Reconstructing extremities following tumor resection poses significant challenges, particularly when balancing limb preservation with effective cancer control. This report details the treatment of a 59-year-old male diagnosed with a malignant giant cell tumor of bone in his right distal forearm and hand. The therapeutic approach involved tumor excision and frozen radioulnar autografting to preserve the limb's structural integrity. The initial reconstruction using a latissimus dorsi flap resulted in flap necrosis, likely due to compromised blood flow, insufficient tissue coverage, and excessive tension. This complication highlighted the necessity for improved intraoperative monitoring to swiftly identify and mitigate potential perfusion issues. In the subsequent revision surgery, the team implemented a pedicled transverse rectus abdominis myocutaneous flap, enhanced with supercharging and superdrainage techniques, to better maintain the remaining tissues. This adjustment facilitated the patient’s functional recovery, enabling a quick return to chemotherapy. Four months after surgery, the patient started a structured rehabilitation program to accommodate functional changes. By the one-year follow-up, he achieved moderate independence, evidenced by an Eastern Cooperative Oncology Group (ECOG) performance status of 1 and a Disabilities of the Arm, Shoulder, and Hand (DASH) score of 34.2 out of 100. These results highlight the significant impact of innovative flap design, reconstructive techniques, and comprehensive rehabilitation in improving outcomes for complex limb reconstructions in oncological settings. Ethical considerations were central throughout the treatment, particularly due to the patient’s potentially limited life expectancy. Decision-making prioritized maximizing palliative benefits and improving the patient’s quality of life, demonstrating a compassionate approach to care in complex cases.
Managing Malignant Giant Cell Tumor of Bone
Recent advancements in surgical techniques, imaging technologies, and adjunct therapies have markedly transformed the management of malignant giant cell tumors of bone. Traditionally, these tumors necessitated limb amputation, but current approaches favor limb-preserving procedures that significantly enhance both functionality and quality of life for patients [1,2]. However, reconstructing complex upper extremity defects after tumor resection presents considerable challenges for surgeons. These include meticulous soft tissue repair and the strategic selection of flap techniques, both crucial for protecting vital structures and ensuring the long-term viability of the limb.
Gaps in Flap Reconstruction Techniques
Flap transfer plays a pivotal role in soft tissue repair within reconstructive surgery by providing crucial coverage for critical structures such as nerves and blood vessels, and it offers adaptable tissue coverage across joints. Although free flap procedures are versatile and capable of addressing large defects, they demand significant resources, including specialized surgical teams and equipment. Moreover, these procedures are associated with a higher risk of complications such as flap failure due to vascular compromise, which can result in substantial morbidity for patients [3].
In contrast, pedicled flap techniques, utilizing tissue with an intact blood supply from a nearby site, generally provide more reliable vascularization. Nonetheless, these methods come with their own set of challenges, including the need for multiple surgeries and prolonged immobilization periods that may delay recovery and rehabilitation [4]. These issues highlight the critical need for continual refinement of flap reconstruction methods to enhance their safety, efficiency, and applicability across a broader range of clinical scenarios. Improving these techniques could decrease the rate of complications and enhance the success rates of reconstructive surgeries, particularly for complex cases requiring extensive tissue coverage.
Advanced Limb Reconstruction Techniques
This case report evaluates advanced limb reconstruction techniques in the treatment of malignant giant cell tumors of bone. Initially, the surgical team utilized a latissimus dorsi (LD) flap for primary reconstruction, aiming to preserve limb functionality while ensuring effective oncological control. The discussion further explores challenges encountered with flap viability, detailing strategic responses including the use of a pedicled transverse rectus abdominis myocutaneous (pTRAM) flap enhanced by supercharging and superdrainage techniques. These modifications substantially improved vascular perfusion, contributing to both limb preservation and functional recovery. This advancement in flap reconstruction for complex surgical scenarios underscores the dynamic evolution of surgical strategies, offering essential insights for refining reconstruction techniques in the field of orthopedic oncology.
Ethical Compliance
The Research Ethics Committee of National Taiwan University Hospital granted approval for this study (project approval number 202404041W), recognizing that it met the exemption criteria under applicable governmental laws and regulations. This exemption is typically granted for studies presenting minimal risk to participants, facilitating compliance with ethical standards without necessitating a full committee review.
Patient History
This case report explores the management of a malignant giant cell tumor of bone in a 59-year-old slender male with a body mass index (BMI) of 22.3. The tumor was located in his right distal forearm and hand. The patient had a significant history of smoking, consuming a pack of cigarettes daily for 20 to 30 years, and occasionally engaged in social alcohol use. Importantly, he had no other underlying health conditions such as diabetes, hypertension, or cardiovascular disorders that could have influenced the treatment approach.
