Objective: The resection of the recurrent laryngeal nerve (RLN) during thyroid cancer surgery frequently results in vocal cord paralysis. Restoration techniques such as direct anastomosis and ansa cervicalis-to-RLN anastomosis aim to regain function. Traditional diagnostic methods often yield inconclusive evidence of reinnervation, highlighting the necessity for electrophysiological evaluations. This research provides the first definitive confirmation of this process in human subjects.
Methods: In this retrospective study, we analyzed three patients who underwent RLN repair and subsequent reoperation due to recurrent thyroid cancer. Intraoperative nerve monitoring was employed to assess vocal cord function and confirm reinnervation through electrophysiological evidence. Electromyographic responses were systematically recorded during electrical stimulation of the nerve central to the anastomosis.
Results: Electromyographic responses were recorded in all patients, confirming successful reinnervation of the vocalis muscles post-RLN repair. Electrical stimulation of the nerve central to the anastomosis elicited clear responses in the vocalis muscles, with amplitudes ranging from 406 to 868 μV, which were sufficiently large compared to those on the contralateral side. Stimulation of the ipsilateral vagus nerve did not evoke a vocalis response in patients who underwent ansa cervicalis-to-RLN anastomosis. The results demonstrated that the reinnervation was both targeted and effective, providing substantial evidence of the efficacy of the surgical techniques used in restoring vocal cord function.
Conclusion: This study presents the first electrophysiological evidence of vocalis muscle reinnervation following RLN repair in humans, signifying a groundbreaking advancement in nerve repair. Utilizing intraoperative nerve monitoring, we confirmed successful reinnervation through clear electromyographic responses, highlighting the essential role of these assessments in clinical practice. This pioneering research redefines the standards for RLN repair, emphasizing the critical importance of precision in surgical techniques and rigorous postoperative monitoring. It paves the way for future medical innovations and offers renewed hope for patients, promising enhanced recovery and improved vocal cord function.
Numerous studies have chronicled phonation recovery in patients who have undergone recurrent laryngeal nerve (RLN) repair following its resection due to thyroid cancer invasion or accidental damage [1–4]. Techniques for RLN repair vary, including direct anastomosis of severed ends, free nerve grafting to bridge gaps, and ansa cervicalis-to-RLN anastomosis [2]. Despite these repairs, the ipsilateral vocal fold typically remains fixed in a median position and does not resume normal movement. However, it does recover from atrophy, regains tension during phonation, and ultimately restores phonatory function. This recovery process is often attributed to misdirected regeneration of adductor and abductor nerve fibers [2].
While several reports detail phonatory tests and laryngoscopic findings post-RLN repair [4–7], direct electrophysiological evidence of vocalis muscle reinnervation remains elusive. This study presents three cases where such reinnervation following RLN repair was confirmed electrophysiologically. Using intraoperative nerve monitoring techniques during surgeries for recurrent thyroid cancer, we documented this reinnervation. To our knowledge, this is the first documented instance of electrophysiological evidence of vocalis muscle reinnervation following RLN repair in humans.
The central research question of this study is whether electrophysiological methods can conclusively demonstrate reinnervation of the vocalis muscles following RLN repair in humans. The objectives are twofold: firstly, to evaluate the functionality of the vocalis muscles via electromyographic responses during surgery; secondly, to correlate these responses with observed vocal cord function, providing a direct and innovative method for assessing the efficacy of nerve repair in clinical settings.
Study Design and Setting
This retrospective study was conducted at Kuma Hospital, focusing on patients who required additional surgeries for recurrent thyroid cancer after initially recovering phonatory function following RLN repair. The study adhered to the ethical principles of the Helsinki Declaration, with all participants providing informed consent for their data to be used in this research.
Participants
Patients included in this study met specific criteria: a history of RLN repair due to thyroid cancer, subsequent recovery of phonatory function, and the necessity for reoperation due to recurrent thyroid cancer. Between 1998 and 2023, RLN repair was performed on 592 patients at Kuma Hospital. Among these, three cases involved loco-regional recurrence necessitating further neck surgery, making them suitable candidates for this electrophysiological study.
Diagnostic Tools
For the patients in this study, the diagnostic process involved a comprehensive array of tools to ensure an exhaustive evaluation of the thyroid and its adjacent structures. This included ultrasound, laryngoscopy, fine-needle aspiration cytology, and computed tomography (CT) scans.
Surgical Interventions
Each surgery in this study was performed under general anesthesia, with meticulous monitoring of RLN integrity to ensure the nerve’s preservation. Surgical techniques, including nerve anastomosis and tumor resection, were standardized and executed using microsurgical instruments to guarantee precision across all cases. The surgical strategies were customized for each patient, taking into account the extent of cancer spread and individual patient needs. Foundational procedures commonly included total thyroidectomy and central neck dissection. For more complex cases, the surgical regimen was expanded to incorporate modified neck dissections and lymph node resections. This tailored approach aimed to provide optimal surgical outcomes by specifically addressing the unique anatomical and clinical challenges posed by each patient’s thyroid cancer progression.
Electrophysiological Monitoring
Intraoperative neuromonitoring was conducted using the NIM-Response 3.0 system (Medtronic, Jacksonville, FL, USA). This involved recording electromyographic responses from the vocalis muscles during electrical stimulation of the RLN and the ansa cervicalis, both before and after anastomosis procedures. Normal electromyographical responses were established based on comparisons with measurements from the unaffected contralateral muscles. Any significant deviations from these normative values were categorized as abnormal, providing a clear benchmark for assessing nerve functionality during surgery.
Statistical Methods
Given the nature of this case series, statistical analysis was not the primary focus; however, descriptive statistics were used to delineate the range and consistency of the electromyographic amplitudes. Observational data were also presented, illustrating clinical outcomes and providing electrophysiological evidence of nerve functionality.
Uniform electromyographic amplitudes across all patients indicate effective reinnervation of the vocalis muscles. This consistency confirms the reliability of the surgical outcomes and validates the efficacy of the employed nerve repair techniques, emphasizing their significant impact on enhancing vocal function after RLN repair.
