Lesions within the parotid gland can significantly displace the facial nerve, leading to substantial anatomical deviations that undermine the reliability of traditional intraoperative landmarks. These deviations necessitate increased vigilance to prevent iatrogenic injury to the facial nerve during surgery. We describe a challenging case involving a 75-year-old Chinese woman with a parotid lesion that caused an undetected preoperative displacement of the facial nerve. This unexpected deviation from the nerve's typical pathway required intraoperative adaptability. Employing a retrograde dissection technique, as opposed to the conventional anterograde approach, was crucial to preserve the integrity of the facial nerve. Despite the availability of advanced imaging techniques, anatomical anomalies can still significantly complicate surgical procedures. This highlights the need for tailor-made surgical strategies to ensure patient safety and successful outcomes.
Preserving the facial nerve during parotidectomy is of paramount importance. However, the size, position, and involvement of the primary parotid lesion can complicate this endeavor. It is well-documented that both superficial and deep lobe parotid lesions can alter the facial nerve's course [1–3], making standard anatomical landmarks unreliable for identifying the nerve. These deviations from typical facial nerve anatomy add to the surgery's complexity and may lead to an increased risk of postoperative facial paresis.
In this paper, we describe a case that highlights the challenges of aberrant facial nerve anatomy due to a parotid lesion. We also discuss the benefits of employing a retrograde dissection technique rather than the conventional anterograde approach. This method allowed us to preserve the integrity of the facial nerve while effectively managing the parotid lesion.
A 75-year-old Chinese female presented to our Ear, Nose, and Throat (ENT) clinic with a right neck mass that had persisted for three weeks. The initial computed tomography (CT) scan of the neck displayed a 2.7 × 3.1 × 2.9 cm mass in the superficial right parotid region. A fine needle aspiration (FNA) biopsy suggested a pleomorphic adenoma. The patient defaulted on the follow-up and