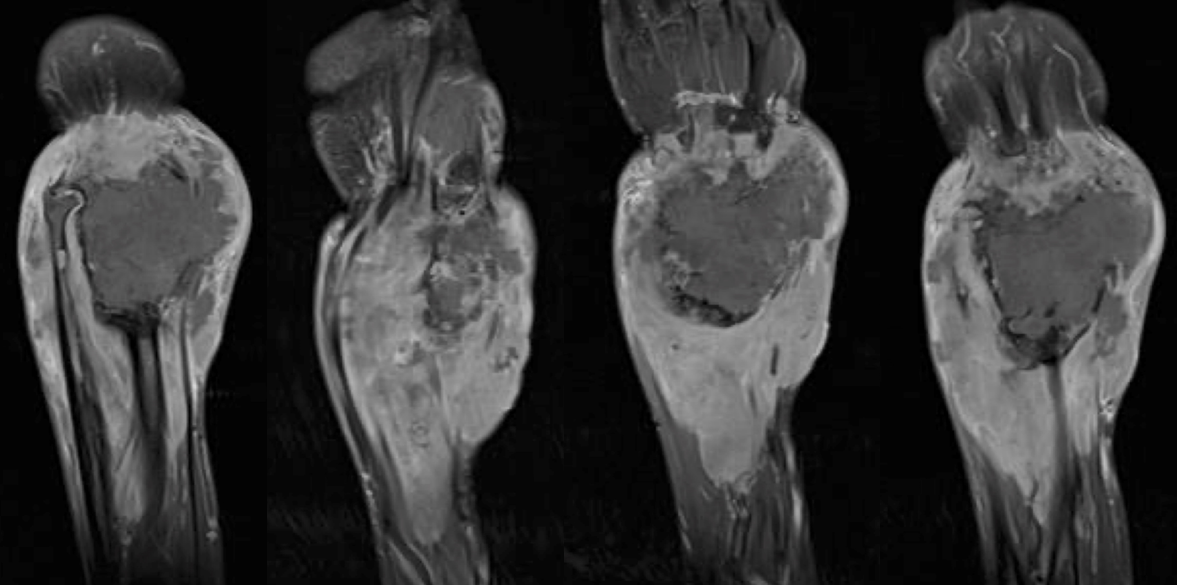
T1-weighted magnetic resonance imaging (MRI) with contrast enhancement revealed a large, expansile, and destructive tumor in the right forearm (Figure 1). The tumor displayed heterogeneous signal intensity, suggesting varied tissue characteristics. It had extensively invaded adjacent structures, including the distal ulna, carpal bones, metacarpal bases, and surrounding soft tissues. Aggressive infiltration into nearby muscles and displacement of the distal ulna resulted in joint incongruity at the radiocarpal interface. This disruption, coupled with notable soft tissue swelling, emphasized the invasive nature of the tumor. Measuring approximately 20 cm in diameter, the mass posed significant challenges for surgical intervention and treatment planning.
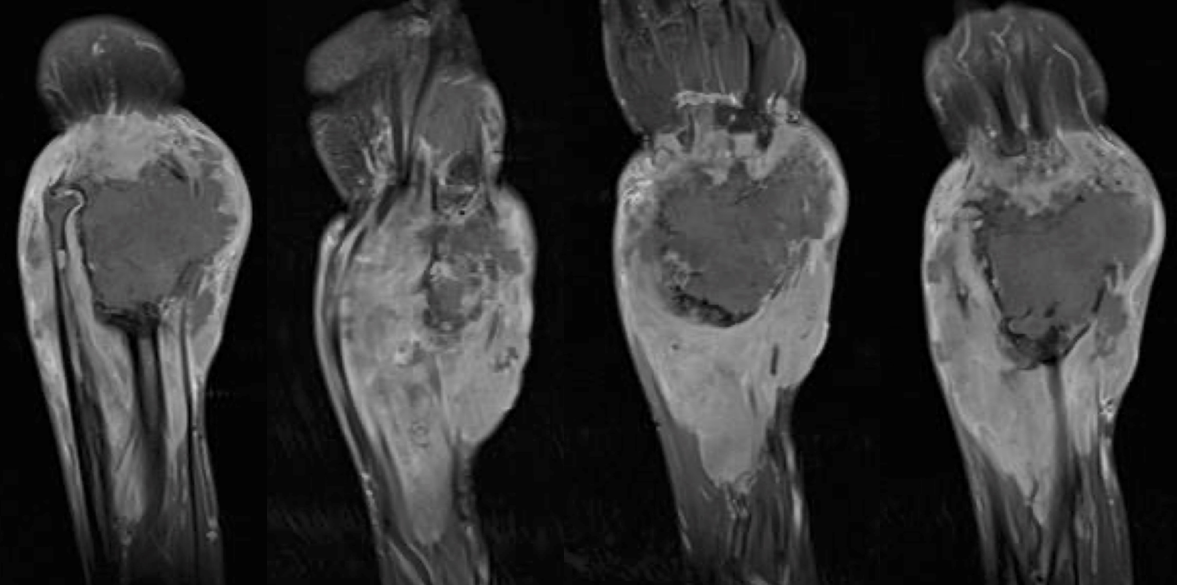
Figure 1. Preoperative T1-weighted magnetic resonance imaging (MRI) of the right forearm. This MRI with contrast enhancement reveals a large, expansile, and destructive tumor in the right forearm. The image displays heterogeneous signal intensity within the tumor, indicating varied tissue responses. Extensive involvement of surrounding anatomical structures includes the distal ulna, carpal bones, bases of the metacarpals, and adjacent soft tissues. The aggressive nature of the tumor is evident from its invasion into nearby muscles and the displacement of the distal ulna. This displacement causes joint incongruity at the radiocarpal interface, which is the joint between the radius and wrist bones, and is further complicated by significant soft tissue swelling around the tumor. The diameter of approximately 20 cm underscores the substantial size of the tumor and the complexity it adds to surgical intervention and treatment planning.
Initial Treatment Challenges
Upon the final diagnosis of a malignant giant cell tumor of bone, the patient was treated with chemotherapy using ifosfamide and epirubicin. However, after five cycles of this chemotherapy regimen, the tumor showed significant resistance, marked by the continued growth of the primary tumor and worsening of lung metastases. This lack of response indicated the ineffectiveness of the chemotherapy, necessitating a shift in treatment strategy.