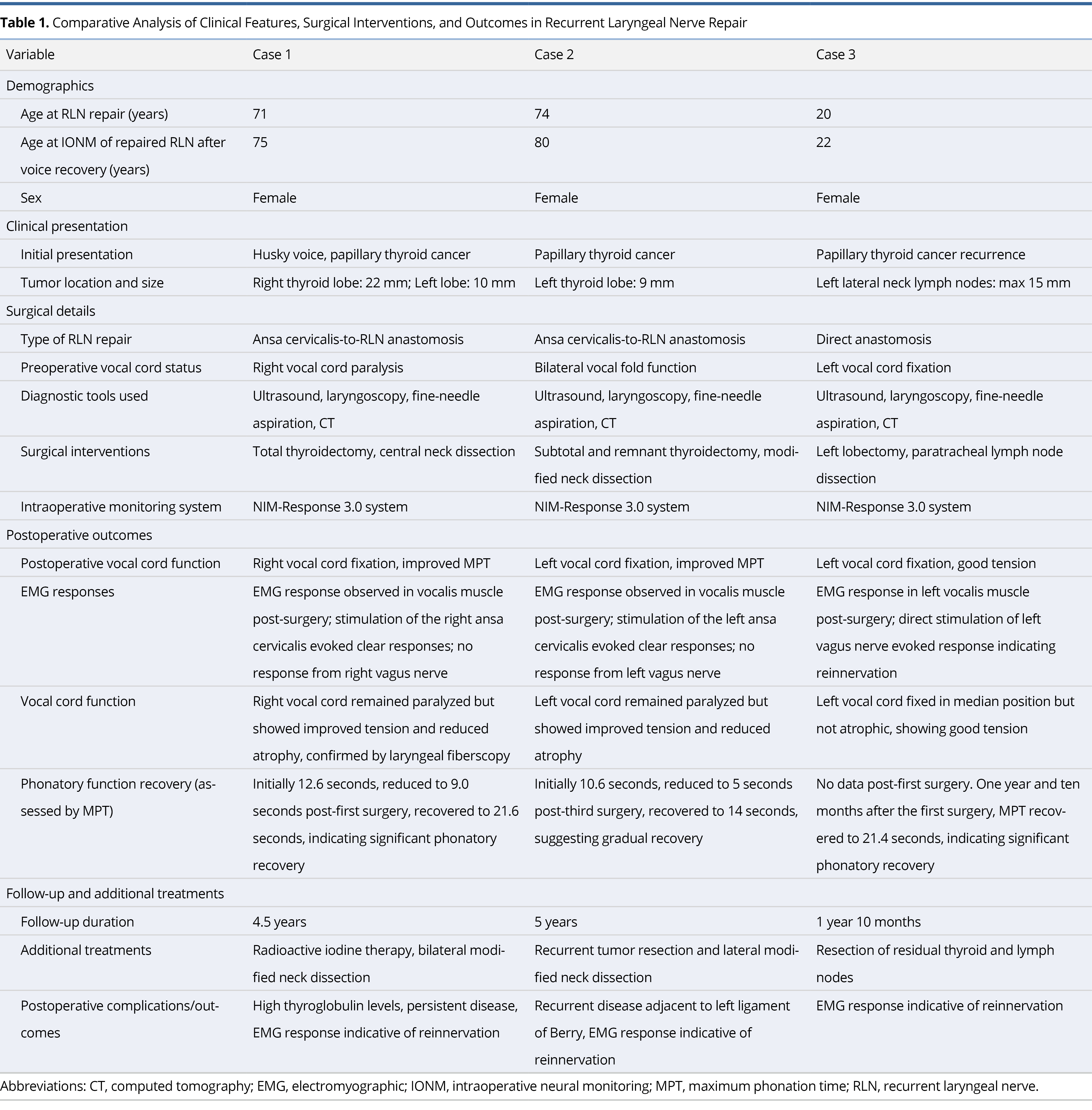
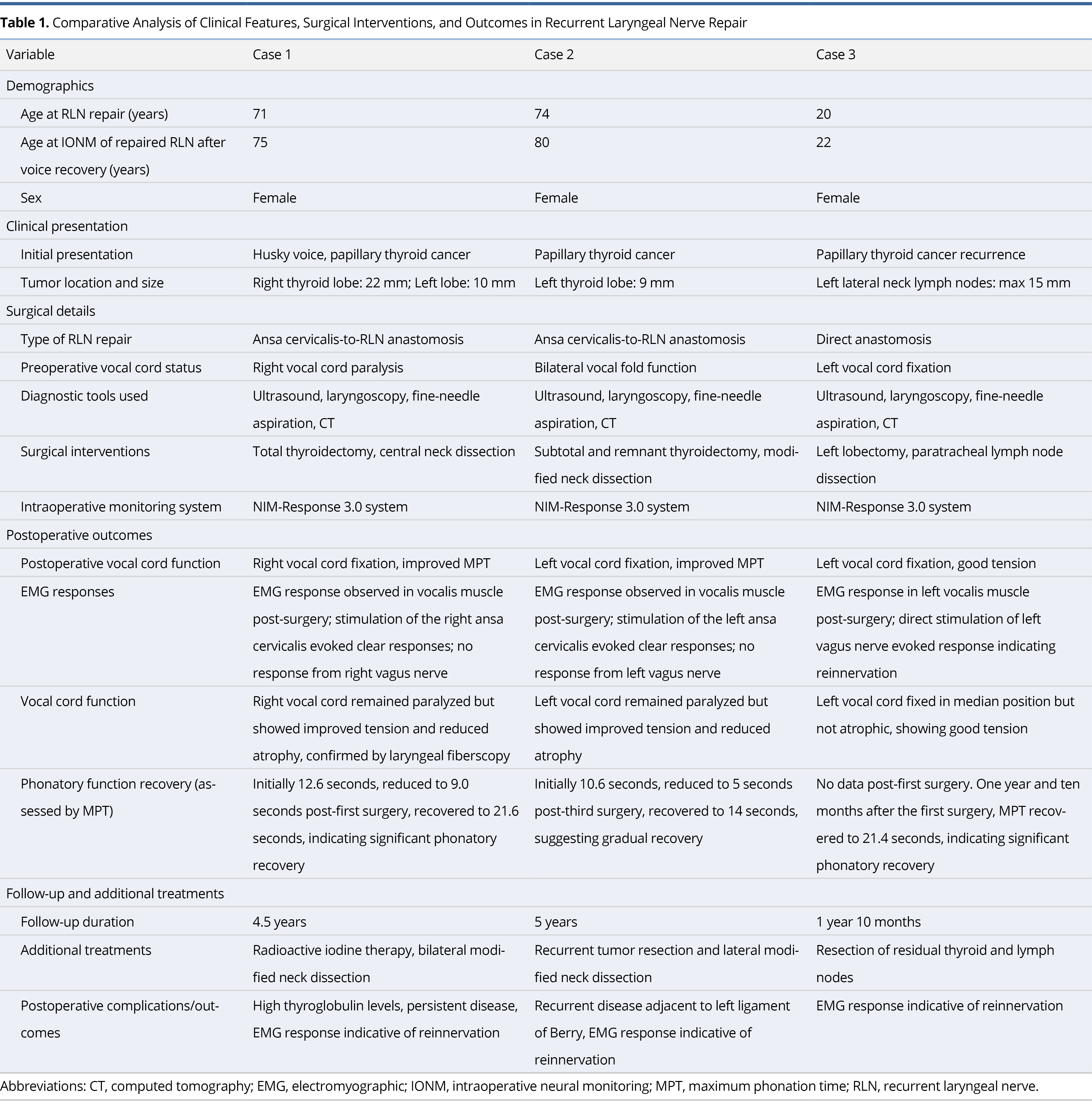
Table 1 comprehensively details the results from intraoperative neuromonitoring and postoperative vocal cord function assessments. This table presents a comparative analysis of the three cases involved in the study, meticulously documenting electromyographic responses during surgery. Furthermore, Table 1 encompasses a broad spectrum of clinical features, surgical interventions, and outcomes, providing a holistic view of the efficacy and implications of the RLN repair techniques employed. This structured presentation aids in clearly understanding the clinical and electrophysiological parameters critical to evaluating the success of RLN repairs.
Patient Demographic Details
This study involved three female patients who underwent RLN repair, aged between 20 and 74 years at the time of the procedure. This range underscores the procedure’s relevance across diverse life stages. Follow-up intraoperative neuromonitoring occurred when the patients were aged 22, 75, and 80, respectively. These evaluations, carried out between two to six years after the initial repair, demonstrate the long-term effectiveness of the procedure. The results highlight its applicability and potential to sustain phonatory function recovery in both younger and older populations, reinforcing its significant demographic and clinical value.
Type of RLN Repair
The surgical techniques for RLN repair employed in this study varied across the three patients, facilitating a comparative analysis of different methods. Two patients underwent ansa cervicalis-to-RLN anastomosis, utilizing the ansa cervicalis nerve for reconnection, while the third patient received direct anastomosis, which involved directly reconnecting the severed RLN ends. This variation in approaches allowed for a detailed examination of the efficacy of each method, providing crucial data on their respective outcomes and enhancing our understanding of surgical options for RLN repair.
Postoperative Outcomes
Postoperatively, all patients exhibited some degree of vocal cord fixation, but significant improvements in muscle tension and reduced atrophy were confirmed by electromyographic responses and laryngoscopic examinations. Importantly, the electromyographic responses validated successful reinnervation of the vocalis muscles, with no responses observed from the corresponding vagus nerves. This outcome highlights the precision and effectiveness of the RLN repair techniques, demonstrating their targeted impact in restoring vocal cord function while preserving the integrity of adjacent nerve pathways.