returned three years later, reporting an increase in the size of her neck mass. Upon physical examination, a 6 cm firm mass was palpable over the right angle of the jaw. No cervical lymphadenopathy was detected, and facial nerve function was intact. Nasoendoscopy findings were within normal limits. A repeat CT scan demonstrated marked growth of the mass, now centered in the superficial parotid gland, with patchy enhancement (Figure 1A), raising suspicions of a low-grade parotid malignancy. There was no radiological evidence of cervical lymph node involvement. The patient was scheduled for surgery to obtain a definitive histological diagnosis.
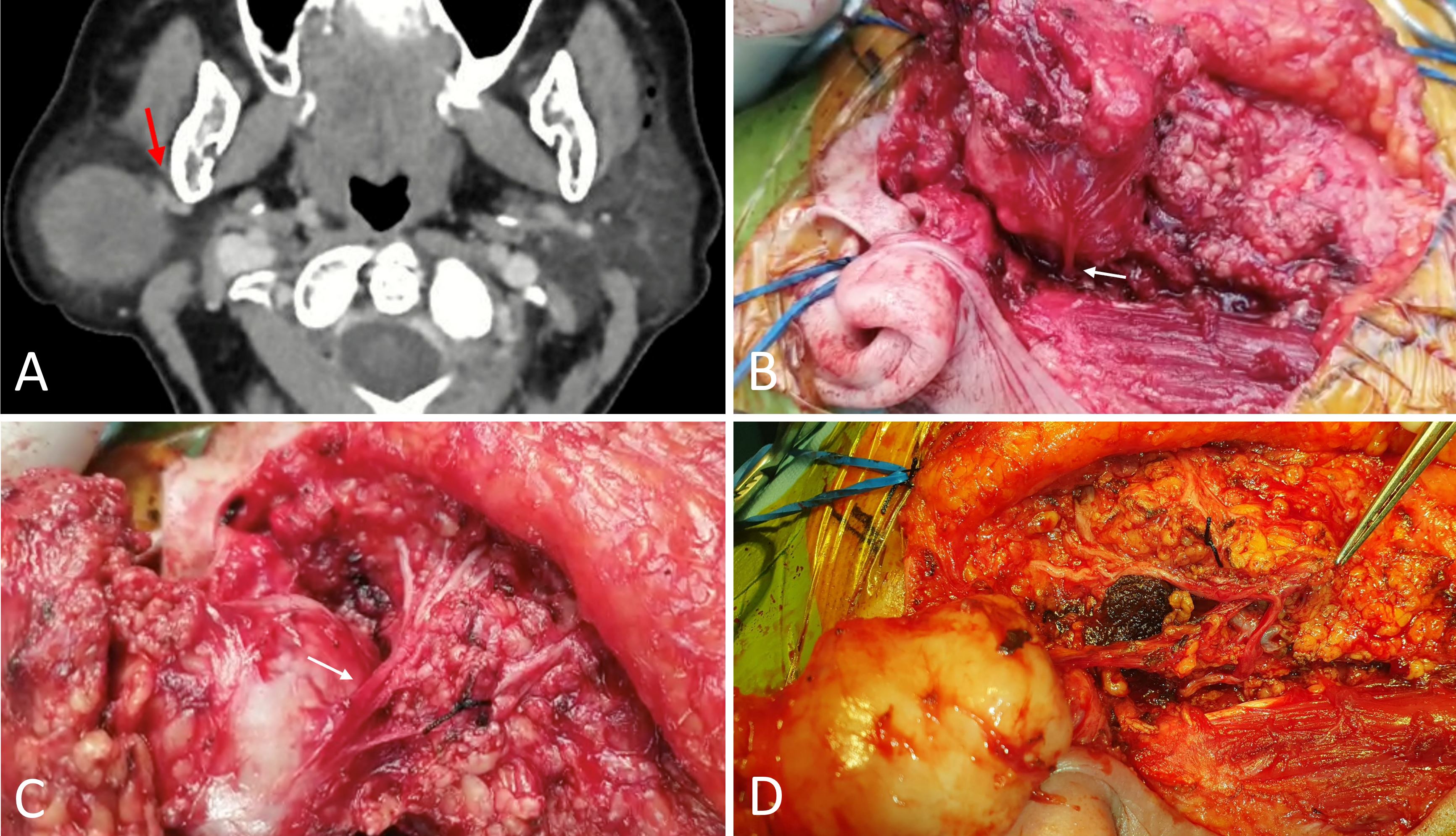
Figure 1. (A) An axial section of the preoperative CT scan illustrates the proximity of the lesion to the retromandibular vein, indicated by the red arrow. (B) Depiction of the main trunk, highlighted by the white arrow, curving posteriorly towards the tragus. (C) The white arrow shows the branches of the facial nerve extending anteriorly across the tumor's surface. (D) The facial nerve and its branches following the excision of the tumor.
A superficial parotidectomy was performed with dual-channel facial nerve monitoring (Medtronic NIM-Response 3.0) in accordance with our institution’s standard practice. Intraoperatively, we encountered a large 6 cm tumor located in the anterior portion of the right superficial parotid lobe, extending towards the deep lobe. Initial anterograde dissection attempts, employing standard surgical landmarks (the tragal pointer, the posterior belly of the digastric, and the tympanomastoid suture), were unsuccessful in identifying the pes anserinus, indicating anomalous facial nerve anatomy. Consequently, a decision was made early on to shift to retrograde dissection to circumvent iatrogenic injury to the main nerve trunk.
The pes anserinus was eventually located using the retrograde approach. Following this, the main nerve trunk was discovered to loop posteriorly towards the tragus (Figure 1B), then run anteriorly across the tumor surface, bifurcating into superior and inferior divisions (Figure 1C). All facial nerve branches were meticulously identified and conserved after en bloc tumor excision (Figure 1D).
