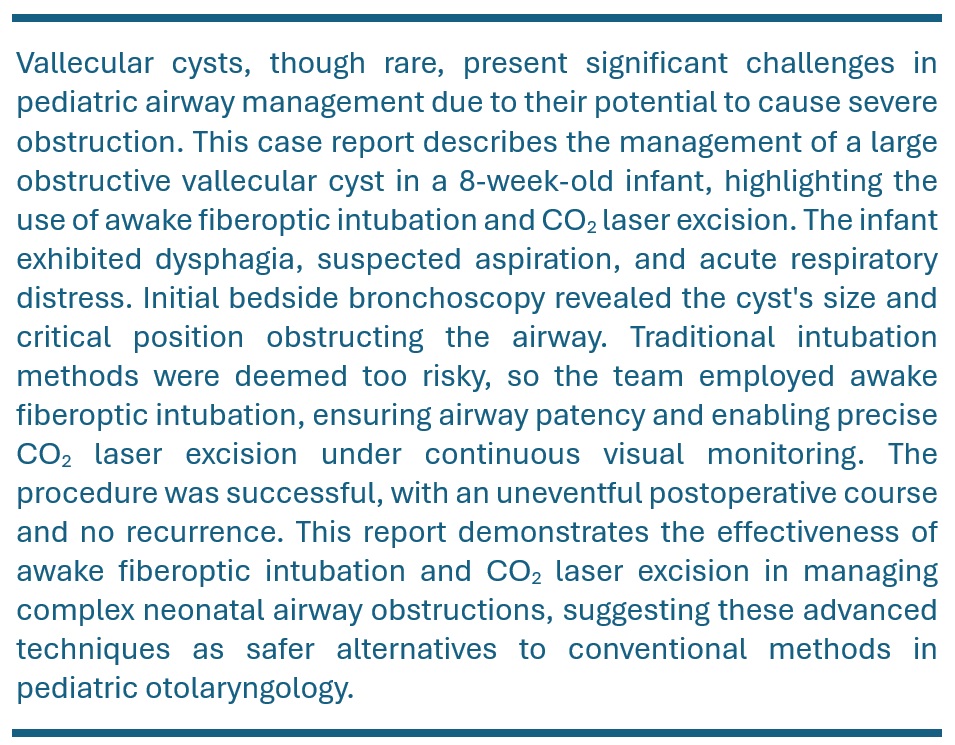
Vallecular cysts present significant challenges in pediatric airway management due to their potential to cause severe obstruction and respiratory distress. This case report highlights the successful management of a large vallecular cyst in an eight-week-old infant through awake fiberoptic intubation and transoral CO2 laser microsurgery for near-total excision. The infant presented with dysphagia, stridor, and signs of impending respiratory failure. Bedside flexible laryngoscopy confirmed the obstructive characteristics of the cyst. Due to the high risk associated with traditional intubation techniques in such cases, the medical team opted for awake fiberoptic intubation, which ensured continuous airway control throughout the procedure. The transoral CO2 laser excision effectively removed the cyst with minimal trauma, resulting in a smooth postoperative recovery. No recurrence was observed at the 6-month follow-up. This case underscores the dual efficacy of awake fiberoptic intubation and CO2 laser microsurgery in managing complex neonatal airway obstructions, advocating for their broader use in pediatric otolaryngology.
