Managing vessel size discrepancies during microvascular anastomosis presents significant challenges, especially when the size disparity exceeds a 1:4 ratio. It is crucial to employ effective and reliable techniques to prevent thrombosis caused by vessel distortion, intimal lacerations, and abrupt changes in turbulence. This study introduces the partial lumen-obliteration with sutures followed by end-to-end anastomosis (PLOSEA) technique, which addresses these challenges by partially obliterating the lumen of the larger diameter vessel before performing an end-to-end anastomosis. A critical aspect of this technique is the implementation of a horizontal mattress corner stitch, which is key to ensuring successful outcomes. Accompanied by a detailed video demonstration, this article aims to elucidate the PLOSEA method and provide insights into its application for managing vessel size discrepancies greater than 1:4.
Video 1. Demonstration of the PLOSEA technique in major vessel size mismatch for venous anastomosis. PLOSEA, partial lumen-obliteration with sutures followed by end-to-end anastomosis.
Addressing size discrepancies during microvascular anastomosis is a formidable challenge, especially when discrepancies exceed a 1:4 ratio. Traditional techniques require complex suturing and precise alignment, demanding high levels of surgical skill [1–4]. These practices elevate risks such as thrombosis and intimal damage, which stem from misalignment and turbulent flow. These complexities may extend operative times and increase the risk of complications, potentially deterring less experienced surgeons.
