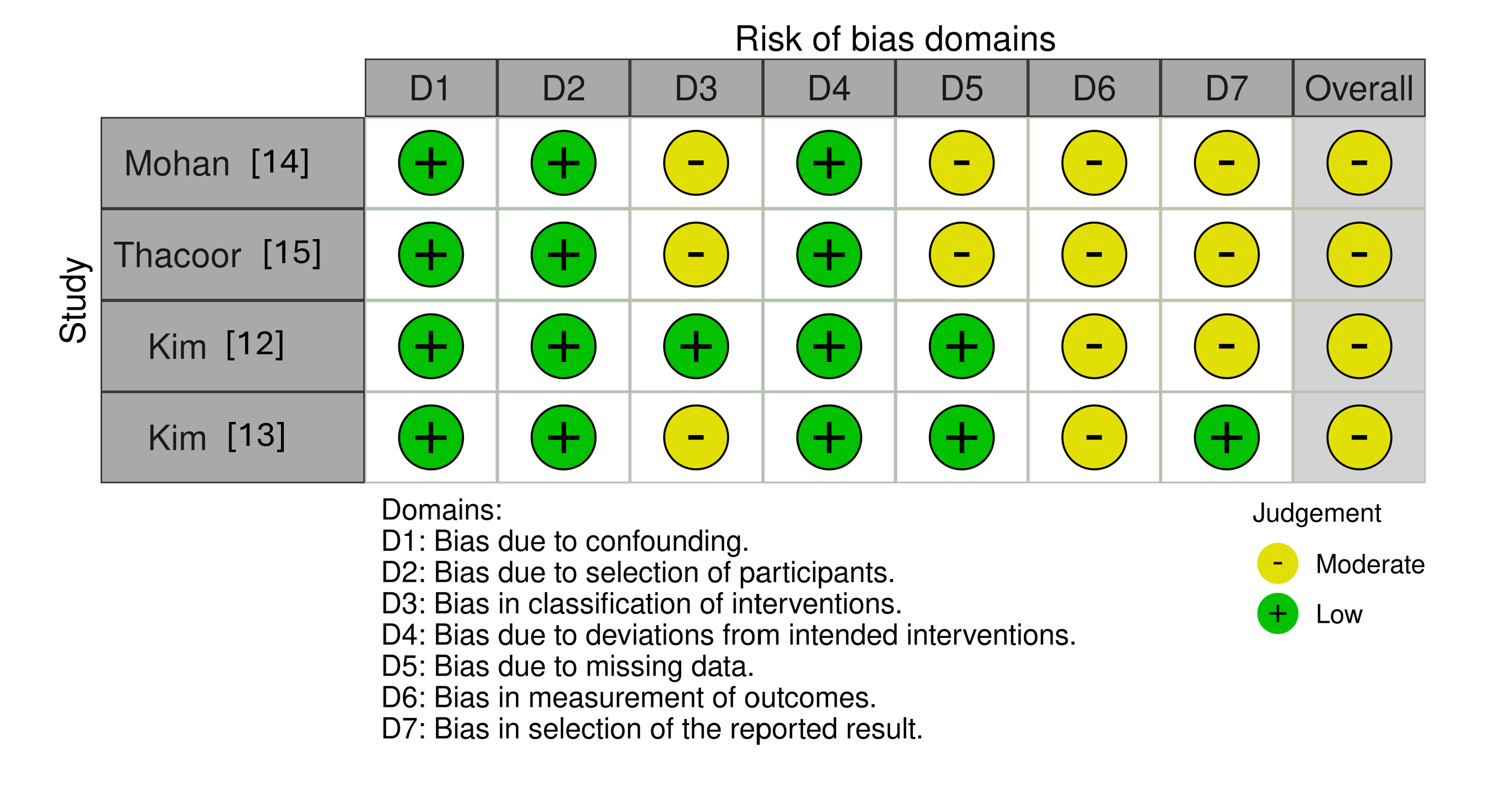
Figure 5. Traffic light plot of observational studies using the ROBINS-I tool for risk of bias assessment in postoperative complications following drainless DIEP flap reconstruction. This traffic light plot evaluates bias across seven domains: confounding, selection of participants, classification of interventions, deviations from intended interventions, missing data, measurement of the outcome, and selection of the reported result. Green circles represent a low risk of bias, while yellow circles indicate a moderate risk of bias. The overall risk of bias is classified as moderate, characterized by low risk in the domains of confounding, selection of participants, and deviations from intended interventions. Moderate risk is observed in the domains of classification of interventions, missing data, measurement of the outcome, and selection of the reported result. Abbreviation: DIEP, deep inferior epigastric perforator; ROBINS-I, Risk of bias in non-randomized studies of interventions tool.