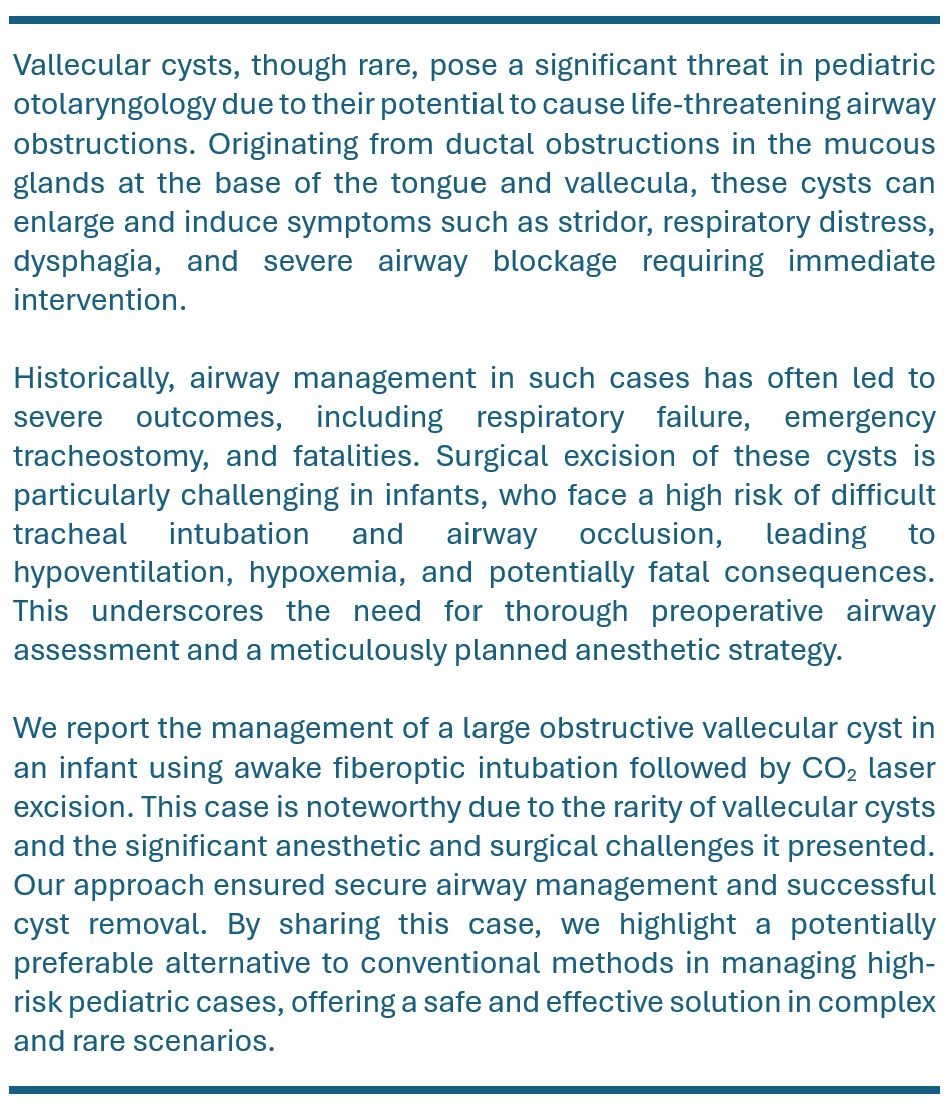
Vallecular cysts present significant clinical challenges in infants due to their potential to cause life-threatening airway obstructions [1]. These lesions originate from ductal obstructions in the mucous glands at the base of the tongue and vallecula [2]. While small vallecular cysts may be asymptomatic, larger ones can induce symptoms such as dysphagia, alongside life-threatening complications including acute airway obstruction, hypoxia, and even death [3]. Such severe manifestations frequently necessitate immediate surgical intervention.
Historically, the positioning of vallecular cysts has occasionally resulted in severe complications during airway management, such as respiratory failure, the need for emergency tracheostomy, and even fatalities [4–6]. The surgical removal of these cysts introduces significant challenges, particularly the high risk of airway occlusion directly related to the complexities of intubation. These intubation challenges can cause hypoventilation and hypoxemia, potentially leading to fatal outcomes [5]. Consequently, conducting a comprehensive preoperative airway assessment and meticulously planning the anesthetic strategy are imperative to ensure patient safety and effective management.