This article introduces the partial lumen-obliteration with sutures followed by end-to-end anastomosis (PLOSEA) technique, specifically designed to manage size discrepancies greater than 1:4. This technique involves partially obliterating the lumen of larger diameter vessels and performing end-to-end anastomosis. A key feature of this approach is the horizontal mattress corner stitch, critical for ensuring successful outcomes, as detailed in the accompanying instructional video.
The PLOSEA technique simplifies the anastomosis process, reducing complexity and potential complications. This improvement enhances accessibility and safety, particularly for surgeons with limited experience. By effectively managing substantial vessel size discrepancies, this method may become a valuable enhancement to the microvascular surgery toolkit.
The PLOSEA technique was applied in four distinct cases, each involving patients who underwent microvascular reconstruction following head and neck oncologic surgeries. Typically, the internal jugular vein or its tributaries were selected as the preferred recipient veins for these procedures. This strategic choice was made to avoid vein grafts in head and neck reconstructions and to align with best practices in surgical efficiency and patient safety.
In situations with substantial size mismatches, specifically when the discrepancy exceeded a 1:4 ratio and the donor vein was long enough to reach the internal jugular vein, an end-to-side anastomosis was typically performed. However, in all reported instances, the skin perforator of the anterolateral thigh flap originated from the oblique branch of the lateral circumflex femoral artery. This branch was notably shorter and narrower, necessitating an end-to-end anastomosis with a tributary of the internal jugular vein.