Phonatory Function Recovery
Maximum phonation time (MPT) served as a crucial metric for assessing the recovery of phonatory function in each patient, showing significant improvements over time. This measure is essential for evaluating the efficacy of surgical interventions designed to restore vocal function. The consistent increase in MPT across all cases underscores the effectiveness of the employed recurrent laryngeal nerve repair techniques, confirming the surgical success in enhancing patients’ vocal capabilities.
Follow-up and Additional Treatments
The follow-up duration for patients in this study ranged from one year and 10 months to five years. During this period, individual patients occasionally required additional interventions to address persistent or recurrent issues related to their initial conditions. These interventions included radioactive iodine therapy, commonly employed to eradicate residual thyroid tissue or treat metastasized thyroid cancer cells. Additionally, some patients underwent further surgeries to manage recurrent disease or complications, such as persistently high thyroglobulin levels, an indicator of residual thyroid cancer. These extended follow-up periods and additional treatments underscore the complexity of thyroid cancer management and the necessity for continuous monitoring and intervention.
Case 1: Ansa Cervicalis-to-RLN Anastomosis
A 75-year-old Japanese woman with a husky voice was referred to our hospital for papillary thyroid cancer treatment. The ultrasound examination revealed tumors measuring 22 mm in diameter in the right thyroid lobe and 10 mm in the left lobe. The fine-needle aspiration cytology confirmed both tumors as papillary thyroid carcinomas. The laryngoscopy showed paralysis of the right vocal cord, with an MPT of 12.6 seconds. The ultrasonography and the neck CT indicated that the right tumor was located adjacent to the right RLN and trachea. No lymph nodes or pulmonary metastases were detected. According to the Union for International Cancer Control (UICC) classification, the patient’s cancer stage was III (T4a, N0, M0).
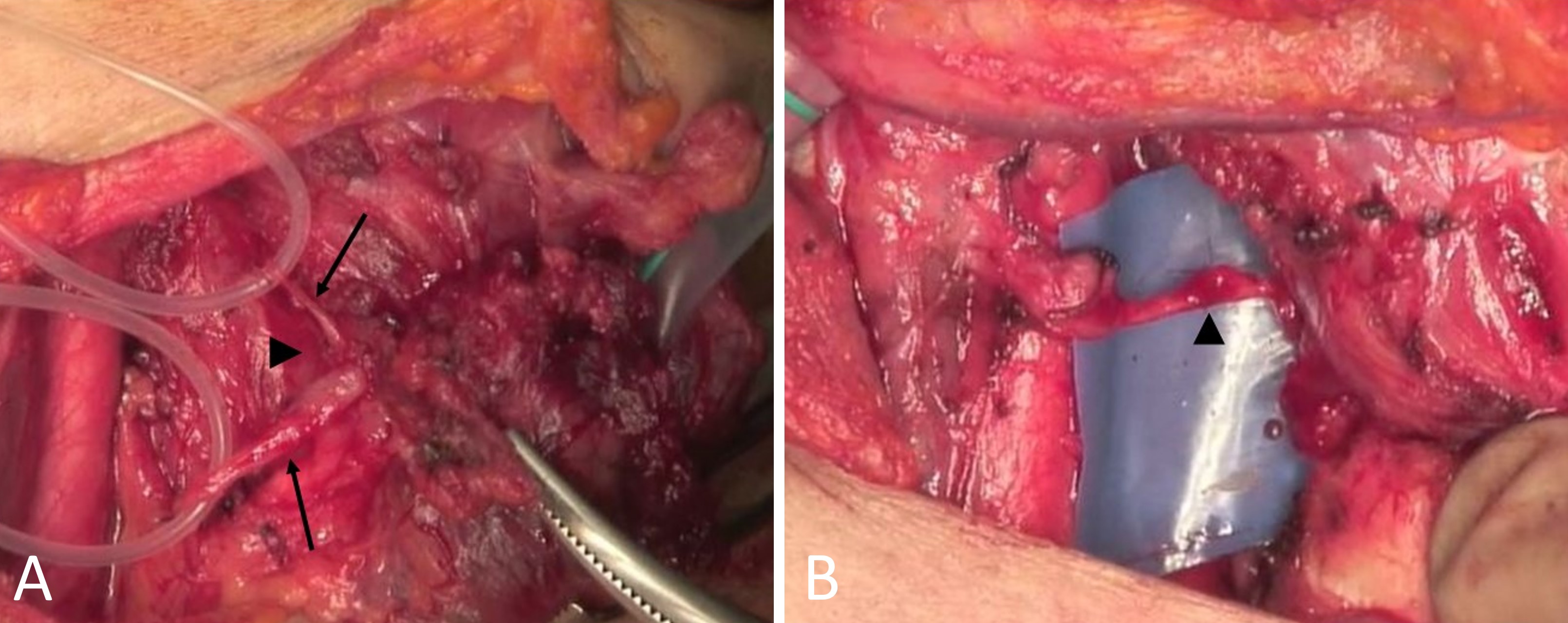
A total thyroidectomy and central neck dissection, along with right RLN repair, were planned. The patient was administered general anesthesia using an endotracheal tube with surface electrodes. The integrity of the RLN and the external branch of the superior laryngeal nerve were monitored using the NIM-Response 3.0 system. Initial stimulation of the right vagus nerve and central portion of the right RLN showed no vocalis muscle response. The right RLN and trachea were involved by the tumor near Berry’s ligament. To expose the peripheral portion of the RLN, the inferior pharyngeal constrictor muscle was divided, a procedure termed the “laryngeal approach” (Figure 1A) [8]. The cancer-invaded segment of the RLN and a partial layer of the trachea were resected. The intraoperative neuromonitoring ensured the preservation of the left RLN.
Following the total thyroidectomy and central compartment dissection, the ansa cervicalis-to-right-RLN anastomosis was performed (Figure 1B). The end-to-end nerve anastomosis was executed with two stitches using 8-0 nylon thread under 2.5× magnification with microsurgical instruments. The postoperative laryngoscopic examination revealed normal movement of the left vocal cord and paralysis of the right vocal cord.

Figure 1. Intraoperative visualization in Case 1. (A) Tumor invasion at Berry's ligament, indicated by a large arrowhead. The peripheral segment of the right RLN is exposed by dividing the inferior pharyngeal constrictor muscle using a laryngeal approach. Smaller arrows distinguish the peripheral and central segments of the right RLN, enhancing anatomical clarity. (B) Ansa cervicalis-to-right RLN anastomosis highlighted by an arrowhead, demonstrating a critical technique for nerve function restoration post-tumor resection. RLN, recurrent laryngeal nerve.