This report details the management of a significant obstructive vallecular cyst in an infant, utilizing awake fiberoptic intubation and transoral CO2 laser microsurgery for near-total excision. The rarity of vallecular cysts and the substantial challenges they pose in both anesthesia and surgical management make this case noteworthy. Our approach effectively managed the airway and facilitated the successful removal of the cyst. By documenting this procedure, we offer an alternative to conventional airway control techniques, suggesting a refined method for managing high-risk pediatric cases involving complex and rare conditions.
Initial Presentation and Diagnosis
An eight-week-old female infant exhibited several signs of respiratory distress, including dysphagia, stridor, chest retractions, and increased respiratory effort. A clinical suspicion of aspiration was also noted. A bedside flexible laryngoscopy revealed a large, one-centimeter obstructive vallecular cyst located between the base of the tongue and the epiglottis, accompanied by mild laryngomalacia. The infant received 0.25 liters of oxygen via nasal cannula to prevent desaturation. Given the severity of the respiratory and feeding challenges, the clinical team promptly initiated definitive management strategies.
Surgical Management
Twenty-four hours post-initial evaluation, the patient was moved to the operating room for complex airway management. Conventional methods, specifically standard mask induction and direct laryngoscopy followed by endotracheal intubation, were deliberately avoided due to their potential to exacerbate airway obstruction. Instead, awake fiberoptic intubation was employed as a safer alternative. During