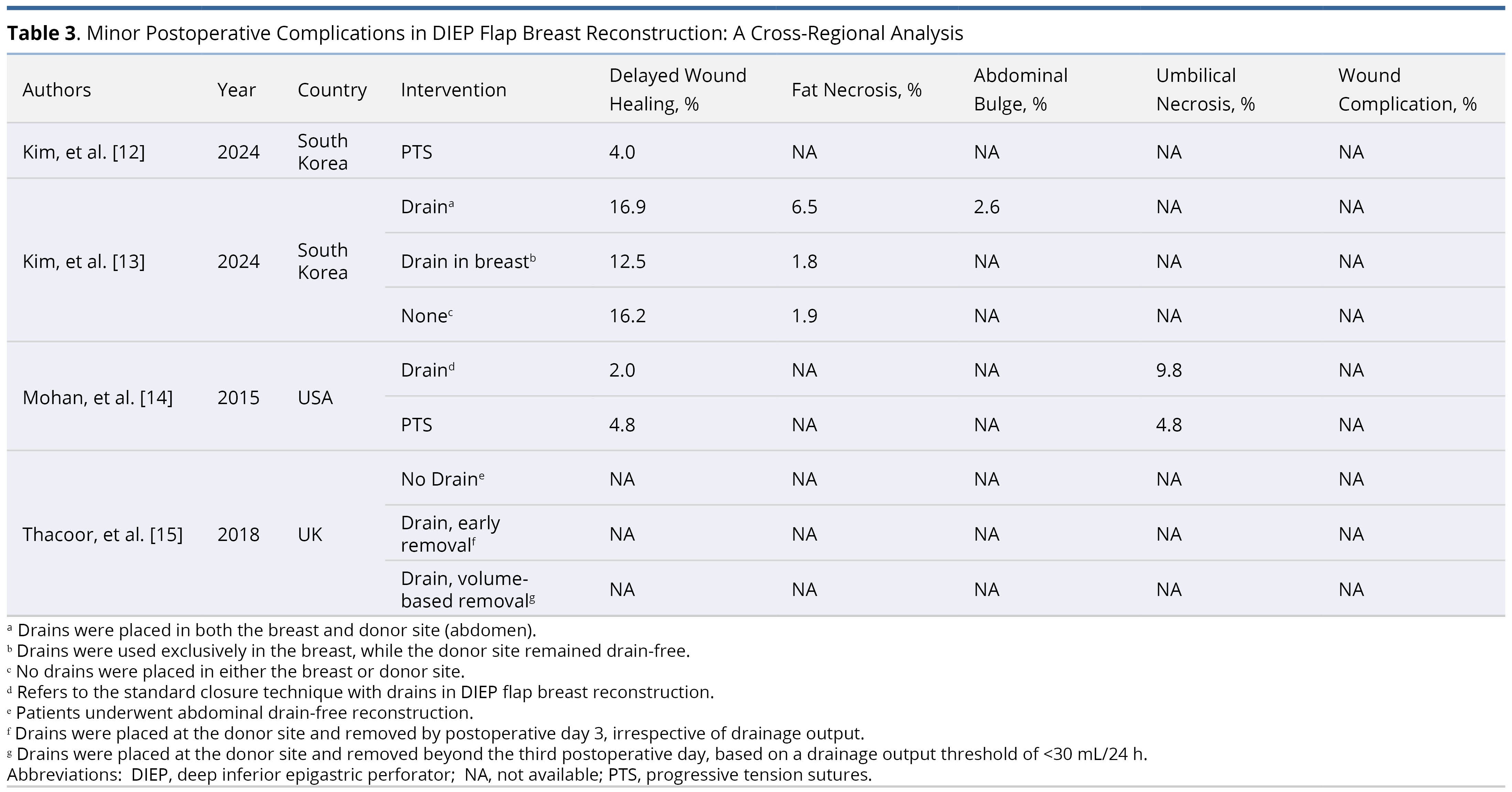
Risk of Bias Assessment
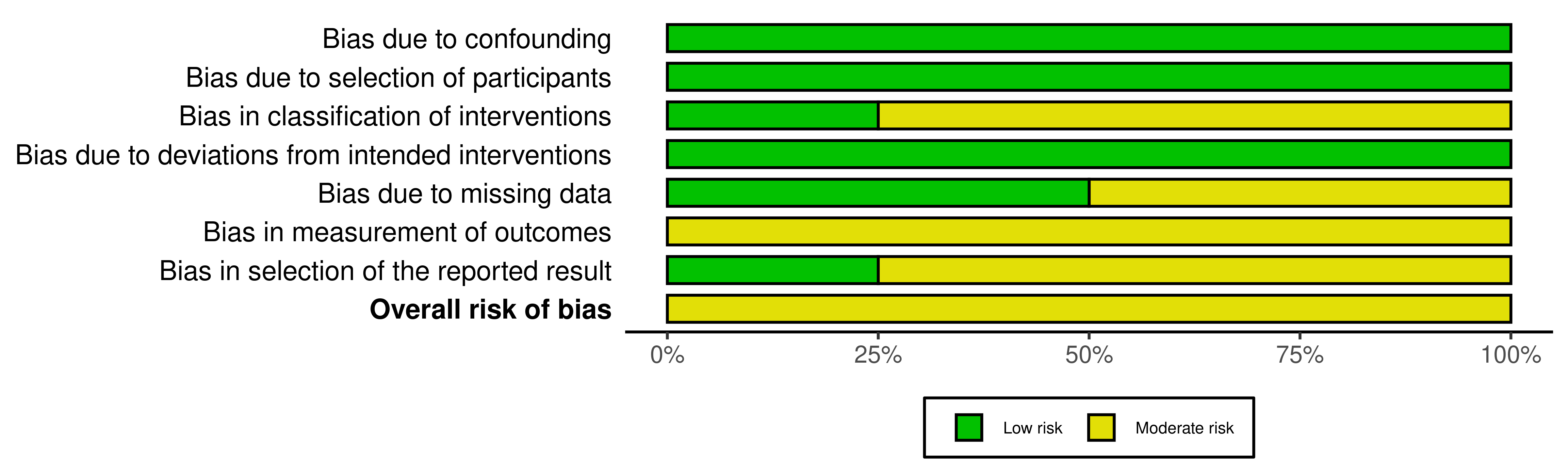
We assessed all four included studies, which were observational in nature, using the ROBINS-I tool. The evaluation of the risk of bias is summarized in Figure 5 (risk of bias traffic plot) and Figure 6 (risk of bias summary plot).
As indicated in Figure 5, the most common sources of bias occurred in the domains of intervention classification, outcome measurement, and selection of reported results, each rated as moderate risk in three of the four studies. The domain concerning bias due to missing data exhibited moderate risk in two studies. In contrast, the risks due to confounding, selection of participants, and deviations from intended interventions were consistently judged as low across all studies, demonstrating adequate methodological rigor in study design and adherence to intended protocols.
Figure 6 provides a consolidated summary of the proportion of studies rated at each risk level across all domains. The highest concentration of moderate risk was observed in domains related to intervention classification, outcome measurement, and selective reporting. No domain was rated as having critical risk, and the overall bias profile supports the inclusion of these studies in the meta-analytic synthesis, albeit with caution due to inherent design limitations.