Given the preoperative FNA diagnosis of pleomorphic adenoma and the imaging features suggestive of a possible low-grade parotid malignancy without nodal involvement, no intraoperative frozen section was performed. The surgical strategy was limited to the parotidectomy alone. At the conclusion of the operation, all branches of the right facial nerve were responsive to stimulation at 0.8 mA.
The final histological analysis confirmed the presence of a pleomorphic adenoma. In the immediate postoperative phase, the patient exhibited right-sided forehead, eye, and mouth movement weakness, graded as House-Brackmann score 4. By the 6-month postoperative follow-up, her condition had improved to a House-Brackmann score of 2.
The identification of the facial nerve is crucial in parotid surgery, requiring surgeons to be vigilant of atypical nerve positions, especially when neoplasms may cause displacement. In a certain case series, the incidence of facial nerve displacement associated with superficial lobe tumors was noted to be as high as 38.3% [2]. Diverse displacement patterns have been documented. For instance, pediatric patients with deep lobe parotid tumors have been reported to experience posterolateral nerve displacement and elongation of the main facial trunk [1], whereas vertical displacement has been observed in a case involving locally advanced mucoepidermoid carcinoma [4]. In the case of our patient, the parotid lesion caused such significant elongation and posterior displacement of the main trunk that the nerve formed a 180-degree loop anteriorly as it proceeded to the pes anserinus and the distal branches.
Displacement of the facial nerve's main trunk can render standard anatomical landmarks unreliable, necessitating an adapted surgical approach to prevent iatrogenic injury. In the case discussed, the aberrant anatomy of the main trunk prevented anterograde dissection using conventional landmarks, leading to a strategic shift to the retrograde approach. The critical nature of systematic evaluation of these landmarks, along with prompt decision-making and a resolute commitment to preserving the facial nerve, is paramount in cases featuring atypical anatomy. Insistence on dissection in the absence of recognizable landmarks may compromise the chances of atraumatic preservation of the facial nerve. While the anterograde approach is the routine choice for many surgeons in facial nerve dissection [5], the presence of anomalous anatomy or acquired aberrations, such as in revision parotidectomy cases, requires surgeons to be adept with the retrograde method or a combination of techniques to safely locate the facial nerve. In benign parotid surgery, both approaches are associated with comparable postoperative incidences of transient or permanent facial nerve injury [6].
Preoperative imaging using CT or magnetic resonance imaging (MRI) is instrumental for assessing tumor size and characteristics, as well as for predicting the tumor's location within the parotid gland. Additionally, preoperative imaging can assist in estimating the intraparotid facial nerve's position by evaluating landmarks such as the retromandibular vein. However, anatomical variations in these landmarks may lead to inaccuracies in identifying the facial nerve [7]. Consequently, it is not surprising that radiological predictions of facial nerve positioning have been reported to be accurate in only 69% of cases [8]. Considering this, surgeons might resort to multiple imaging modalities preoperatively to refine surgical planning, carefully assessing the facial nerve's trajectory, where discernible, and the degree of deep lobe involvement in the parotid lesion.
High-resolution MRI protocols that incorporate steady-state sequences and diffusion-weighted imaging have also been employed for direct visualization of the intraparotid facial nerve. A recent systematic review and meta-analysis by Lee et al. has reported facial nerve detection rates as high as 99.8% with the use of these advanced imaging techniques [9]. While such MRI protocols have yet to be universally standardized, they could be considered in situations where aberrant facial nerve anatomy is anticipated. This includes scenarios involving large tumors that extend across both superficial and deep lobes of the parotid or tumors situated near the stylomastoid foramen, potentially leading to altered facial nerve pathways.
The literature extensively details variations in the facial nerve's terminal branches [10,11], yet reports of the main trunk's anatomical deviations are less common. This case report enhances our understanding of the potential for unusual positioning of the main trunk and the possible surgical complications that could follow. Both preoperative imaging and intraoperative nerve monitoring are vital in facilitating the detection and protection of the facial nerve in surgical settings. It is crucial for surgeons to be aware of and prepared for non-standard facial nerve anatomies, employing a range of surgical techniques to secure parotid surgery's safety.