this procedure, while the pediatric anesthesia team closely monitored the patient, the pediatric otolaryngology team utilized the brief pauses in the infant’s cries to enhance visualization of the airway. These moments allowed for vocal cord abduction during inhalations, improving visibility and aiding the intubation process. A 3.0 endotracheal tube (ETT) was loaded onto a 2.5 mm flexible laryngoscope. The laryngoscope was then used to guide the ETT accurately into place (Figure 1A). The correct placement of the ETT was confirmed through flexible tracheobronchoscopy.
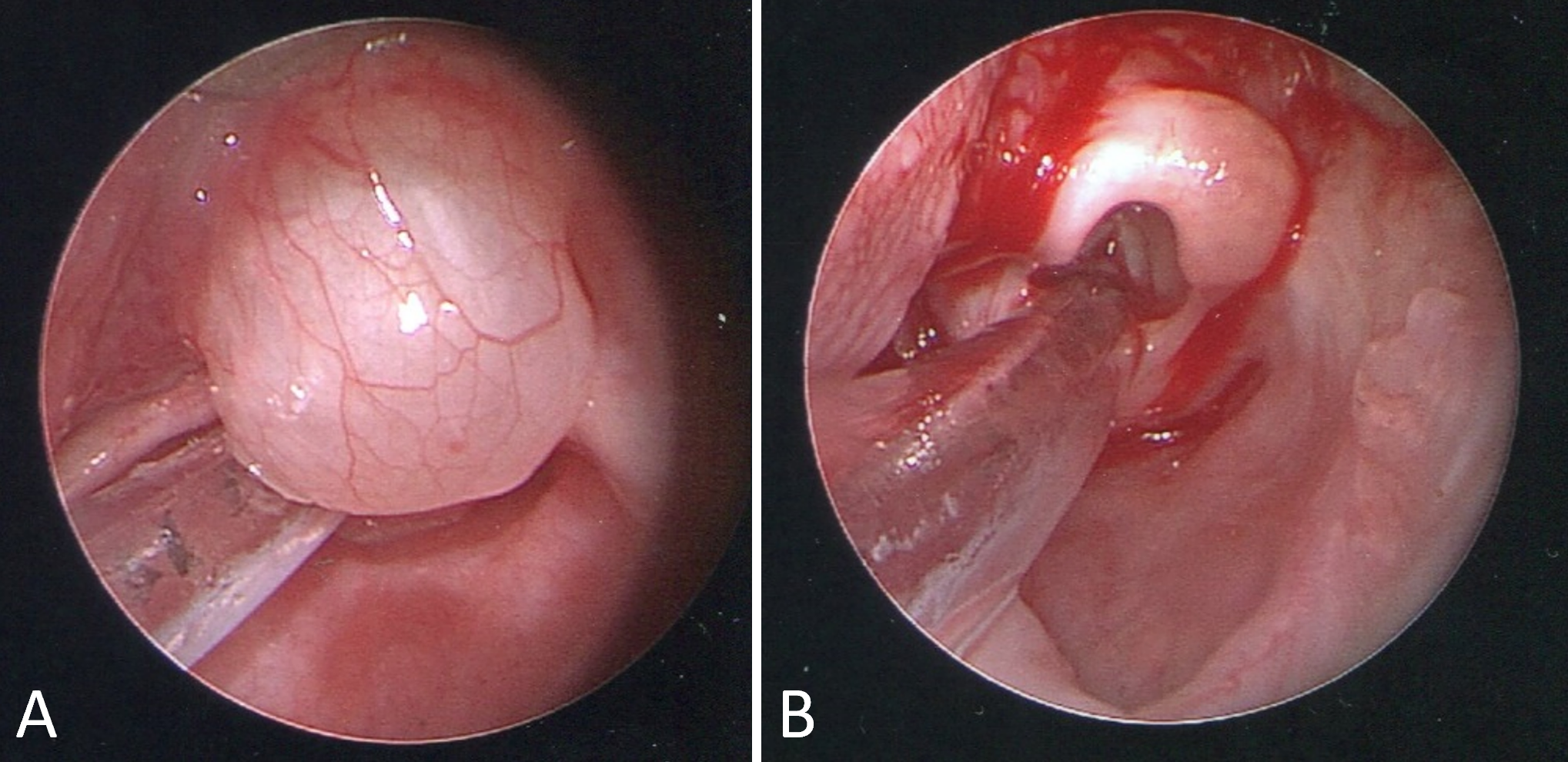
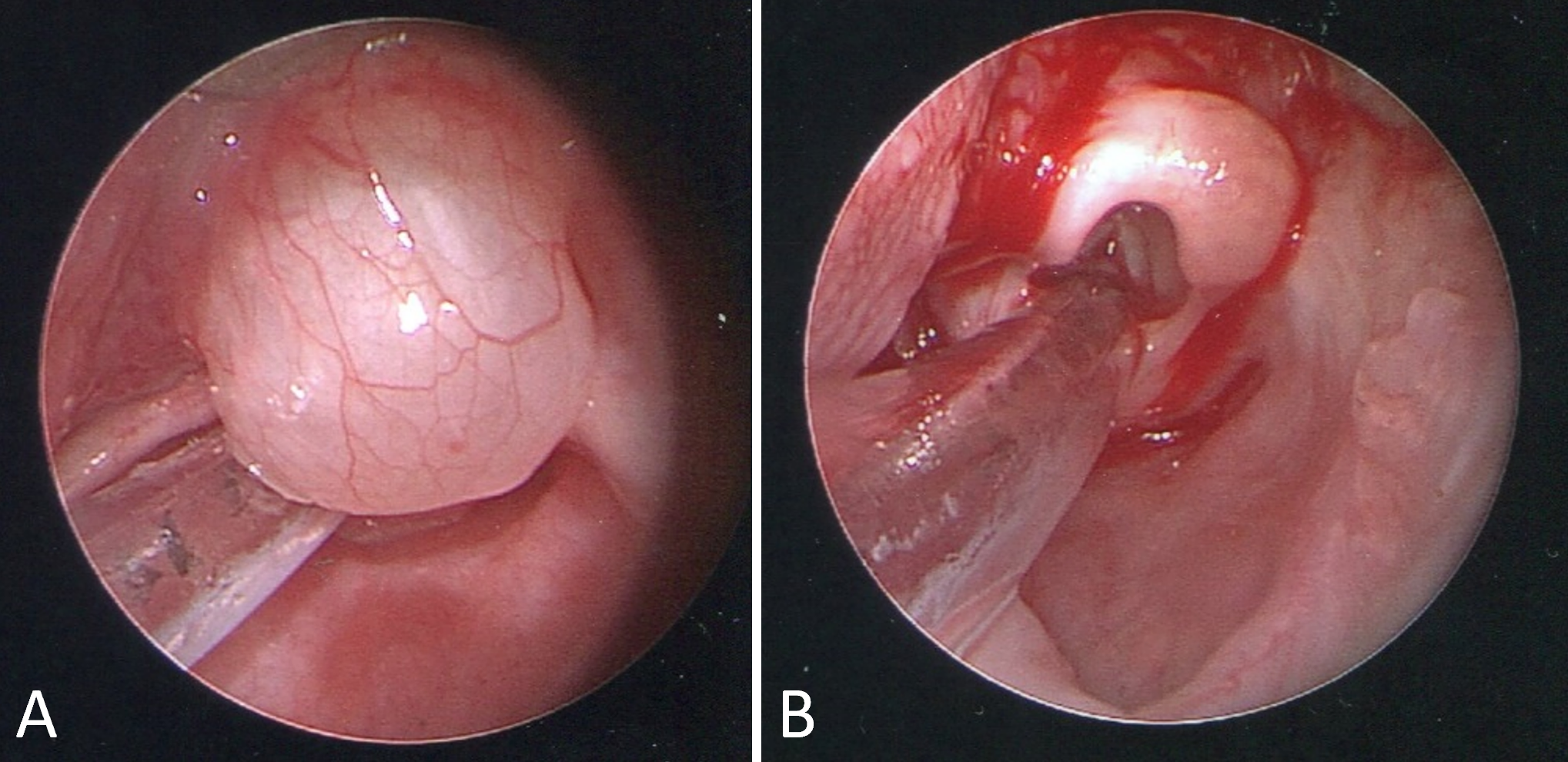
Figure 1. (A) Preoperative view of a large vallecular cyst located between the base of the tongue and the epiglottis in an eight-week-old infant. The translucent cyst, showing visible vascularization, is adjacent to the endotracheal tube placed via awake fiberoptic intubation. (B) Postoperative view following transoral CO2 laser excision of the cyst, illustrating a clear surgical field with minimal bleeding. This comparison highlights the effectiveness of CO2 laser microsurgery in managing complex airway obstructions in infants.
Following airway stabilization and the administration of general anesthesia, the surgical team employed a Parsons laryngoscope to improve visibility and surgical access to the cyst. The procedure began with the use of micro-cup forceps to securely grasp the cyst. Then, a CO2 laser, set at 1 watt, was used to remove about 95% of the cyst, effectively minimizing bleeding and enhancing safety. The residual, exceedingly thin cyst wall was vaporized at the tongue’s base, a process termed “cyst wall vaporization.” This action designated the surgery as a near-total excision (Figure 1B). Post-operatively, to reduce swelling risks, the patient remained intubated with a 3.0 ETT and was closely monitored in the pediatric intensive care unit (PICU).
Effective Postoperative Recovery
The patient received intravenous dexamethasone at 0.5 mg/kg twice daily, aiding in the management of postoperative inflammation and contributing to a smooth extubation process three days after surgery. Continuous monitoring in the PICU ensured close observation during the critical postoperative phase, supporting the patient’s stabilization before transfer to the general ward. The patient underwent specialized neonatal interventions to manage respiratory and feeding difficulties, demonstrating marked improvements within two days.
Following surgery, a follow-up flexible laryngoscopy conducted ten days later confirmed the absence of cyst recurrence, inflammation, or significant airway obstruction. Although mild laryngomalacia and arytenoid collapse were observed, these conditions did not necessitate further surgical intervention as they were not significantly impairing the infant’s breathing or feeding abilities. The mild nature of these findings, often expected to improve as the child grows, led to a conservative management approach. Consequently, the infant demonstrated improved oral feeding capabilities, which facilitated the removal of the nasogastric tube and ultimately enabled discharge from the hospital. The child was able to breathe comfortably and achieve full oral feeding under parental care at home, illustrating successful postoperative recovery and management without the need for additional surgical procedures.