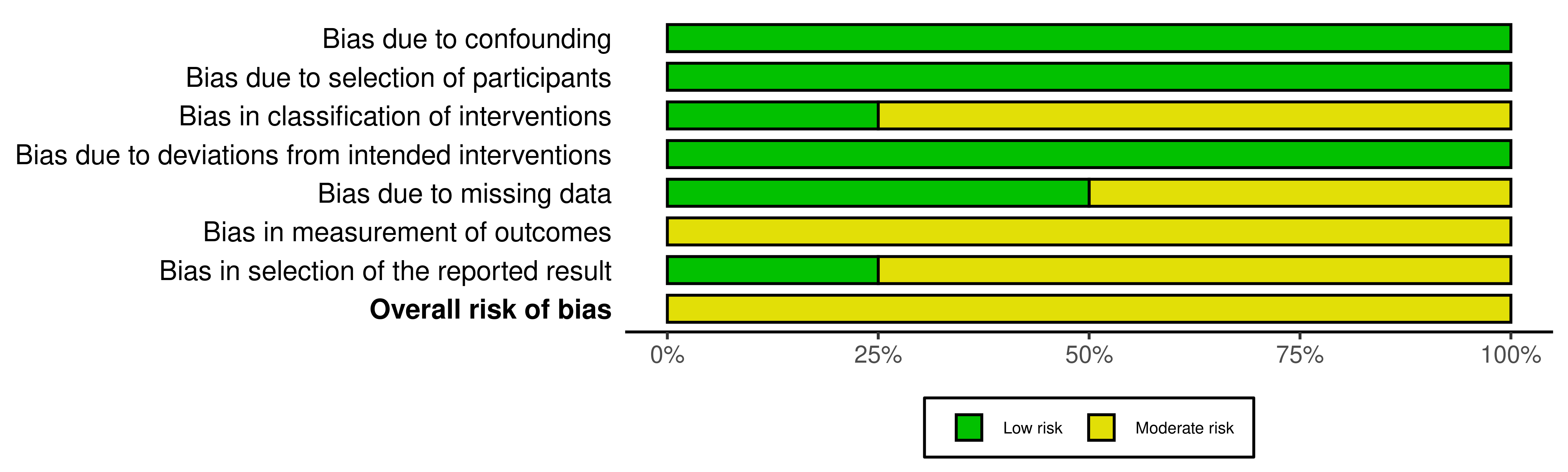
Figure 6. Summary plot of observational studies using the ROBINS-I tool for risk of bias assessment in postoperative complications following drainless diep flap reconstruction. This summary plot evaluates bias across seven domains and overall risk for four studies: bias due to confounding, bias due to selection of participants, bias in classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in measurement of the outcome, bias in selection of the reported result, and overall risk of bias. Green bars represent a low risk of bias, while yellow bars indicate a moderate risk of bias; no high risk is observed. Low risk is predominant in confounding (100%), selection of participants (100%), and deviations from intended interventions (100%). A balanced distribution is observed in missing data (50% low, 50% moderate). Moderate risk is predominant in classification of interventions (25% low, 75% moderate) and selection of the reported result (25% low, 75% moderate). Measurement of the outcome shows 100% moderate risk. The overall risk of bias is 100% moderate. Abbreviation: DIEP, deep inferior epigastric perforator; ROBINS-I, Risk of bias in non-randomized studies of interventions tool.
Key Findings
In this systematic review and meta-analysis, we aimed to compare postoperative complications between drainless and drain-based DIEP flap breast reconstruction, thereby addressing a significant gap in evidence concerning optimal donor-site management. Drawing on data from four studies involving 603 patients, we found no statistically significant differences in the incidence of hematoma, seroma, or wound dehiscence between the two techniques. However, the limited data available on infection prevented a comprehensive pooled analysis, constraining our conclusions regarding this specific variable.
Our findings align with the preliminary outcomes reported in Wong and Chansiriwongs’ conference abstract [9], which suggested comparable outcomes across 580 patients. However, this abstract lacked the detailed data necessary for a comprehensive meta-analysis. Without access to a complete dataset, the abstract fell short in offering the transparency required for rigorous scientific evaluation. Our study, employing rigorous meta-analytic methods focused exclusively on DIEP flaps, represents the first comprehensive meta-analysis in this domain. This significant contribution enhances our understanding of postoperative outcomes and substantiates the comparability of drainless and drain-based techniques. The absence of significant differences between the two techniques underscores the need for further investigation into the factors influencing complication rates and the role of drainage in postoperative recovery.
Hematoma Risk Equivalence
Hematoma arises from vascular disruption, which leads to blood leakage into surrounding tissues [16]. An inflammatory response may intensify hematoma formation through vasodilation and increased vascular permeability. One study pinpointed inadequate hemostasis as a key factor in hematoma development, underscoring the critical role of meticulous surgical techniques in mitigating this complication [16]. The use of PTS, a common practice in drainless techniques, enhances hemostasis by uniformly distributing tension and reducing dead space, thereby diminishing the bleeding risk.