A 55-year-old male required reconstructive surgery following a wide local excision of buccal carcinoma. The patient underwent reconstruction with an anterolateral thigh flap to repair a through-and-through cheek defect. In this reconstruction, the flap was singularly based on a single oblique perforator. The procedure presented specific challenges: the donor vein, approximately 1 mm in diameter, was significantly narrower than the recipient common facial vein, which measured 5 mm in diameter. The pedicle’s short length further complicated the procedure, rendering an end-to-side anastomosis with the internal jugular vein impractical. Moreover, the absence of viable alternative recipient veins restricted the surgical options. In response to these challenges, we employed the PLOSEA technique, which effectively managed the significant vessel size discrepancy and facilitated a successful microvascular reconstruction.
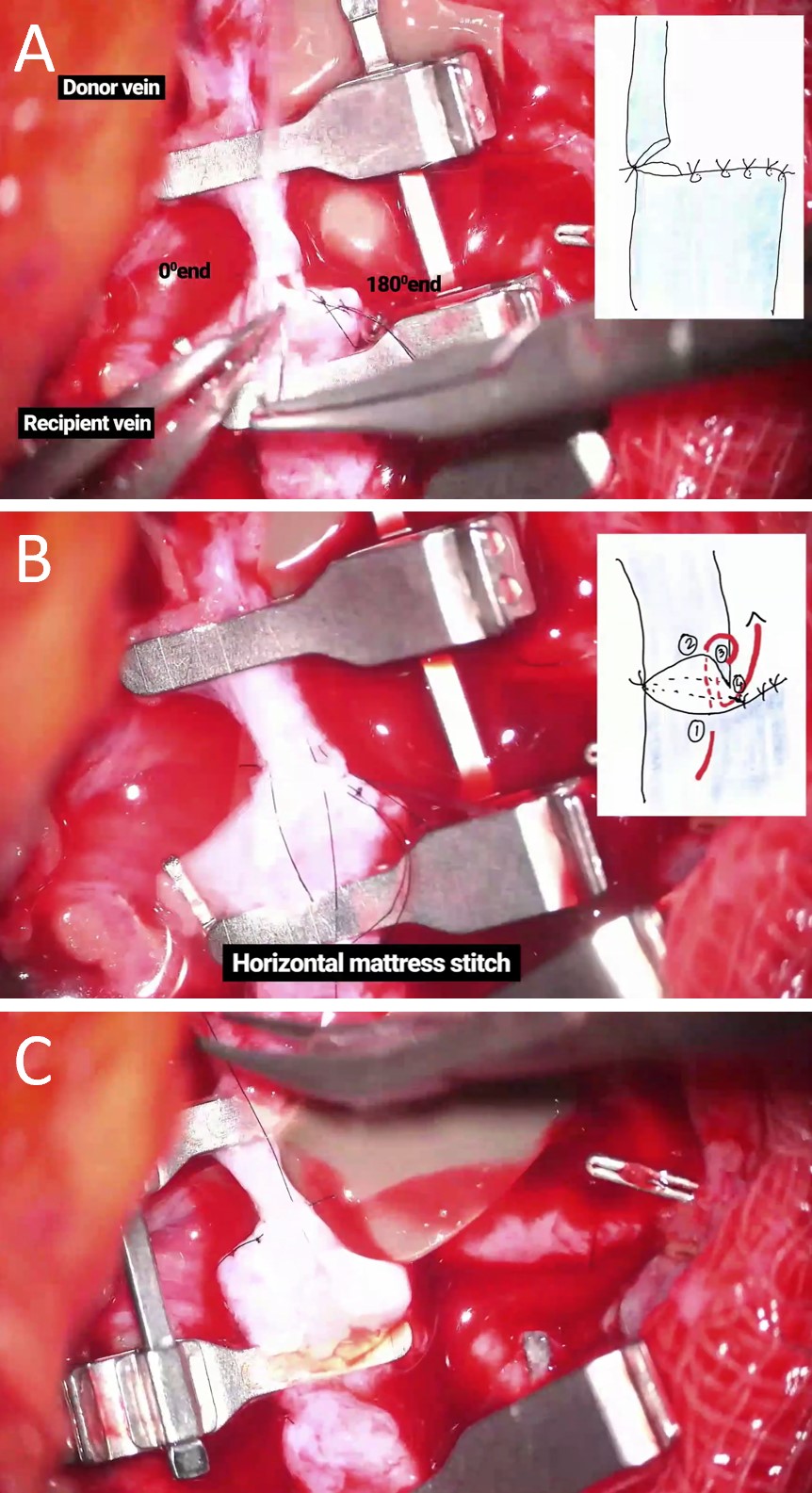
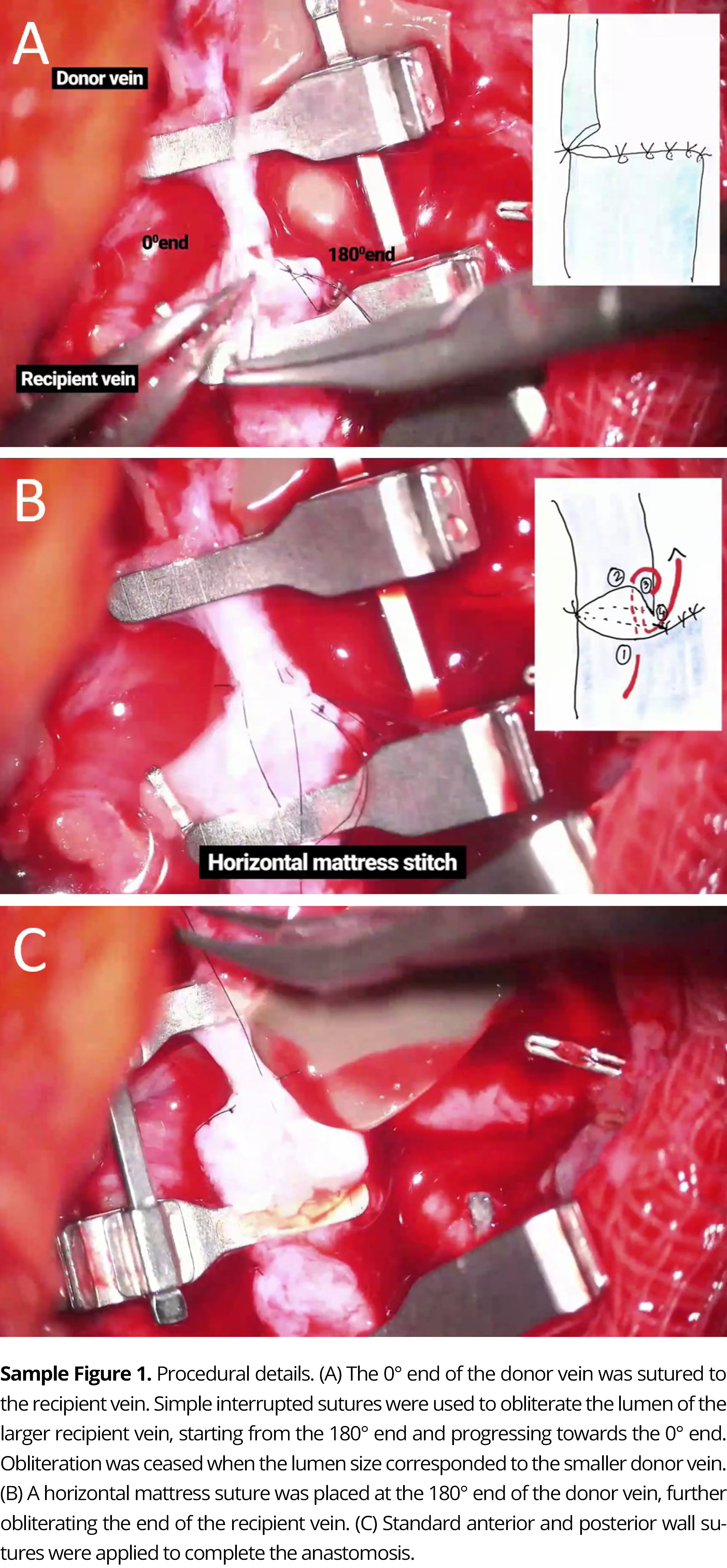
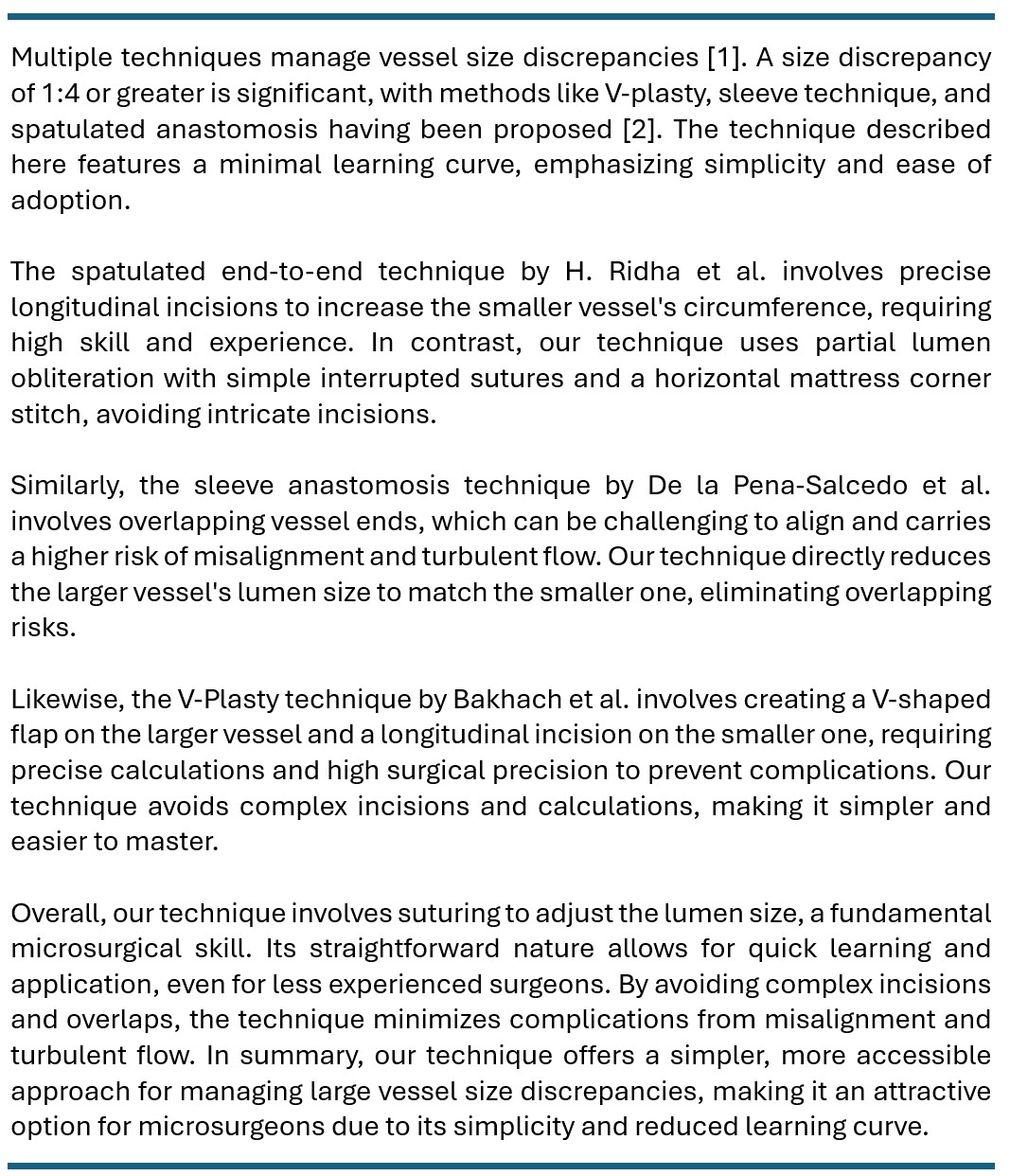
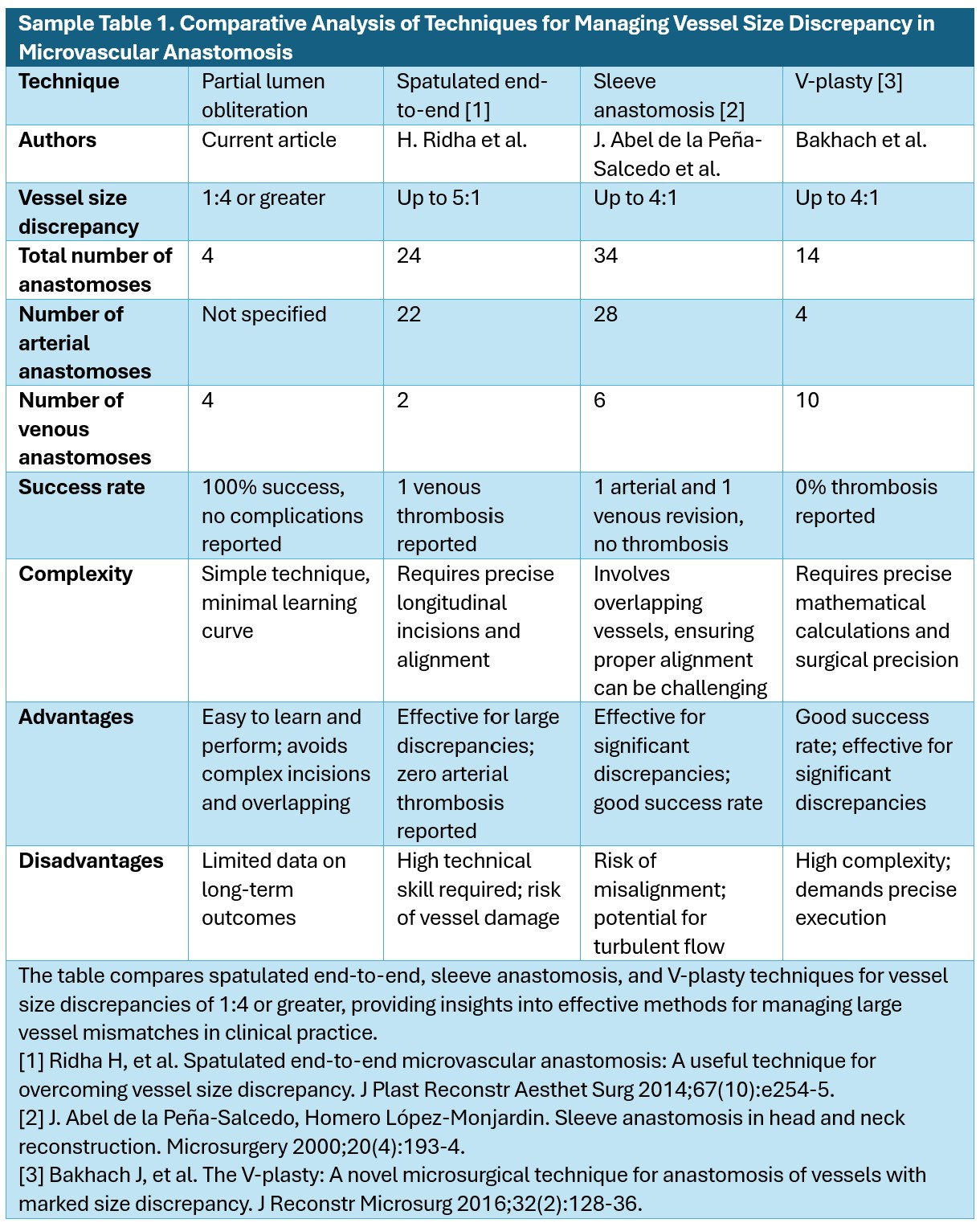
Following the completion of the arterial anastomosis, we initiated the venous anastomosis. This stage commenced with suturing the 0° ends of both the donor and recipient veins. To address the size discrepancy, we adopted a meticulous method, progressively reducing the lumen of