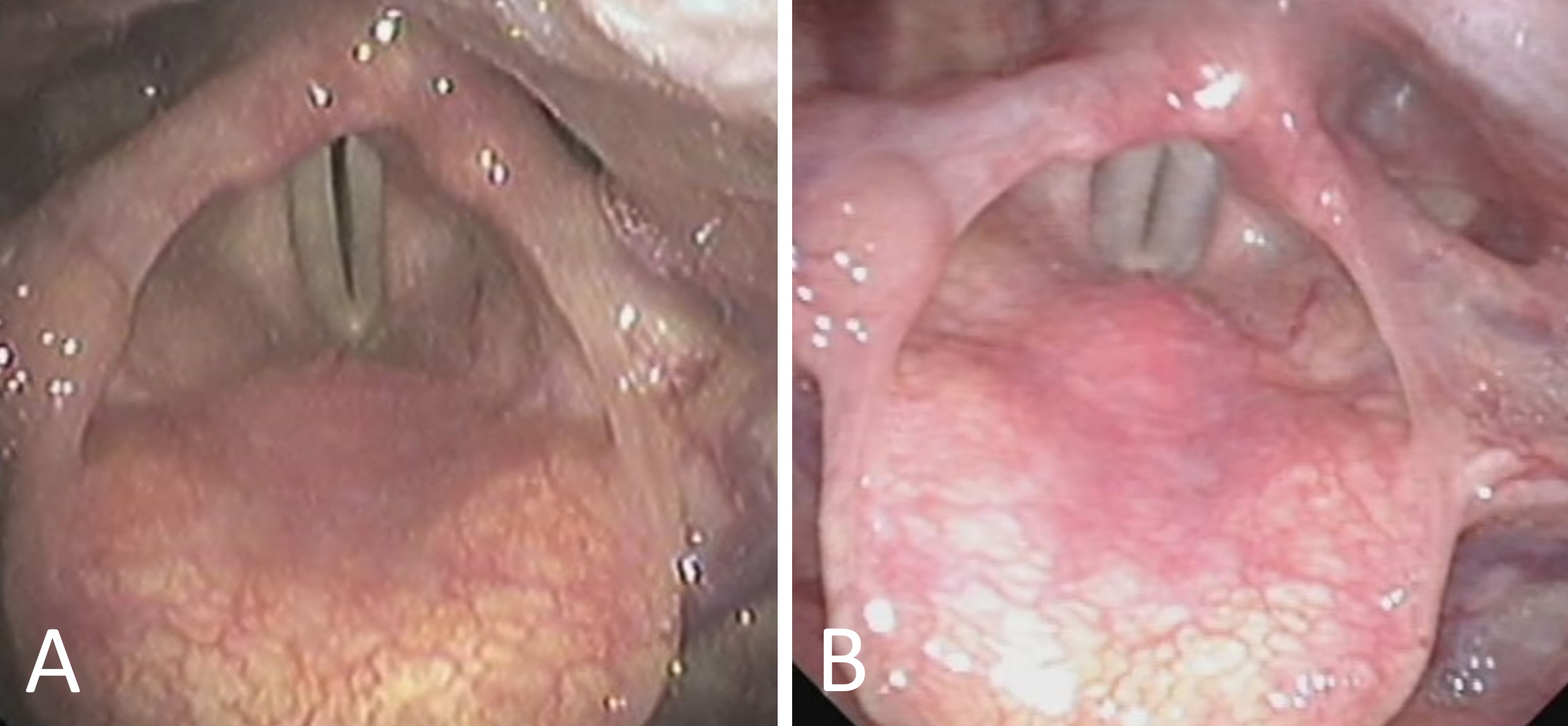
The postoperative evaluations included periodic MPT and laryngoscopic examinations. The MPT values progressively increased to 9.0, 10.9, 14.9, and 21.6 seconds at 1, 3, 6, and 12 months post-surgery, respectively. The patient’s hoarseness resolved three months after surgery. The laryngoscopic examination one month post-surgery showed slight atrophy of the right vocal cord and a small gap between the cords during phonation (Figure 2A). Twelve months post-surgery, the right vocal cord remained immobile at the midline but displayed good tension and a narrowed gap during phonation (Figure 2B).
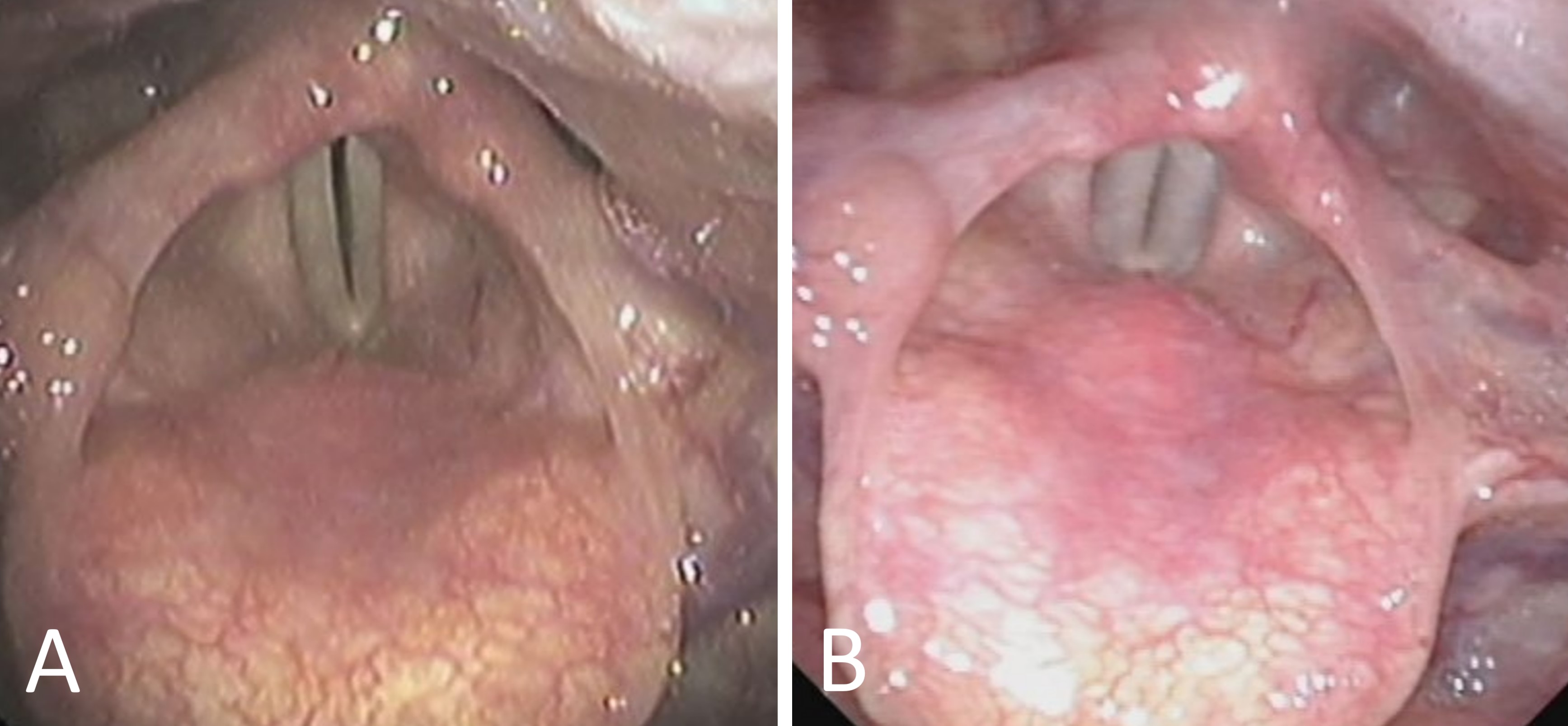
Figure 2. Postoperative laryngoscopic assessments in Case 1. (A) One-month follow-up reveals slight atrophy and a pronounced phonation gap in the right vocal cord, indicating early recovery challenges. (B) Twelve-month follow-up shows the right vocal cord at midline with improved tension and a reduced phonation gap, demonstrating successful surgical recovery.
At eight months and again three years post-surgery, the patient underwent radioactive iodine therapy sessions (30 mCi and 100 mCi, respectively), with no suspicious accumulation observed. However, high serum thyroglobulin levels persisted. Four years post-surgery, the ultrasound examination detected suspicious bilateral neck lymph nodes. The fine-needle biopsy confirmed metastatic papillary thyroid carcinoma in these nodes. The CT scans revealed no pulmonary metastases.