Our meta-analysis of four studies on drainless DIEP flap reconstruction found no hematoma events, thereby precluding risk ratio calculations. The absence of hematoma cases suggests an exceedingly low risk associated with drainless procedures, although the lack of comparative data curtails definitive statistical comparisons between techniques. However, the consistent absence of hematoma across the studies may reflect the efficacy of precise closure methods such as PTS.
Collectively, the evidence suggests that both drain-based and drainless techniques are associated with a low risk of hematoma. Despite the constraints on statistical interpretation due to the absence of events, the uniformity of the findings offers reassurance to surgeons opting for drainless closure methods, particularly when they implement rigorous hemostasis techniques like PTS.
Comparable Seroma Outcomes
The drainless approach in DIEP flap breast reconstruction obviates the need for postoperative drain management, thus reducing follow-up requirements and alleviating logistical and financial burdens on patients [17]. This method is particularly beneficial for outpatient recovery, as it circumvents the complications associated with delayed drain removal and the need for frequent output monitoring.
Previous research has demonstrated complication rates comparable to those observed in conventional drain-based reconstruction. Specifically, studies comparing drainless techniques employing PTS to traditional drain-based methods have not identified significant differences in postoperative outcomes. For instance, Jackson et al. reported similar rates of seroma, hematoma, infection, and wound dehiscence between the two groups [17].
Seroma formation often results from persistent dead space within disrupted tissue [18]. It has proved to be effectively addressed by the drainless technique through the application of PTS. This method eliminates dead space, distributes tension evenly, and improves tissue approximation. It enhances hemostasis, reduces lymphatic leakage, and promotes efficient healing, thus potentially reducing fluid accumulation.
Despite these mechanistic advantages, robust evidence confirming the benefits of the drainless approach remains elusive. To bridge this evidence gap, we conducted a meta-analysis to compare seroma incidence between drain-based and drainless techniques. The pooled data showed no statistically significant difference in seroma risk. However, substantial heterogeneity and wide CIs were evident, likely reflecting variations in surgical methods, outcome definitions, and sample sizes. This variability, together with the imprecision of current data, precludes definitive conclusions regarding the superiority of either approach in preventing seroma.
Nevertheless, the drainless technique remains an attractive option in selected settings, particularly when minimizing postoperative management and improving patient comfort are priorities. In clinical practice, the choice of reconstruction should balance complication risk with patient-specific factors, including comorbidities, recovery environment, and individual preference.
Wound Dehiscence Equivalence
Our pooled analysis revealed a slightly higher incidence of wound dehiscence in the drainless group, although these differences between the techniques were not statistically significant. The consistency of findings across studies with minimal heterogeneity suggests a stable overall trend. These results align with the findings from a conference abstract by Wong and Chansiriwongs [9]. Unlike this abstract, which surveyed a broad range of drain-less techniques and outcomes, including postoperative pain and length of stay, our study delivers a more focused and methodologically rigorous analysis. The limitations of the previous review in methodological transparency and its lack of detailed outcome data due to its format are in stark contrast to our meta-analysis, which delivers a comprehensive evaluation of wound-related complications using standardized definitions and thorough bias assessments.
From a mechanistic standpoint, excessive pressure from retained drains may hinder local perfusion and delay tissue healing. Moreover, if not properly managed, drains can become potential sources of infection, exacerbating inflammation and compromising wound integrity [19]. Conversely, the absence of drainage might lead to fluid accumulation and increased tissue tension, which could also contribute to wound dehiscence. These opposing factors likely explain the slight variations in reported rates, without producing statistically significant differences.
These findings suggest that both drain-based and drainless techniques provide comparable safety profiles concerning wound dehiscence. Clinicians should weigh individual patient risk factors and surgical nuances that may influence healing outcomes. Ultimately, precise intraoperative technique and tailored postoperative care are likely more influential than the choice of drainage strategy alone in minimizing wound-related complications.
Infection Risk Uncertainty
The incidence of infection could not be evaluated through pooled analysis due to inconsistent reporting across the studies reviewed. Among the literature, only Mohan et al. provided relevant data, documenting an infection rate of 7.8% in the drain-based group and 4.8% in the drainless group [14]. The scarce data on infection-related outcomes limits our capacity to assess the relative safety of each surgical approach comprehensively.