the larger recipient vein with simple interrupted sutures. The process began at the 180° end and progressed towards the 0° end. The obliteration continued until the lumen of the larger vein equaled the diameter of the smaller donor vein (Figure 1A). We strategically placed a horizontal mattress suture at the 180° end of the donor vein to fully obliterate the end of the recipient vein (Figure 1B). The anterior and posterior wall sutures were performed using established surgical techniques (Figure 1C).
The entire venous anastomosis procedure, including each detailed step, is documented in Video 1. This video acts as an exhaustive visual resource, offering a deeper insight into the execution and intricacies of the technique. Video 1 can be accessed online at https://doi.org/10.24983/scitemed.imj.2024.00187.
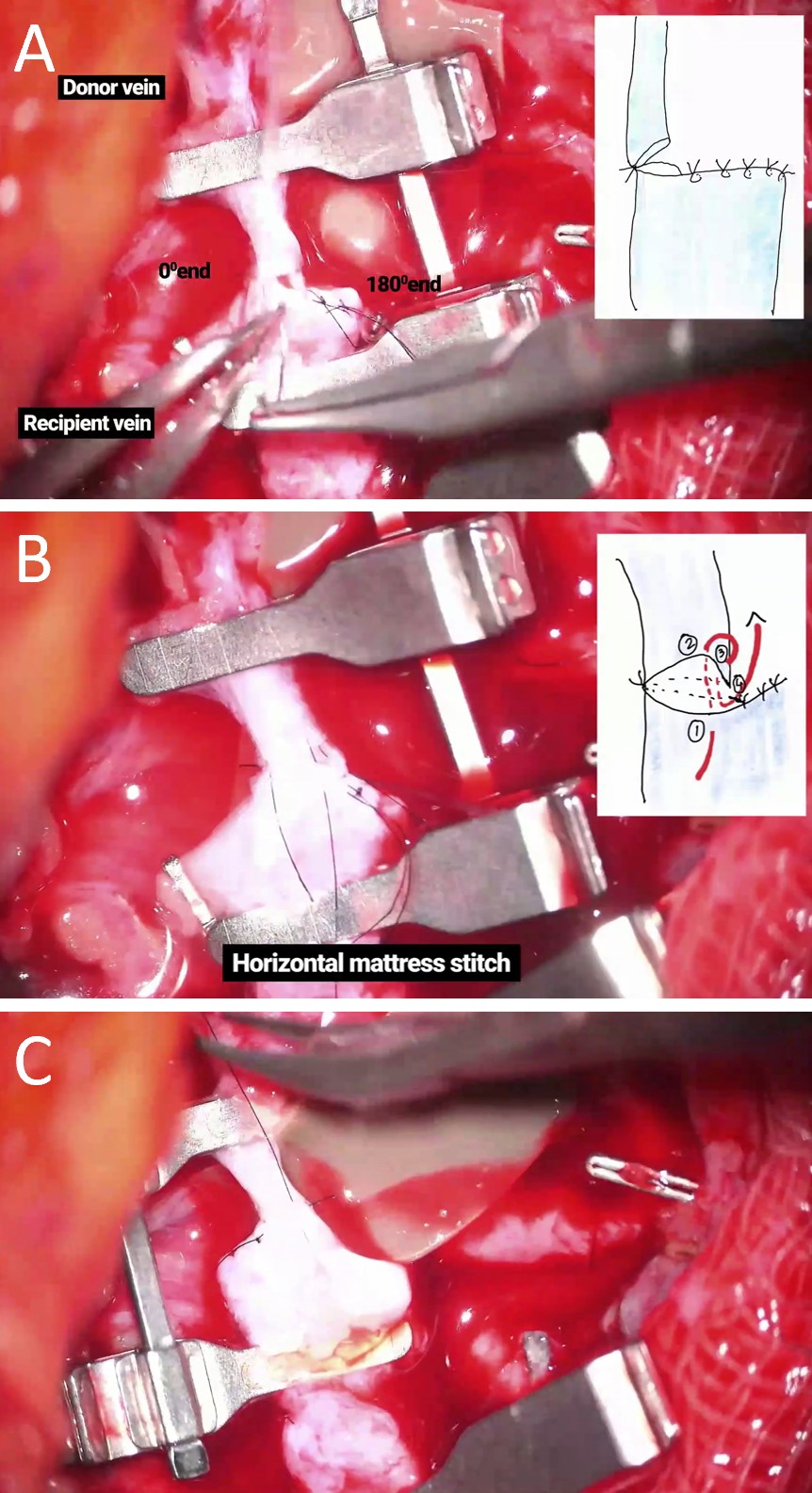
Figure 1. Procedural details of the PLOSEA technique. (A) The 0° end of the donor vein is sutured to the recipient vein. Simple interrupted sutures are employed progressively to obliterate the lumen of the larger recipient vein, initiating at the 180° end and advancing toward the 0° end. Obliteration ceases once the lumen dimensions align with those of the smaller donor vein. (B) A horizontal mattress suture is strategically placed at the 180° end of the donor vein to enhance obliteration of the end of the recipient vein. (C) Anterior and posterior wall sutures are performed in accordance with established surgical protocols to finalize the anastomosis. PLOSEA, partial lumen-obliteration with sutures followed by end-to-end anastomosis.