This case report elucidates uncommon anatomical deviations of the main trunk of the facial nerve, which may pose significant surgical complications. It emphasizes the critical role of preoperative diagnostic imaging and vigilant intraoperative neuro-monitoring for the accurate detection and conservation of the facial nerve's integrity. The report advocates for surgeons to maintain a high degree of awareness and preparedness for non-standard anatomical structures when undertaking parotidectomy procedures.
Received date: August 29, 2023
Accepted date: October 17, 2023
Published date: November 17, 2023
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2023 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
This report presents the first documented case of parotid NUT carcinoma with an NSD3::NUTM1 fusion, characterized by rapid metastasis and patient death five weeks post-surgery. This outcome challenges prior reports suggesting favorable survival for non-thoracic NSD3::NUTM1 tumors, indicating potential parotid-specific aggression. By integrating 13 previously published cases with the current case, the article provides a comprehensive clinicopathological reference for this rare malignancy. While further validation is required, the findings advocate for targeted NUT immunohistochemistry and molecular profiling in undifferentiated parotid tumors. BET inhibitors show therapeutic potential, underscoring the need for early recognition and precision-based care.
This article presents a case study involving a 75-year-old patient with a parotid gland lesion, highlighting the importance of facial nerve preservation during a parotidectomy. While dealing with parotid lesions, the surgical team encountered a unique anatomical aberration that deviated from the normal trajectory of the facial nerve. Consequently, they needed to employ alternative surgical techniques, transitioning from conventional anterograde dissection to a retrograde approach. This article describes a surgical experience characterized by flexibility and accuracy. It highlights the expertise required for parotid surgery, allowing readers to understand its intricate nature. Therefore, readers can gain both a deeper understanding and increased respect for the balance between surgical skill and unexpected obstacles. In this context, every choice is significant, and safeguarding the facial nerve is a primary goal. I recommend the article for publication due to its significant advantages; however, there are some issues that need to be addressed before final approval.
The study presents an in-depth analysis of a 75-year-old patient diagnosed with a parotid gland lesion, emphasizing the importance of facial nerve preservation during a parotidectomy. During the surgical intervention for the parotid lesion, the team observed an uncommon anatomical deviation that significantly deviated from the conventional facial nerve course. Consequently, this observation necessitated an adjustment in their surgical approach, leading them to transition from anterograde dissection to retrograde dissection. Despite its critical insights into the interaction between surgical expertise and unexpected challenges in parotid surgery, the case report may not be accepted for publication in its current form. There may be some concerns that need to be addressed further.
This paper details a notable case of a 75-year-old patient who initially exhibited a parotid mass, which subsequently manifested as a potential low-grade malignancy over three years. Notably, the patient exhibited displacement of the facial nerve main trunk due to the parotid lesion. The authors provide a detailed analysis of the complexities and challenges associated with anomalous facial nerve anatomy. This case study emphasizes the difficulties associated with managing parotid gland anomalies, making it a valuable resource for medical research and discourse. I believe it deserves to be published if it undergoes a few minor revisions.
In adherence to our publication's established standards, we respectfully ask for the inclusion of each author's academic and professional credentials, which may encompass designations such as MD or MD, PhD. The inclusion of these credentials enables readers to evaluate the authors' expertise and professional qualifications, thereby augmenting the comprehensive credibility and integrity of the published material.
ResponseThank you, the authors' credentials have been included.
Lee GM, Fong PY, Tan LTH, Loh ICY. Challenges associated with aberrant facial nerve anatomy in parotidectomy: A case report. Arch Otorhinolaryngol Head Neck Surg 2023;7(1):5. https://doi.org/10.24983/scitemed.aohns.2023.00175