Surgical intervention was thus recommended, focusing primarily on palliative locoregional control rather than curative intent. The surgery aimed to reduce the tumor burden, alleviate symptoms such as pain, and enhance the patient’s quality of life by managing the local effects of the tumor, rather than attempting to eradicate the disease or prevent further metastasis.
This approach underscores the importance of balancing aggressive treatment options with palliative care in cases of advanced cancer, aiming to enhance the patient’s quality of life even when the disease remains incurable.
Patient-Centered Surgical Decision-Making
Thorough discussions with the patient and his family were crucial for obtaining informed consent for the surgical procedure. These conversations ensured that all parties fully understood the potential risks, benefits, and alternative options, leading to an informed decision. The expected improvements in the patient’s quality of life, especially enhanced functionality and pain relief, were emphasized, given the advanced stage of the patient’s cancer.
During the decision-making process, the advantages of surgery, such as symptom relief and improved limb function, were carefully weighed against potential challenges, including the risks associated with surgery and the possibility of incomplete tumor removal. The patient’s personal goals and palliative care needs were thoughtfully considered, ensuring that the treatment plan aligned with his values and preferences. This approach was guided by key ethical principles, including respect for patient autonomy, the pursuit of beneficence by acting in the patient’s best interest, and the principle of non-maleficence, aimed at minimizing harm. These considerations allowed for the development of a personalized surgical plan that sought to balance the goals of improving the patient’s quality of life and managing disease progression.