From a mechanistic standpoint, infections may arise from surgical site contamination, seroma accumulation, or inadequate debridement. Traditionally, drains are employed to minimize fluid buildup, theoretically reducing the risk of infection; however, they may also introduce bacteria into the wound. In contrast, the drainless approach eliminates this potential entry point but depends on effective wound closure and fluid management to prevent infection. Although previous research suggests that drains may help mitigate infection by reducing seroma accumulation [7], the similar seroma rates observed in our study challenge the definitive assessment of drainage's impact on infection risk.
Minor Complications Overview
While the primary focus of this analysis was on major postoperative complications, minor events such as delayed wound healing, fat necrosis, abdominal bulge, and umbilical necrosis were also reported across several studies. These outcomes were less consistently reported, contributing to the limited overall quality of data. The rates of delayed wound healing varied widely, with fat necrosis infrequently documented. Notably, abdominal bulge and umbilical necrosis occurred more frequently in groups managed with drains. These observations indicate potential differences in minor postoperative outcomes between drainage strategies. However, the limited number of cases and inconsistent reporting constrain definitive interpretation. Comprehensive studies that systematically capture both major and minor complications are essential to fully understand the spectrum of postoperative recovery.
Balancing Drainage Decisions
This meta-analysis found no statistically significant differences in major postoperative complications between drain-based and drainless DIEP flap reconstruction. However, the practical advantages of adopting a drainless approach warrant careful consideration. By eliminating drains, postoperative management is simplified, reducing the need for frequent clinical visits for drain removal and monitoring, which in turn enhances patient comfort. Consequently, this simplification can logically be expected to shorten hospital stays, thereby reducing both the logistical and financial burdens for patients undergoing DIEP flap breast reconstruction.
Several studies corroborate the assertion that eliminating drains could shorten hospital stays. For instance, Thacoor et al. reported comparable complication rates and lengths of hospital stay between drain-based and drainless DIEP reconstruction [15]. Similarly, Chan et al. observed that patients undergoing drainless abdominal flap breast reconstruction (including both DIEP and TRAM flaps) using PTS experienced significantly lower postoperative complication rates and shorter hospital stays compared to conventional drain-based methods [20]. Moreover, Jackson et al. demonstrated that omitting drains after mastectomy significantly reduced both length of stay and overall healthcare costs without increasing complication rates or subsequent interventions for seroma [17]. Additionally, Khan et al. conducted a meta-analysis involving multiple abdominal flap types, including both DIEP and TRAM flaps [10]. The surgeries employed PTS to facilitate the drainless closures. They found that drainless closure significantly reduced hospital stays by an average of 1.15 days and lowered the overall complication rate [10]. This reduction in hospital time was associated with decreased postoperative resource utilization.
Collectively, these findings suggest that, in selected clinical scenarios, the drainless approach represents a viable option without compromising safety, potentially providing meaningful improvements in patient-centered outcomes and cost-effectiveness. Clinicians should carefully weigh the relative benefits and limitations of each method, tailoring the choice of reconstruction technique according to individual patient characteristics, medical comorbidities, available recovery resources, and personal values regarding postoperative comfort and convenience.
Risk of Bias Considerations
The overall risk of bias across the included studies was assessed as moderate, with no domain reaching a critical level. This moderate risk profile supports the inclusion of these studies in our meta-analysis, though caution is required when interpreting the findings due to inherent limitations associated with retrospective observational designs.
As depicted in Figure 5, the risk of bias judgments varied across domains and studies. This variation highlights methodological inconsistencies, particularly in areas such as intervention classification, outcome measurement, and the selection of reported results. Figure 6 reinforces these findings, summarizing the overall distribution of risk levels across domains and showing a concentration of moderate risk in these specific areas.
In contrast, areas such as confounding, participant selection, and adherence to planned interventions consistently showed low risk of bias, reflecting robust methodological control in these aspects. Despite this, the absence of randomization and limited adjustment for baseline characteristics are significant limitations that could influence effect estimates.
For future research, it is essential to prioritize prospective studies with pre-registered protocols and standardized definitions. Rigorous adjustment for confounding factors is necessary. Furthermore, transparent handling of missing data and complete outcome reporting are crucial for minimizing bias and enhancing the reliability of comparative surgical research.