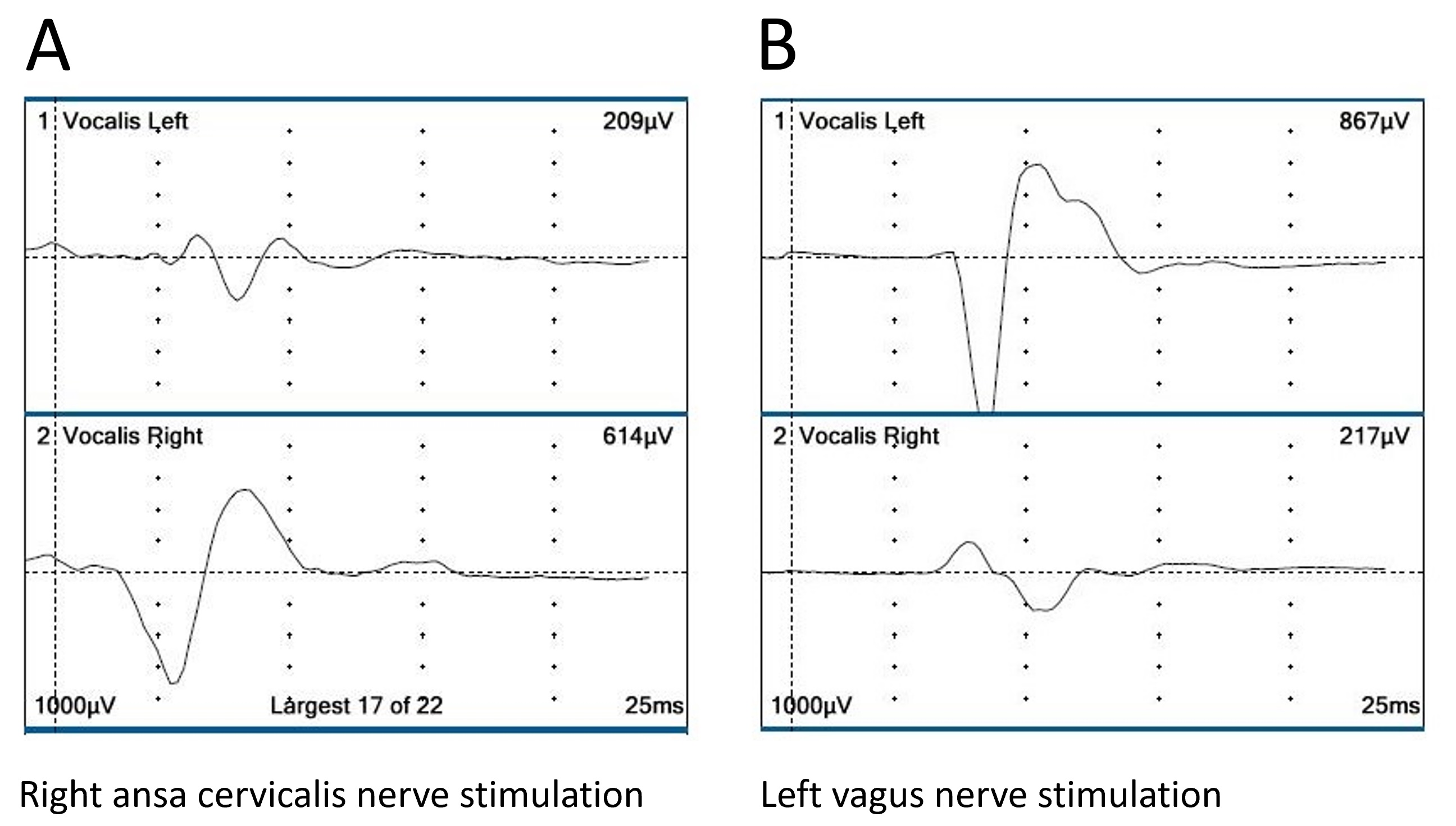
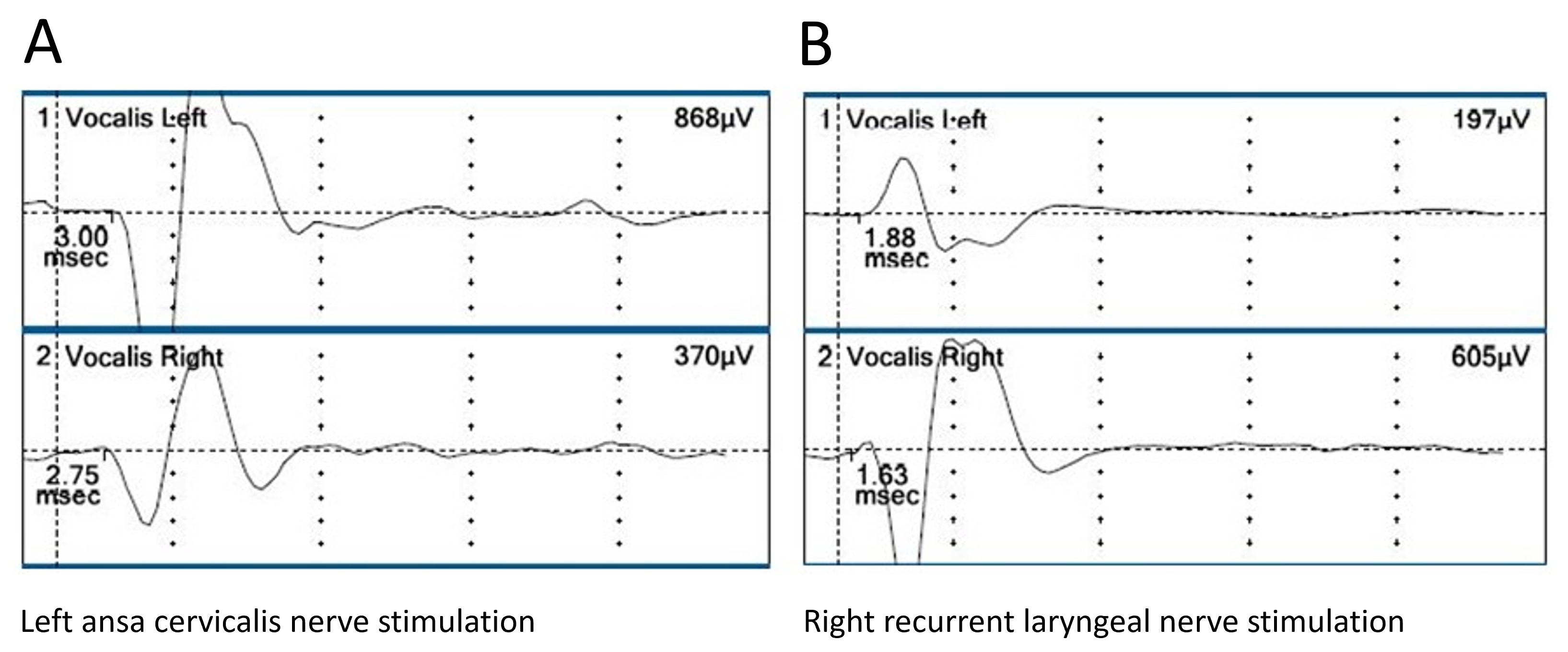
Four and a half years after the initial surgery, a bilateral modified neck dissection was performed. During this reoperation, general anesthesia was administered using an endotracheal tube with surface electrodes. The same nerve monitoring system was used to evaluate the RLN, vagus nerve, and right ansa cervicalis-to-RLN network. The electrical stimulation of the right ansa cervicalis evoked a clear electromyographic response in the right vocalis muscle (Figure 3A), whereas the stimulation of the right vagus nerve did not. Stimulation of the left vagus nerve produced a normal electromyographic response in the left vocalis muscle (Figure 3B).