Conditions involving substantial vessel size discrepancies and limited donor vein lengths are exceedingly rare. Over the past six years, out of more than 500 free flap procedures, we encountered only four cases that exhibited these specific challenges. Notably, such scenarios have not been observed in reconstructions of the extremities or breast, underscoring the unique complexity and rarity of these cases in head and neck reconstructive surgery.
In these four patients treated with the PLOSEA technique, surgical outcomes were uniformly successful, with each case requiring only a single venous anastomosis. All patients demonstrated uneventful healing, with follow-up periods extending to at least six months. Crucially, there were no incidences of venous congestion or flap loss, and no complications were encountered. These results underscore the efficacy and reliability of the PLOSEA technique in managing significant vessel size discrepancies in complex reconstructive cases.
Advancements in Techniques for Vessel Size Discrepancies
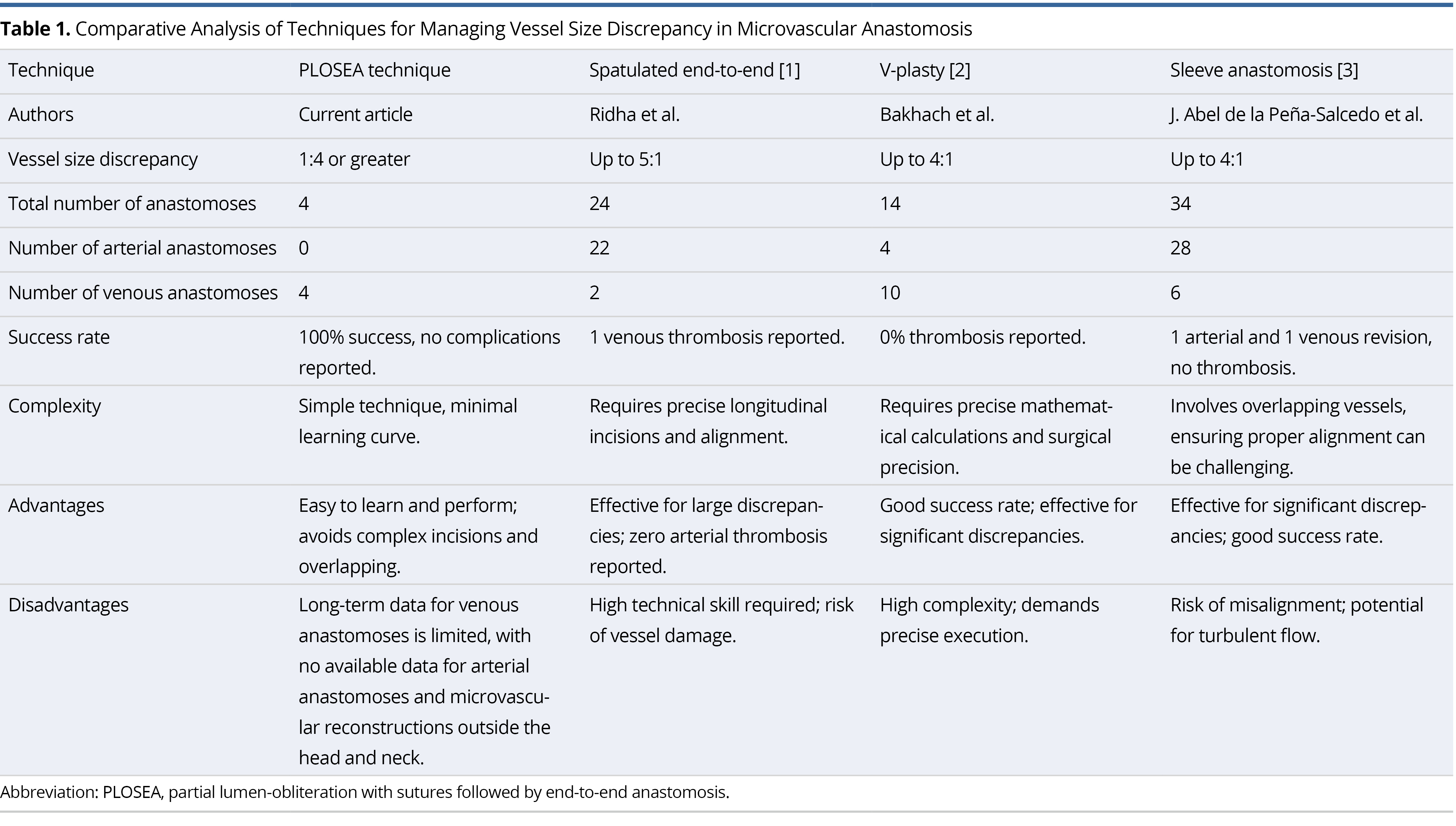
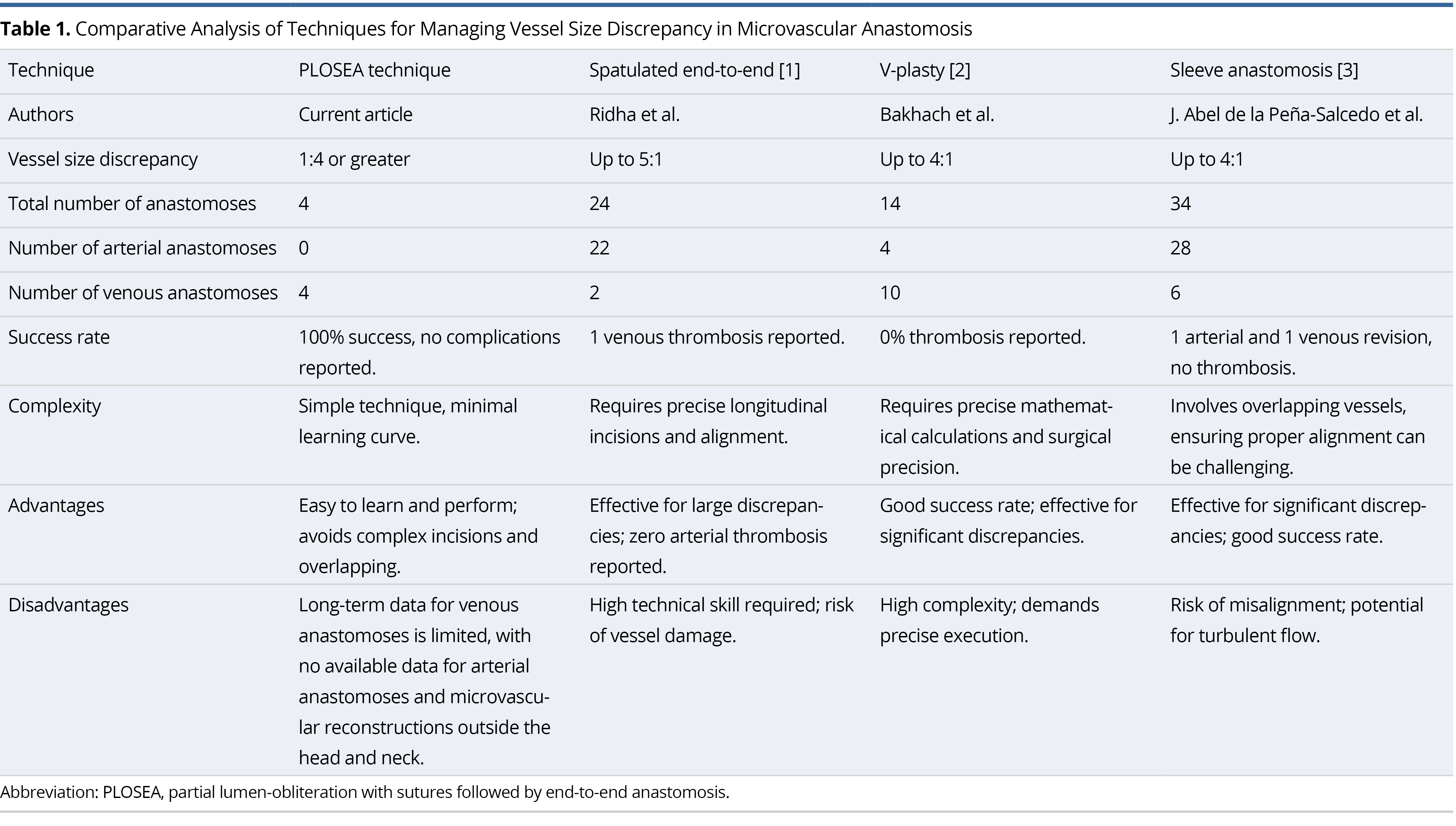
Several surgical techniques have been developed to address the challenges posed by vessel size discrepancies, particularly when they exceed a 1:4 ratio in microvascular surgery. Established methods such as spatulated end-to-end anastomosis [1], V-plasty [2], and sleeve technique [3] are tailored to manage these substantial mismatches. While effective, these approaches often involve complex procedures and require high precision and advanced surgical skills, which may restrict their use and increase the risk of complications in certain scenarios.
The spatulated end-to-end technique, detailed by Ridha H et al. [1], necessitates intricate longitudinal incisions to expand the circumference of the smaller vessel, requiring extensive surgical expertise. In contrast, the PLOSEA technique simplifies this process by using partial lumen-obliteration with simple interrupted sutures and a horizontal mattress corner stitch, thereby reducing procedural complexity.
Similarly, the V-Plasty technique by Bakhach et al. [2] involves precise modifications to the larger vessel, such as creating a V-shaped flap, requiring meticulous calculations and surgical precision. The PLOSEA technique, however, circumvents these complicated steps, offering a more streamlined approach that enhances procedural efficiency.
Additionally, the sleeve anastomosis technique described by de la Pena-Salcedo et al. [3] requires overlapping vessel ends, which can lead to alignment challenges and an increased risk of misalignment and turbulent flow. In contrast, the PLOSEA technique directly reduces the lumen size of the larger vessel to match the smaller one, effectively mitigating the risks associated with overlapping and ensuring a smoother, more predictable outcome. This strategic simplification facilitates mastery for surgeons and enhances the reliability and success rate of surgeries involving substantial vessel size discrepancies.