Study Limitations
This study encounters several limitations that warrant consideration when interpreting its findings. Firstly, the limited number of studies and their relatively small sample sizes may have reduced the statistical power needed to detect significant differences between drainless and drain-based DIEP flap reconstruction. This limitation could also affect the ability to assess heterogeneity accurately, potentially leading to an underestimation of the true variability across studies.
Secondly, the heterogeneity observed in the included studies regarding study design, patient selection, and surgical techniques could have influenced the reported complication rates. Variations in postoperative management, adjunctive measures, and methods for assessing complications likely contributed to differences in findings. Moderate heterogeneity noted for some outcomes, such as seroma, may impact the stability of the meta-analysis estimates and warrants cautious interpretation.
Thirdly, the precision of some meta-analysis estimates was limited by wide CIs, reflecting significant uncertainty in the results. This uncertainty, combined with the observed heterogeneity, suggests that the findings might not be fully generalizable and should be interpreted with caution. Additionally, the prediction intervals for certain outcomes indicate that future studies could yield results with considerable variability, further emphasizing the need for careful consideration.
Assessment variability also represents an additional source of limitation. Differences in operator skill levels and the sensitivity of evaluation methods may influence complication detection and reporting. Some studies incorporated diagnostic tools such as ultrasound to enhance accuracy and reduce examiner-dependent error [21]. However, ultrasound interpretation is operator-dependent and may introduce interobserver variability, potentially affecting the consistency and validity of reported outcomes. Despite using strict inclusion and exclusion criteria, methodological differences across studies remain a challenge to comparability.
Moreover, all included studies were retrospective in design, which introduces a higher risk of selection bias and confounding. Drainage protocols were not standardized, varying from no drainage to early removal or volume-based thresholds, which may have influenced postoperative outcomes. Complication rates were often reported without measures of variability or formal statistical comparisons, limiting the interpretability and generalizability of the results.
Lastly, the absence of economic evaluations in the included studies prevents an assessment of the cost-effectiveness of drainless DIEP flap reconstruction. While this approach may theoretically reduce follow-up visits and hospitalization, the lack of direct cost comparisons limits the ability to evaluate its financial impact.
Future research should prioritize well-designed, large-scale randomized controlled trials employing standardized surgical protocols, consistent outcome definitions, and long-term follow-up. Incorporating cost-effectiveness analyses is also essential to comprehensively evaluate the clinical and economic value of drainless DIEP flap reconstruction.
The study is the first to examine postoperative outcomes between drainless and drain-based DIEP flap reconstructions exclusively. No statistically significant differences were observed in seroma, hematoma, or wound dehiscence rates. Analysis of infection rates was not possible due to insufficient data. Although it remains unclear if drainless techniques are superior, the results indicate comparable outcomes to traditional drain-based methods, suggesting drainless approaches are viable and safe, potentially improving patient-centered outcomes and cost-effectiveness. Clinicians should tailor their choice of technique to individual patient needs and preferences. Future research should focus on long-term complications and cost-effectiveness, incorporating patient-reported outcomes to support evidence-based surgical decisions.
Received date: November 30, 2024
Accepted date: March 04, 2025
Published date: April 21, 2025
The authors confirm that this systematic review has been registered in PROSPERO (CRD42024588015). The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the research topic.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2025The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Controversies have recently arisen regarding post-operative haemorrhagic complications in relation to the surgical procedures adopted for tonsillectomy. The authors set out to verify the relationship between surgical techniques and post-operative haemorrhage based on the analysis of data derived from multi-centric studies.
This study examined two surgical techniques commonly used for turbinate reduction (i.e., submucous resection and partial excision) and their associated complications in functional nasal surgery patients. So far, there has been no direct comparison of these two methods with endpoints of epistaxis and nasal congestion. It was found neither technique was statistically significantly different from the other, so both are clinically useful with a low incidence of postoperative epistaxis.
This article presents a crucial case report on potential wound healing complications linked to fremanezumab, a calcitonin gene-related peptide-targeting antibody for migraine prevention. It documents the first known instance of delayed wound healing following a free flap breast reconstruction, underscoring the need for heightened clinical vigilance and individualized patient assessment in perioperative settings. Highlighting significant safety data gaps, the report advocates for comprehensive research and rigorous post-marketing surveillance. The findings emphasize the importance of balancing the risks of delayed wound healing with the need for effective disease control, especially when using biologic agents for chronic conditions. This article is essential for medical professionals managing patients on biologic therapies, offering critical insights and advocating for a personalized approach to optimize patient outcomes. By presenting novel observations and calling for further investigation, it serves as a vital resource for enhancing patient care and safety standards in the context of biologic treatments and surgical interventions.