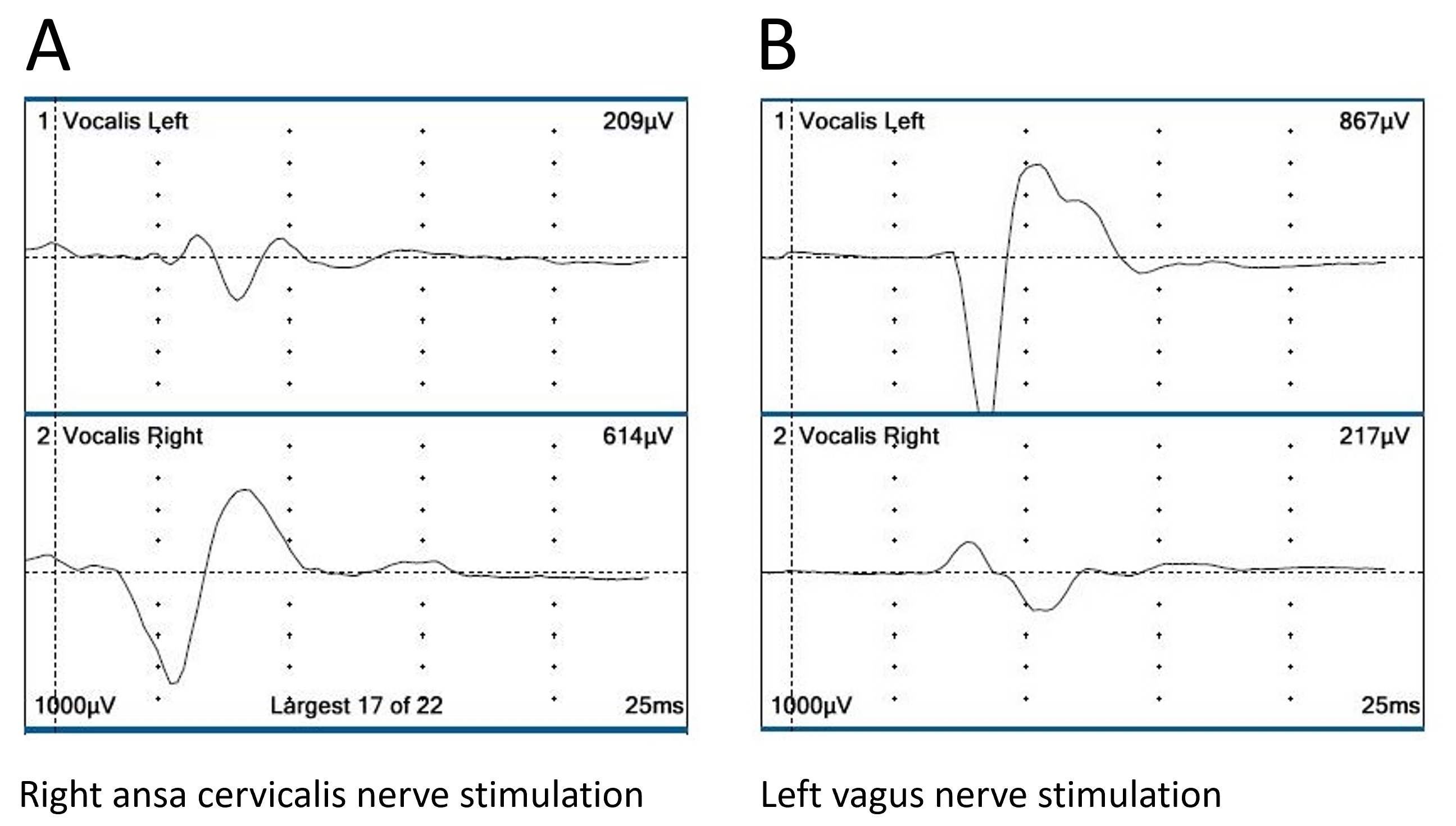
Figure 3. Electromyographic responses from right ansa cervicalis-to-right RLN anastomosis in Case 1. (A) Robust response in the right vocalis muscle following right ansa cervicalis nerve stimulation, indicating successful reinnervation. (B) Normal response in the left vocalis muscle following left vagus nerve stimulation, confirming intact neuromuscular function on the non-operated side. RLN, recurrent laryngeal nerve.
Case 2: Ansa Cervicalis-to-RLN Anastomosis
A 59-year-old Japanese woman initially underwent a subtotal thyroidectomy and left modified neck dissection for papillary thyroid cancer. At age 65, she underwent a remnant thyroidectomy and right-modified neck dissection due to disease recurrence. Eight years later, the patient experienced a recurrence near Berry’s ligament on the left and developed right lateral neck lymph node metastases. Despite not having hoarseness, her MPT was 10.6 seconds, and the laryngoscopy revealed bilateral vocal fold function. The patient subsequently underwent a third surgical procedure. According to the UICC classification, her cancer stage at that time was Stage III (T4a, N1b, M0).
The tumor adjacent to Berry’s left ligament invaded the left RLN, necessitating resection of this nerve segment along with the tumor. The nerve was then repaired using left ansa cervicalis-to-left RLN anastomosis, performed in an end-to-end manner with three stitches of 8-0 nylon thread. Postoperatively, the patient developed hoarseness, with an MPT of 5 seconds three months after the third surgery. However, her hoarseness symptoms resolved within a year, and her MPT improved to 14 seconds.
Five years after the third surgery, the periodic ultrasound examinations revealed an increase in the size of the right lateral neck lymph nodes and subcutaneous tumors superficial to Berry’s ligament on the left. A fine-needle biopsy confirmed these as metastatic papillary thyroid cancer. Following these findings, the patient underwent resection of the lymph node metastasis and the recurrent tumor.
The general anesthesia was administered using an endotracheal tube with surface electrodes. The nerve monitoring system was used to assess the activity of the right RLN and the anastomosed ansa cervicalis-to-left RLN network. Electrical stimulation of the left ansa cervicalis central to the anastomosis and the right RLN elicited clear electromyographic responses in the left (Figure 4A) and right (Figure 4B) vocalis muscles, respectively. Both stimuli elicited weak responses in the contralateral vocalis muscles, likely due to low specificity in laterality from the inappropriate placement of electrodes on the endotracheal tube. These findings demonstrated the functionality of the anastomosed ansa cervicalis-to-left RLN neural network. Additionally, the fiberoptic laryngoscopy performed during surgery revealed contraction of the left vocal fold upon electrical stimulation of the left ansa cervicalis, although stimulation of the left vagus nerve did not evoke a vocalis muscle response.