Outpatient Follow-up
During outpatient follow-up visits and flexible laryngoscopy assessments at 2, 3, and 6 months post-procedure, the patient demonstrated normal breathing and feeding capabilities. These evaluations confirmed the complete resolution of airway obstruction without any recurrence of the cyst. Additionally, the previously noted laryngomalacia had resolved. These results underscore the effectiveness of the surgical intervention and affirm the successful postoperative recovery.
This report details the successful management of a significant obstructive vallecular cyst in an infant, achieved through awake fiberoptic intubation and transoral CO2 laser microsurgery for near-total excision. The absence of cyst recurrence over a six-month postoperative period highlights the effectiveness of the applied surgical and anesthetic techniques. However, the reproducibility of such outcomes may vary based on the cyst’s specific characteristics, including size and location, and the unique clinical circumstances of each case. The success of this approach critically depends on the specialized expertise of the surgical and anesthetic teams, especially those proficient in pediatric anesthesia and otolaryngology. Additionally, access to specialized equipment and the support of a well-equipped PICU are vital for managing complex airway obstructions effectively. This case exemplifies the importance of tailoring anesthetic and surgical strategies to enhance patient safety and secure favorable outcomes, serving as a crucial reference for similar pediatric airway challenges.
Airway Impacts from Vallecular Cysts
Vallecular cysts, classified primarily as retention cysts, arise due to ductal obstructions in the mucous or minor salivary glands at the base of the tongue and vallecula. Though relatively rare, they account for 10.5% to 20.1% of all laryngeal cysts [5,7]. The incidence of vallecular cysts is estimated to range between 3.49 and 5.3 cases per 100,000 live births [8]. These cysts are typically present at birth, with the median age of diagnosis ranging from 3 to 40 days. However, they may also manifest or be identified later in older children and adults [2,7,9].
Vallecular cysts are often associated with clinical signs such as stridor, feeding difficulties, failure to thrive, dysphonia, and respiratory distress [3,5,10]. Although benign, the growth of these cysts can lead to substantial airway obstruction. This obstruction can result in acute, life-threatening scenarios that frequently require emergency intervention [3–6]. Numerous reports in the literature document cases with fatal or near-fatal outcomes related to these cysts [5,11]. A 10-year study involving 238 patients identified the lingual surface of the epiglottis as the most common site of occurrence [2]. This finding was corroborated in our case, where flexible laryngoscopy revealed the cyst at this specific anatomical location, emphasizing the clinical relevance of this site for effective airway management.
Diagnostic Strategies for Vallecular Cysts
The diagnosis of vallecular cysts can be supported by various imaging modalities and examination techniques, including flexible laryngoscopy, direct laryngoscopy, lateral radiography, ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI). Each diagnostic tool offers unique benefits and drawbacks [5].
Flexible laryngoscopy is regarded as the optimal technique for diagnosing vallecular masses. It is rapid, minimally invasive, and effective for initial assessments, although it may not differentiate among similar conditions. Direct laryngoscopy offers a more comprehensive view under cardiopulmonary monitoring, proving invaluable for in-depth evaluations despite its significant invasiveness [5].
Lateral radiography, though convenient, frequently lacks the necessary diagnostic precision. Ultrasound is a non-invasive and readily accessible technique that excels in distinguishing between solid and cystic masses and confirming normal thyroid anatomy. It serves as an excellent initial screening tool for vallecular cyst evaluation, especially beneficial for pediatricians inexperienced with flexible laryngoscopy. However, ultrasound may not adequately visualize deeper structures of the throat, which limits its diagnostic utility for vallecular cysts. CT scans, while valuable for specific diagnoses, expose infants to radiation. These procedures often require sedation to minimize movement, introducing additional risks. MRI delivers the most precise diagnostic data; however, its use in infants is complicated by the need for sedation. This requirement, along with high costs and potential motion artifacts, limits its practicality [5].