A 33-year-old woman presented with acute right-sided facial swelling, dysphonia, and dysphagia, and further examination revealed a raised floor of the mouth with fluctuation and induration. Panoramic imaging suggested an odontogenic abscess associated with a previously treated tooth that had failed root canal treatment. However, imaging after emergency department referral revealed radio-opacities along the right submandibular duct's course, indicating sialolithiasis as the likely cause. This case emphasizes the importance of considering anatomic structures when establishing a differential diagnosis and highlights the potential for sialolithiasis to mimic the presentation of an odontogenic abscess. Rapid identification and proper management of these conditions are crucial, given the potential risk they pose to the airway and other structures.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
This article presents a crucial case report on potential wound healing complications linked to fremanezumab, a calcitonin gene-related peptide-targeting antibody for migraine prevention. It documents the first known instance of delayed wound healing following a free flap breast reconstruction, underscoring the need for heightened clinical vigilance and individualized patient assessment in perioperative settings. Highlighting significant safety data gaps, the report advocates for comprehensive research and rigorous post-marketing surveillance. The findings emphasize the importance of balancing the risks of delayed wound healing with the need for effective disease control, especially when using biologic agents for chronic conditions. This article is essential for medical professionals managing patients on biologic therapies, offering critical insights and advocating for a personalized approach to optimize patient outcomes. By presenting novel observations and calling for further investigation, it serves as a vital resource for enhancing patient care and safety standards in the context of biologic treatments and surgical interventions.
This article examines the comparative outcomes of drain versus drainless DIEP flaps in breast reconstruction, utilizing systematic review methodologies combined with meta-analysis to provide a detailed exploration of postoperative complications like seroma and wound dehiscence. By synthesizing existing data, the authors highlight the potential benefits of drainless techniques in reducing complications, offering a patient-centered approach to surgical innovation. The study’s emphasis on minimally invasive methods aligns with the broader goal of improving patient outcomes and optimizing clinical practices. However, significant concerns presently affect the article, rendering it unsuitable for publication without essential revisions. Some revisions addressing the issues below could enhance the article's suitability for publication.
This article systematically reviews and analyzes the outcomes of drainless DIEP flaps in breast reconstruction, highlighting their potential to minimize complications while maintaining clinical effectiveness. Building on established surgical methods, the study explores key factors such as seroma formation and wound dehiscence, providing insights into optimizing postoperative care. By synthesizing data through a meta-analysis, it underscores the importance of tailoring techniques to enhance patient outcomes. However, inconsistencies in data interpretation and unsupported conclusions weaken its impact. Addressing these issues would elevate the study’s contribution to evidence-based practice and advance the field of reconstructive surgery.
This article addresses a critical aspect of breast reconstruction by comparing outcomes between drain and drainless DIEP flaps, offering valuable insights into optimizing surgical techniques to minimize complications. Through a detailed analysis of multiple studies, the authors provide evidence of comparable efficacy between the two methods in terms of seroma and wound dehiscence, while emphasizing the potential benefits of drainless interventions in enhancing patient comfort and reducing procedural risks. The article’s originality lies in its balanced focus on clinical outcomes and practical implications, offering indispensable guidance for reconstructive surgeons and healthcare policymakers. This work demonstrates robust methodology and significant clinical relevance, meriting publication upon addressing specific enhancements, such as including a reference to PRISMA guidelines to strengthen methodological rigor, clarifying ambiguous statements in the statistical analysis section, and justifying the exclusion criteria for studies with fewer than five participants to enhance transparency and the validity of selection criteria.
Christian S, Suteja RC, Purnama GV, Tokan RK, Kenjiro E, Chen J, Salim A, Samsarga GW. Drainless versus drain-based DIEP flap breast reconstruction: A systematic review and meta-analysis of postoperative complications. Int Microsurg J 2025;9(1):1. https://doi.org/10.24983/scitemed.imj.2025.00195