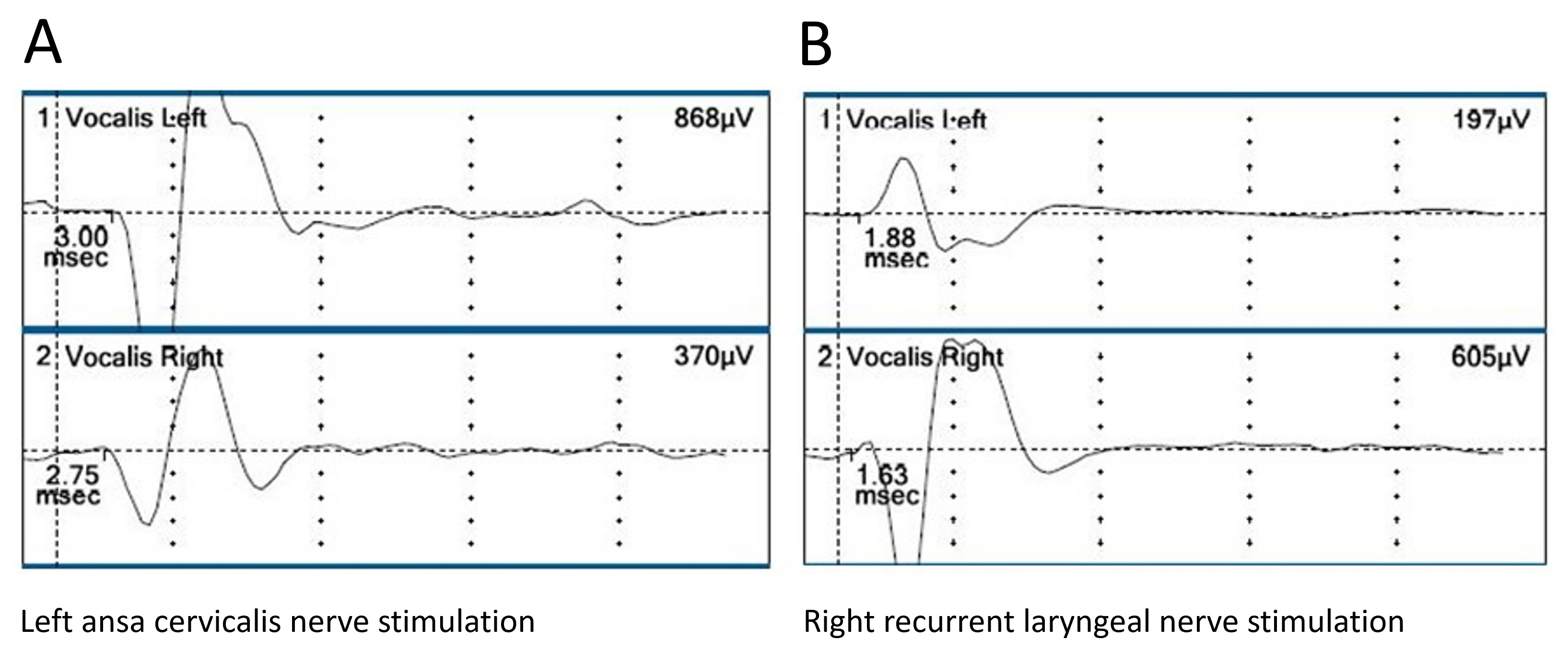
Figure 4. Electromyographic analysis following left ansa cervicalis-to-left RLN anastomosis in Case 2. (A) Pronounced electromyographic response in the left vocalis muscle after left ansa cervicalis nerve stimulation, indicating effective nerve activation post-surgery. (B) Normal response in the right vocalis muscle from right RLN stimulation, confirming intact function. Weak responses on the left side suggest suboptimal electrode placement on the tracheal tube. RLN, recurrent laryngeal nerve.
Case 3: Direct Anastomosis of Severed RLN
This patient was a 32-year-old Japanese woman. One year and 10 months before her first visit to our hospital, she underwent a left lobectomy with paratracheal lymph node dissection and was diagnosed with papillary thyroid cancer. During the surgery, her left RLN was found to be invaded by the tumor, necessitating resection of the nerve, which was subsequently repaired via direct anastomosis. At the time of the initial surgery, the patient’s cancer stage, according to the UICC classification, was Stage I (T4a, N0, M0).
The patient was referred to our hospital for the treatment of recurrent papillary thyroid cancer in the left lateral neck lymph nodes. The ultrasonography revealed swelling in the left cervical lymph nodes, and a fine-needle biopsy confirmed metastatic papillary thyroid cancer. The laryngoscopy at her first visit to our hospital revealed fixation of the left vocal cord in the median position, although it was not atrophic and exhibited good tension during phonation. The patient did not present with hoarseness, and her MPT was 21.4 seconds. CT scans showed no pulmonary metastases.
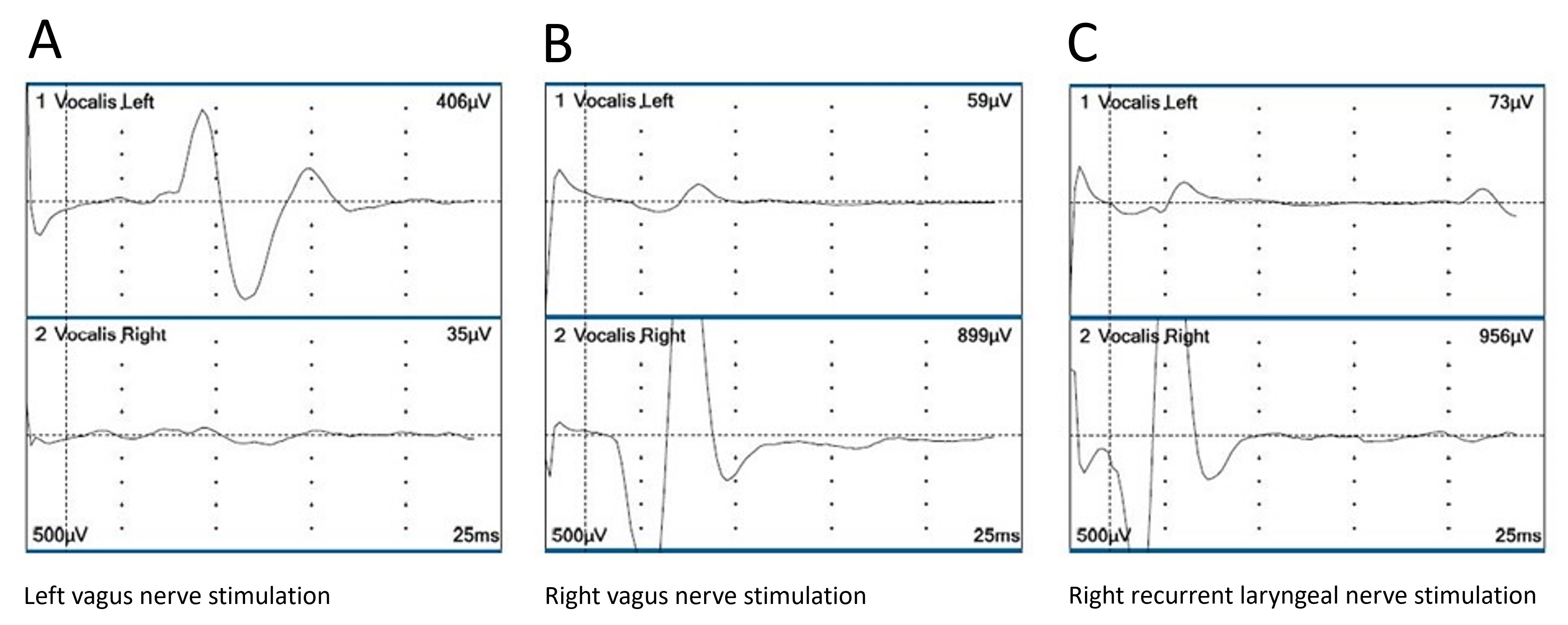
The patient underwent resection of the residual right thyroid lobe and left modified neck dissection. General anesthesia was administered using an endotracheal tube with surface electrodes. The nerve monitoring system described earlier assessed the activity of the RLNs and vagus nerves. During the surgery, both the vagus nerve and the right RLN were stimulated. Electrical stimulation of the left vagus nerve on the side of the direct anastomosis evoked an electromyographic response in the left vocalis muscle, providing clear electrophysiological evidence of reinnervation (Figure 5A). Electrical stimulation of the right vagus nerve (Figure 5B) and right RLN (Figure 5C) also evoked electromyographic responses in the right vocalis muscle, consistent with normal findings. Notably, stimulation of the left vagus nerve exhibited a longer latency between stimulation and response compared to the right vagus nerve. This was attributed to the greater distance between the stimulation site and the vocalis muscle in the former nerve.

Figure 5. Electromyographic outcomes following direct anastomosis of resected left RLN in Case 3. (A) Clear electromyographic response in the left vocalis muscle after left vagus nerve stimulation, indicating successful nerve recovery. (B) Enhanced response in the right vocalis muscle following right vagus nerve stimulation, reflecting optimal neural function. (C) Exceptionally clear response in the right vocalis muscle from right RLN stimulation, affirming robust nerve functionality. RLN, recurrent laryngeal nerve.
Need for Direct Reinnervation Evidence
Numerous reports have documented the postoperative recovery of phonation following RLN repair [1,2]. Typically, when the severed RLN is repaired, the ipsilateral vocal cord remains fixed in the median position and does not regain normal movement. However, the vocal fold eventually recovers from atrophy and restores tension during phonation, ultimately leading to the patient’s voice recovery [1]. This recovery is evidenced by the improvement in MPT following RLN repair [2].