The varying benefits and limitations of each diagnostic tool underscore the need for personalized diagnostic strategies in the evaluation of vallecular cysts. Individualized approaches are essential due to the wide variation in condition presentation, cyst size, and symptom severity across patients. By tailoring diagnostic methods to the specific needs and circumstances of each case, clinicians can ensure the use of the most effective and minimally invasive techniques, ultimately leading to accurate diagnoses and improved patient outcomes.
In this case, flexible laryngoscopy was the primary tool for preoperative assessment, selected due to critical considerations. Facing acute respiratory distress in the infant, this method provided rapid and precise diagnosis while minimizing the risks associated with more invasive imaging techniques like MRI or CT, which typically require sedation and, in the case of CT, expose patients to radiation. The endoscopic examination effectively delineated a translucent, vascularized cyst, thus providing clear diagnostic insight without the need for further imaging. Additionally, direct laryngoscopy performed under general anesthesia offered a detailed anatomical evaluation of the lesion. This technique maintained a delicate balance between diagnostic thoroughness and patient safety, circumventing more complex and risky imaging approaches.
Critical Airway Management
Effective visualization is crucial for successful ETT placement in airway management [12]. However, achieving clear visibility in infants with constricted airways poses significant challenges, especially when a large vallecular cyst substantially obstructs the airway.
The initial challenge centered on the decision to perform cyst aspiration. In infants, this procedure presents unique difficulties due to the delicate nature of airway structures and the urgency required in securing the airway. Additionally, maneuvering surgical instruments within the constricted infant airways poses significant challenges, further complicating the process. Traditional intubation under anesthesia can lead to induction risks, potentially resulting in critical outcomes such as hypoxia or death. Conversely, awake intubation offers a viable alternative that mitigates these induction risks by maintaining spontaneous respiration, though it still carries the potential risk of pulmonary aspiration of cyst contents during the procedure [3,5,6,9,13].
The subsequent challenge involved the strategic selection of awake intubation. This technique, which employs direct laryngoscopy or fiberoptic bronchoscopy without prior sedation, is typically reserved for specific clinical scenarios within anesthetic and airway management practices. Thus, a thorough review of empirical evidence regarding its application in children with vallecular cysts is crucial. In a cohort study of 156 children diagnosed with vallecular cysts, ranging in age from 1 day to 11 years and with a median age of 12.1 months, 6.4% (10 patients) experienced complications during conventional intubation techniques [14]. The noted complications included critically reduced blood oxygen saturation below 85%, failures in standard intubation practices, emergency cyst punctures, and instances of respiratory and cardiac arrest. This 6.4% incidence of potentially catastrophic complications underscores the urgent need to reassess the safety and efficacy of conventional intubation methods, particularly for children exhibiting preoperative signs of imminent respiratory failure—such as stridor, chest retractions, increased respiratory effort, and perioral cyanosis—similar to those observed in our patient.
Given the associated risks, our team opted for awake fiberoptic intubation as the most prudent method to secure the airway [12]. This technique provided excellent visualization and stabilization of the vocal cords and laryngeal inlet. Positioning the infant upright during the procedure enhanced laryngeal visibility, thus improving the precision of the fiberoptic intubation. The decision to forego cyst aspiration was intentional, underscoring our commitment to reducing risks and ensuring patient safety.
Ethical Considerations in Awake Infant Intubation
Performing awake fiberoptic intubation in infants raises ethical concerns due to the perceived invasiveness and potential discomfort of the technique. However, when confronting life-threatening conditions such as severe airway obstruction, the primary duty of the medical team is to ensure patient safety. In the described case, awake intubation was selected as a safer alternative to conventional methods that presented greater risks. While the procedure may cause discomfort, the administration of local anesthesia can significantly reduce pain. It is crucial to balance the risks and benefits and to ensure that families are thoroughly informed about all treatment options and associated risks prior to obtaining consent. Ethically, decisions must prioritize the patient’s safety and well-being above all else.