Table 1 provides a comprehensive comparative analysis of the PLOSEA technique against the above-mentioned methods for managing vessel size discrepancies greater than 1:4. The table details specific parameters and outcomes of each method, including the number of procedures performed, success rates, and the technical demands. Notably, the PLOSEA technique boasts a 100% success rate with no complications reported, underscoring its effectiveness and reliability in surgical settings.
PLOSEA: Optimizing Lumen-Obliteration Technique
The PLOSEA technique relies on fundamental microsurgical skills, particularly suturing, to adjust lumen size. Its straightforward nature facilitates rapid learning and application, making it especially suitable for less experienced surgeons. By eliminating the need for complex incisions and overlaps, this technique significantly reduces complications due to misalignment and turbulent flow. Consequently, it provides a simpler, more accessible method for managing large vessel size discrepancies, making it an attractive option for microsurgeons seeking to reduce procedural complexity and enhance operational efficiency.
Numerous lumen-obliteration techniques have been proposed in the literature [5–6]. For instance, methods involving tapering the larger vessel through wedge excision and performing an end-to-end anastomosis have been documented [5], although they lack detailed descriptions. Suri et al. introduced a ligaclip technique for tapering and obliterating the larger lumen [6]. While promising, this method demands significant expertise due to its irreversible nature. In our series, we have not applied tapering to the wider vessels; however, employing either of the mentioned techniques is feasible. Nevertheless, our instructional video demonstrates that partial lumen-obliteration of the larger vessel with sutures, followed by end-to-end anastomosis, provides a straightforward yet highly effective solution for specific clinical scenarios.
Potential Complications of PLOSEA
The consistent success and lack of complications associated with the PLOSEA technique underscore its potential as a preferred method for similar surgical procedures. Its effectiveness in facilitating successful anastomosis despite substantial size discrepancies makes it especially valuable for reconstructive surgeons, particularly in head and neck surgery where these challenges are more common.
However, potential complications may arise with this procedure, including intimal damage, stenosis, and thrombosis. Adhering to traditional principles of microvascular anastomosis, such as accurate lumen matching and precise horizontal mattress corner suturing, is crucial for mitigating these risks. The patency of the anastomosis can be confirmed using Acland’s test.
Turbulent flow across the anastomosis, caused by sudden transitions in vessel sizes, is a known risk factor for thrombosis. In our case series, the internal jugular vein was used as the recipient vein. The inspiratory fall in intrathoracic pressure created a suction effect on venous return, minimizing the risk of stasis and turbulence in the larger vein. Consequently, we did not taper the larger vessel, a tributary of the internal jugular vein, due to this unique physiological advantage.
Pitfalls and Solutions
We have exclusively applied the PLOSEA technique for venous anastomosis in head and neck reconstructions, specifically using the internal jugular vein as the recipient vein. Due to the absence of a “sulking effect” in other veins, we recommend tapering the wider lumen vein either with a clip or with wedge excision followed by suturing. This strategy may reduce the likelihood of stasis and thrombosis. In these specific cases, the sequence of procedures may differ from the standard PLOSEA approach. It is advisable to taper the wider vein lumen after completing the anastomosis. This adaptation ensures a tailored approach to effectively address unique surgical challenges.
We have not yet used this technique for arterial anastomosis. In situations with a significant size mismatch where end-to-side anastomosis is not feasible, the PLOSEA technique could theoretically be applied. However, it should be approached with caution when used for arterial anastomosis. Tapering the wider lumen is crucial to prevent turbulence, stasis, and the associated risk of thrombosis. Alternatively, the branched interpositional vein grafting technique can be considered [4]. Further studies and clinical trials are recommended to evaluate the safety and efficacy of using the PLOSEA technique for arterial anastomosis.
Study Limitations
The limitations of this study include a small sample size and the absence of a control group, largely due to the rarity of the technique’s indications. Despite the challenges, future validation through large-scale clinical trials and the establishment of a control group are essential to confirm the technique’s efficacy.
In high-volume microsurgical practices involving head and neck, extremity, and breast reconstructions, we have encountered a variety of vessel wall discrepancies over the years. In our experience, no single method is universally applicable. Depending on the size discrepancy, we have employed most of the techniques discussed. Microsurgeons should be prepared to encounter unusual circumstances and should be capable of applying the appropriate technique safely and reliably. We believe the proposed PLOSEA technique is beneficial for this rare subset of patients with significant size discrepancies. This video demonstration would be particularly helpful to young microsurgeons early in their learning curve.
The PLOSEA technique has demonstrated consistent success and no complications in managing significant vessel size discrepancies in head and neck reconstructive surgery. Its simplicity and reduced complexity make it an appealing option for microsurgeons, offering a reliable solution that does not require specialized skills. While effective in venous anastomosis, further research is recommended to validate its safety and efficacy in other contexts, including arterial anastomosis and reconstructions of anatomical regions requiring microvascular anastomosis, such as the extremities and breast. This video demonstration serves as a valuable resource, aiding young microsurgeons in mastering the technique and improving surgical outcomes.
Received date: June 10, 2024
Accepted date: July 08, 2024
Published date: July 22, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)’ autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Video 1. Demonstration of the PLOSEA technique in major vessel size mismatch for venous anastomosis. PLOSEA, partial lumen-obliteration with sutures followed by end-to-end anastomosis.
A novel technique of sequential ETS micro-venous anastomoses using three vessel loops for IJV occlusion and a single vascular clamp to retract and hold the anastomoses sites in position.