The recovery process has been linked to misdirected regeneration among the adductor and abductor fibers within the RLN, as observed in electromyographic analyses of animal experiments [9]. In the RLN, the number of adductor nerve fibers is three times that of the abductor nerve fibers, and in the larynx, the adductor muscles are significantly stronger than the abductor muscles. This imbalance results in the reinnervated vocal fold not restoring normal movement and remaining in the median position during inspiration and phonation [9], complicating the assessment of reinnervation.
Traditional diagnostic approaches, such as phonatory examinations, laryngoscopic examinations, stroboscopic analyses, and vocal function questionnaires, typically provide only suggestive evidence of reinnervation and are often inconclusive [4–7]. Therefore, electrophysiological evaluations are essential to furnish direct and convincing evidence of reinnervation. Electrical stimulation of the nerve central to the repair site provides conclusive evidence of reinnervation of the ipsilateral vocalis muscle—a technique that, to our knowledge, has not been previously reported in humans.
Electrophysiological Evidence for RLN Repair
In this study, we neurophysiologically assessed three patients using intraoperative nerve monitoring techniques. These patients had regained good phonation after RLN repair and subsequently required reoperation due to the recurrence of papillary thyroid carcinoma. Of the three patients, two underwent ansa cervicalis-to-RLN anastomosis and one underwent direct anastomosis. Clear electromyographic responses of the vocalis muscle on the repair side were recorded when the nerve central to the anastomosis was electrically stimulated. The amplitudes (406–868 μV) obtained from the stimulation were sufficiently large compared to the contralateral side, with clear waveforms and defined latencies.
Wang et al. previously inserted needle electrodes percutaneously into the laryngeal muscles of patients who underwent PLN repair and obtained electromyographic data during phonation and respiration [10]. However, this method does not conclusively demonstrate the functionality of the nerve-to-nerve anastomosis neural network. To our knowledge, this is the first report to confirm reinnervation by measuring the electromyographic response of the vocalis muscles upon electrical stimulation of the nerve central to the anastomosis. In addition to the electrophysiological evidence of reinnervation, simultaneous laryngeal fiberscopy confirmed the contraction of the vocal fold on the RLN repair side, providing another direct indication of reinnervation.
The extent of phonatory dysfunction in patients who have had resection or injury of unilateral RLN can vary, and some patients without RLN repair may show spontaneous recovery of phonatory function. One possible explanation for this phenomenon is the innervation of the vocalis muscles from the superior laryngeal nerve or contralateral RLN via intrinsic intralaryngeal anastomosis. Another possibility is spontaneous reinnervation across the injury site without nerve anastomosis [11,12]. However, the former is difficult to assess. The latter—spontaneous reinnervation across the RLN injury site—should be evaluated in patients with RLN injuries who have demonstrated phonatory recovery, as described in this report. Specifically, stimulation of the RLN central to the injury site and the ipsilateral vagus nerve should yield an electromyographic response in the vocalis muscle.
Comparative Techniques for RLN Repair
To repair RLNs that have been severed or partially resected due to cancer invasion or accidents, several techniques have been employed: direct anastomosis of the cut ends, free nerve grafting to bridge the defect, ansa cervicalis-to-RLN anastomosis, and, in exceptional cases, vagus-to-RLN anastomosis. Each method presents distinct limitations and advantages. However, the recovery of phonation, as assessed by MPT or the phonation efficiency index, did not significantly differ among these methods, according to our evaluations and previous studies [2,13].
Study Limitations
A primary limitation of this study is the small sample size, with only three cases. However, opportunities to assess reinnervation in patients who underwent RLN repair are limited. From 1998 to 2023 at Kuma Hospital, RLN repair was performed on 592 patients, with 449 cases previously reported [13]. Among these patients, the three cases presented here involved loco-regional recurrence necessitating neck surgery, providing a unique opportunity for electrophysiological study. Thus, these cases are particularly significant. While it is theoretically possible to insert electrode needles directly into the larynx, this approach is not beneficial for patients and may result in adverse events, such as infection, vocal cord damage, bleeding, and additional postoperative complications.
This study presents the first electrophysiological evidence of vocalis muscle reinnervation following RLN repair in humans. Through intraoperative nerve monitoring, we demonstrated clear electromyographic responses, confirming successful reinnervation. These findings underscore the critical role of electrophysiological assessments in validating nerve repair and emphasize the importance of precise surgical techniques and rigorous postoperative monitoring in restoring vocal cord function. This pioneering evidence not only sets a new standard for evaluating RLN repair success but also paves the way for future research and innovation in surgical and diagnostic practices, offering renewed hope and improved outcomes for patients with vocal cord paralysis.
Received date: March 12, 2024
Accepted date: June 12, 2024
Published date: July 03, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)’ autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
Total thyroidectomy and adjuvant RIT followed by a suppressive dose of levothyroxine are the established therapeutic procedures of choice for DTC. The treatment of DTC has changed from a one size fits all standard to a more individualized approach. The use of less complete surgery as well as decision to use RIT and the dose administered are to be considered carefully in the treatment of DTC. Surveillance for very low risk DTC is an acceptable option. The aim to lower morbidity, lower the cost of treatment and improve patient quality of life is attainable using these principles.
This article is crucial as it offers robust evidence of vocalis muscle reinnervation following recurrent laryngeal nerve (RLN) repair, demonstrating its efficacy in restoring phonatory function postoperatively. The study documents clear electromyographic responses in patients, providing key insights for refining treatment strategies and improving outcomes for individuals with vocal cord paralysis. The article is a candidate for publication, subject to a few minor revisions.
The manuscript underscores the importance of intraoperative neuromonitoring in thyroid surgeries but requires minor revisions due to significant deficiencies. Insufficient clinical details, particularly regarding cancer staging, impede precise outcome interpretation and future research criteria. Furthermore, unclear electromyographic (EMG) amplitude definitions compromise study validity and reproducibility. Establishing a clear EMG criterion, such as utilizing contralateral responses as a baseline, is crucial for reliable conclusions regarding nerve functionality and reinnervation. Addressing these deficiencies through detailed clinical context, clear EMG criteria, and a robust discussion will markedly enhance the manuscript's quality and suitability for publication.
This article significantly enhances our understanding of intraoperative nerve monitoring in recurrent laryngeal nerve repair, providing crucial evidence of its effectiveness in improving vocal function recovery after surgery. As a pioneering work, it highlights the importance of intraoperative nerve monitoring, a well-established technique, and offers fresh insights into its advantages over traditional methods. The authors conduct a comprehensive examination of surgical outcomes, employing a robust and detailed methodology, which underscores the significant implications for clinical practice and future research in nerve repair. This article demonstrates a high level of expertise in its execution and merits publication, contingent upon addressing the following specific issue beforehand.
Incorporating a table into a medical case series enhances clarity by organizing complex data for direct comparison across cases, aiding understanding of treatment effectiveness variations. This visual tool streamlines comparisons, boosting comprehension of critical differences and parallels in research findings. As an example, I present a table comparing clinical attributes, therapeutic strategies, and patient outcomes across three cases, elucidating the efficacy and distinctions among recurrent laryngeal nerve repair techniques.

ResponseThank you for your suggestion. We have incorporated a table into the manuscript based on your recommendation. This table compares clinical attributes, therapeutic strategies, and patient outcomes across the three cases, elucidating the efficacy and distinctions among recurrent laryngeal nerve repair techniques. This addition enhances the clarity of our data presentation, enabling a more straightforward comparison and better understanding of the variations in treatment effectiveness.
Masuoka H, Miyauchi A, Kawano S. New insights into reinnervation of the vocalis muscles after recurrent laryngeal nerve repair: Electrophysiological evidence. Arch Otorhinolaryngol Head Neck Surg 2024;8(1):5. https://doi.org/10.24983/scitemed.aohns.2024.00186