Optimal Techniques for Vallecular Cyst Surgery
Various surgical techniques are utilized in managing vallecular cysts, including aspiration, marsupialization, and complete excision [3,4]. Aspiration, with a recurrence rate reported as high as 50%, offers limited efficacy [5]. Both complete excision and marsupialization demonstrate significantly lower recurrence rates [15,16]. A literature review of 52 reported cases from 1988 to 2011 revealed no recurrences in 10 patients following extirpation, which includes resection and excision, while a single recurrence was observed among 39 patients undergoing marsupialization [5]. This data suggests a marginally higher recurrence risk with marsupialization compared to complete excision. Nonetheless, given that complete excision risks damaging healthy tongue tissue [17], near-total excision emerges as a balanced option, effectively reducing recurrence while minimizing tissue harm.
In the management of vallecular cysts, surgical instruments such as cold steel surgery, electrocautery, coblation, microdebriders, and CO2 lasers play pivotal roles. Cold steel surgery, though effective, often increases bleeding and reduces visibility, complicating airway management. Electrocautery is notable for its hemostatic benefits but risks thermal injury to surrounding tissues. Coblation, which causes less thermal damage, requires larger equipment that may be impractical for small airways. Microdebriders, though useful for specific surgical procedures, may be less ideal than CO2 lasers due to their lower precision and higher risk of inducing bleeding. The CO2 laser stands out for its precise and hemostatic properties, facilitating remote access to surgical sites and minimizing trauma, thereby expediting healing.
In this instance, we opted for transoral CO2 laser microsurgery for the near-total excision of the vallecular cyst. This technique was selected due to its precision, low recurrence rate, minimal tissue trauma, and reduced bleeding, enhancing recovery efficiency in pediatric airway management. However, it is vital to recognize that no single method is universally optimal. The choice of technique should consider several factors, such as the surgeon’s expertise, patient’s specific anatomy and condition, and the availability of specialized equipment. Customizing the surgical approach to these variables is essential to optimize outcomes.
Vallecular cysts pose significant challenges in pediatric airway management due to their potential to cause substantial airway obstruction and life-threatening complications. In the discussed case, the integrated use of awake fiberoptic intubation and transoral CO2 laser microsurgery for near-total excision was highly effective. This strategy was skillfully applied to manage a large vallecular cyst in an eight-week-old infant, yielding positive outcomes. These results affirm the safety and efficacy of these methods for treating prominent vallecular cysts in pediatric otolaryngology.
Received date: April 19, 2024
Accepted date: August 12, 2024
Published date: September 09, 2024
LL and ND prepared the initial draft of the manuscript. DLW, LL, and ND then critically revised the manuscript. All authors have reviewed and approved the final version for publication and agree to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
This study rigorously adheres to the ethical guidelines established by the 1964 Declaration of Helsinki and its subsequent amendments, as well as other applicable ethical standards. These guidelines are integral to the governance of human subject research, ensuring that all aspects of the study are conducted with ethical rigor and responsibility. The research team has diligently ensured compliance with all relevant ethical standards and guidelines, with the aim of protecting participant well-being and privacy. The authors confirm that they have secured all necessary patient consent forms. These forms document that the patient and her guardians have provided their consent for the publication of her images and other clinical information in the journal. It is explicitly understood by all parties involved that personal identifiers, such as names and initials, will be excluded from publication. Efforts will be made to protect the identities of the participants, although the authors acknowledge that complete anonymity cannot be fully guaranteed.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)’ autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Otolaryngologists and gastroenterologists seem to differ in their definitions and management of laryngopharyngeal reflux (LPR). In this review article, the author suggests a multidisciplinary approach to LPR diagnosis. Based on the latest findings, the author proposes an algorithm to facilitate the assessment and management of LPR.
ResponseWe appreciate the reviewer’s suggestions and have incorporated them into the abstract.
Li L, Davidson N, Parnass A, Walner D. Airway obstruction management in an infant with a large vallecular cyst: Awake fiberoptic intubation and transoral CO2 laser microsurgery for effective resection. Arch Otorhinolaryngol Head Neck Surg 2024;8(2):1. https://doi.org/10.24983/scitemed.aohns.2024.00190