The authors present a novel synthetic vascular model for microanastomosis training. This model is suitable for trainees with intermediate level of microsurgical skills, and useful as a bridging model between simple suturing exercise and in vivo rat vessel anastomosis during pre-clinical training.
Improving efficiency of microvascular anastomosis by combination of open-loop and airborne suture techniques.
Authors report a case of lower extremity lymphedema treated by LVA that preoperatively mapped not only lymphatic vessels by PDE, but also veins and venules using Veinsite™ .
Combining intraoperative ICG lymphography with NIR vein visualization can aid supermicrosurgeons in identifying lymphatic vessels and superficial venules to guide LVA incision placement. This guided approach significantly improves successful creation of LVAs when compared to the blind (anatomic) approach. In addition, the absence of linear ICG lymphographic patterns does not prevent formation of successful LVAs.
Immediate limb compression following the LVA procedure facilitates lymphatic drainage and increases the surgical efficacy by increasing the number of functioning anastomoses, and is a recommended postoperative practice.
Optimum operating conditions are an integral part of a successful microvascular surgery. We hereby introduce a new technique to make a low- cost microsuction cannula, which will be helpful for microvascular surgeons.
Traditionally, suturing techniques have been the mainstay for microvascular anastomoses, but owing to its technical difficulty and labour intensity, considerable work has gone into the development of sutureless microvascular anastomoses. In this review, the authors take a brief look at the developments of this technology through the years, with a focus on the more recent developments of laser-assisted vascular anastomoses, the unilink system, vascular closure staples, tissue adhesives, and magnets. Their working principles, with what has been found concerning their advantages and disadvantages are discussed.
This case report demonstrates an important supermicrosurgical technique for lymphedema, which was established by Isao Koshima in 1994. So far, over 2,000 cases of limb edema have been treated by this surgical method.
LVA and vascularized lymph node transfer VLNT are established lymphedema treatments. However, LVA is only effective for early disease and VLNT can cause donor-site lymphedema and contour deformity. VLVT is free of these limitations. The authors described their experience of a new VLVT technique.
Authors proposed a simple innovative technique that helps in achieving a clear surgical field at the time of venous repair by diverting the venous bleeding through a glove finger and at the same time preventing venous congestion of the flap.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
Authors discuss a silicone tube that provides structural support to vessels throughout the entire precarious suturing process. This modification of the conventional microvascular anastomosis technique may facilitate initial skill acquisition using the rat model.
This article presents a case study on the successful replantation of a pediatric lower lip after a dog bite, focusing on artery-only microanastomosis. It highlights the challenges and effective strategies in pediatric microvascular surgery, particularly emphasizing the importance of specialized surgical techniques and thorough postoperative care. Alongside the case study, an extensive literature review supports the feasibility of artery-only anastomosis and the traditional yet critical use of leech therapy for managing venous congestion. This research is vital for medical professionals specializing in pediatric surgery, offering key insights into improving both functional and aesthetic outcomes for young patients. Additionally, it identifies gaps in long-term research and stresses the need for ongoing studies to refine treatment protocols, making it an indispensable resource for enhancing patient care and outcomes in pediatric reconstructive surgeries.
A novel technique of sequential ETS micro-venous anastomoses using three vessel loops for IJV occlusion and a single vascular clamp to retract and hold the anastomoses sites in position.
Authors proposed a simple innovative technique that helps in achieving a clear surgical field at the time of venous repair by diverting the venous bleeding through a glove finger and at the same time preventing venous congestion of the flap.
This article provides a practical and effective technique for managing significant vessel size discrepancies in microvascular anastomosis, focusing on partial lumen obliteration with a horizontal mattress corner stitch. The method is particularly suited for discrepancies of 1:4 or greater, addressing a common challenge in reconstructive surgery. Readers in the medical field will find this study valuable for its straightforward and reproducible approach, which offers a solution with a minimal learning curve. The article's importance lies in its potential to improve surgical outcomes and efficiency, making it a must-read for practitioners seeking to enhance their skills in microsurgery. The expertise demonstrated in this study supports its merit for publication, provided that specific aspects are addressed and resolved. This article showcases a solid, practical contribution to the field of reconstructive surgery.
This article addresses a crucial aspect of reconstructive surgery by presenting a technique for managing significant vessel size discrepancies in microvascular anastomosis, specifically using partial lumen obliteration with a horizontal mattress corner stitch. This method is particularly relevant for discrepancies of 1:4 or greater, which are common and challenging in surgical practice. The practical nature of this approach is noteworthy for its simplicity and ease of replication, potentially improving surgical efficiency and patient outcomes. However, the study's impact is limited by its small sample size, with only four cases presented. This restricts the ability to draw robust conclusions and generalize the findings. To meet the rigorous standards of publication, additional data from larger clinical trials are necessary to validate the technique's efficacy and safety comprehensively. While the current findings are promising, the presence of these critical issues suggests the article is not yet fit for publication in its current guise.
This article makes a valuable contribution to plastic surgery by introducing a technique for managing large vessel size discrepancies in microvascular anastomosis. The authors report successful outcomes in four cases over six years, but more detailed long-term follow-ups are necessary. It’s important to identify specific patient selection criteria, such as age, comorbidities, and defect type. The technique should address intraoperative challenges, especially the risks of turbulence and thrombosis from angled anastomosis. Ensuring a smooth transition and alignment between vessels is crucial. This practical and replicable approach offers valuable insights for improving surgical efficiency and patient outcomes, potentially advancing microsurgical procedures in plastic surgery. The article has the potential for publication, pending a few minor corrections.
Naalla R, Samantaray SA. A simplified technique for large vessel size discrepancies: Partial lumen-obliteration with sutures followed by end-to-end anastomosis. Int Microsurg J 2024;8(1):4. https://doi.org/10.24983/scitemed.imj.2024.00187