Below-Elbow Amputation
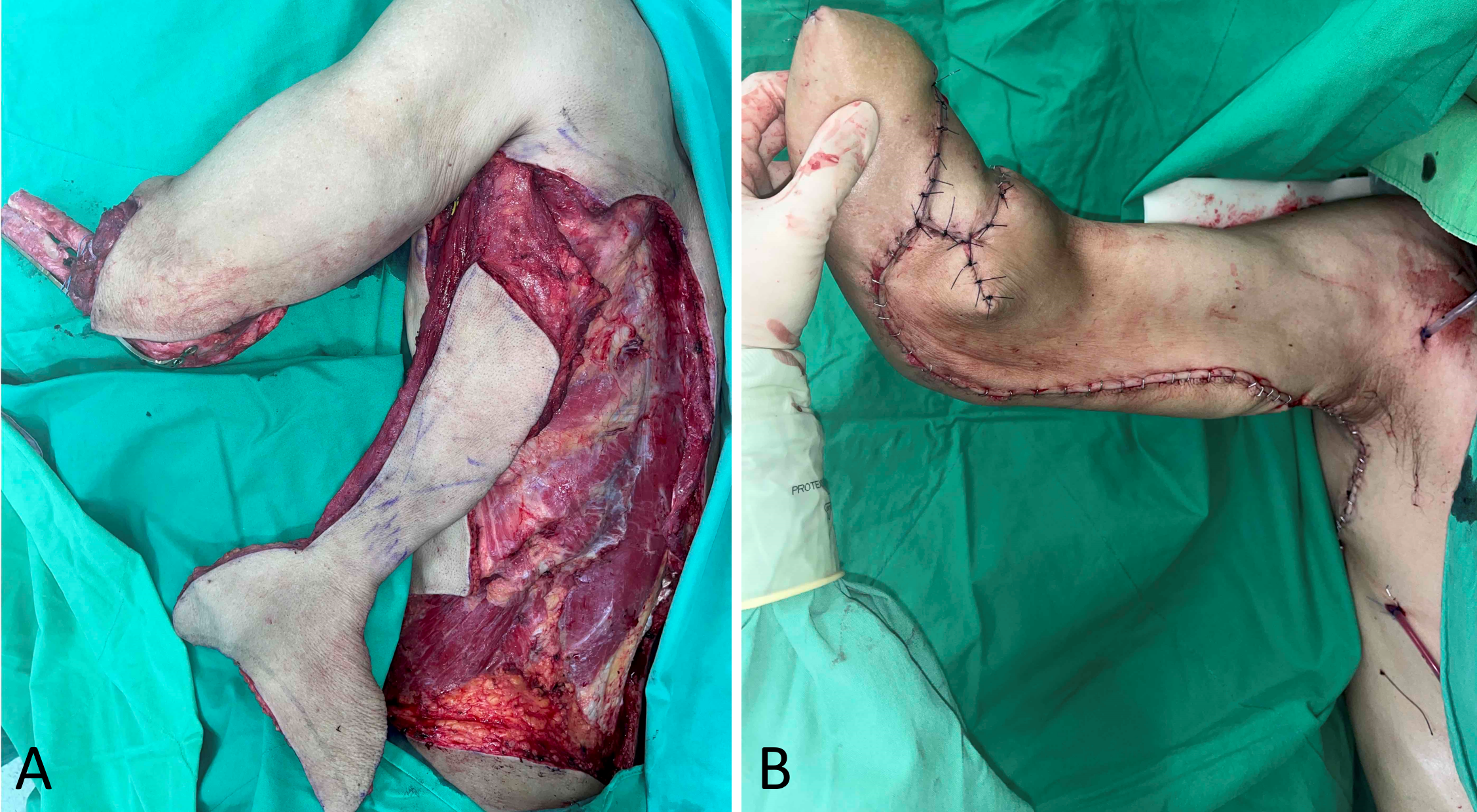
The surgical team initiated the procedure with a below-elbow amputation at the mid-forearm level to effectively remove the tumor (Figure 2). During the surgery, the team cut the ulna approximately 8 cm from the tip of the olecranon, aiming to maintain as much structural integrity of the limb as possible. In contrast, they completely removed the radius, which the tumor extensively involved, to ensure total removal of the malignant tissue and reduce the risk of residual disease.

Figure 2. Intraoperative photograph following below-elbow amputation of the right forearm. This photograph shows a 20 cm x 15 cm tumor that predominantly involves the entire radius and affects approximately 70% of the distal ulna, taken after a below-elbow amputation of the right forearm. The image highlights the extensive nature of the tumor resection. Following the resection, surgeons secure the radioulnar autograft, recycled via liquid nitrogen freezing, to the remaining forearm stump using a locking plate. Additionally, they reattach the biceps brachii muscle to ensure functional restoration.
This approach balanced the need for thorough tumor resection with the objective of preserving limb structure. By retaining a portion of the ulna, the surgery enhanced the potential for future reconstructive procedures. This decision allows for greater structural support within the limb, which can facilitate the attachment of prosthetic devices or enable additional reconstructive surgeries that might help improve the limb’s functionality and appearance.
Frozen Radioulnar Autograft for Limb Preservation
After excising the tumor, the team preserved the radioulnar autograft by freezing it in liquid nitrogen, a process known as frozen autografting. This method eliminates any residual tumor cells while preserving the bone’s structural integrity. Once thawed to room temperature, the autograft was secured using an AO olecranon locking plate, providing essential support and ensuring proper alignment.
Furthermore, surgeons reattached the biceps brachii muscle to the radial tuberosity and annular ligament, enhancing both the structural integrity and functionality of the limb. This comprehensive approach maintained the limb’s structural framework and preserved crucial functional capabilities for the patient.
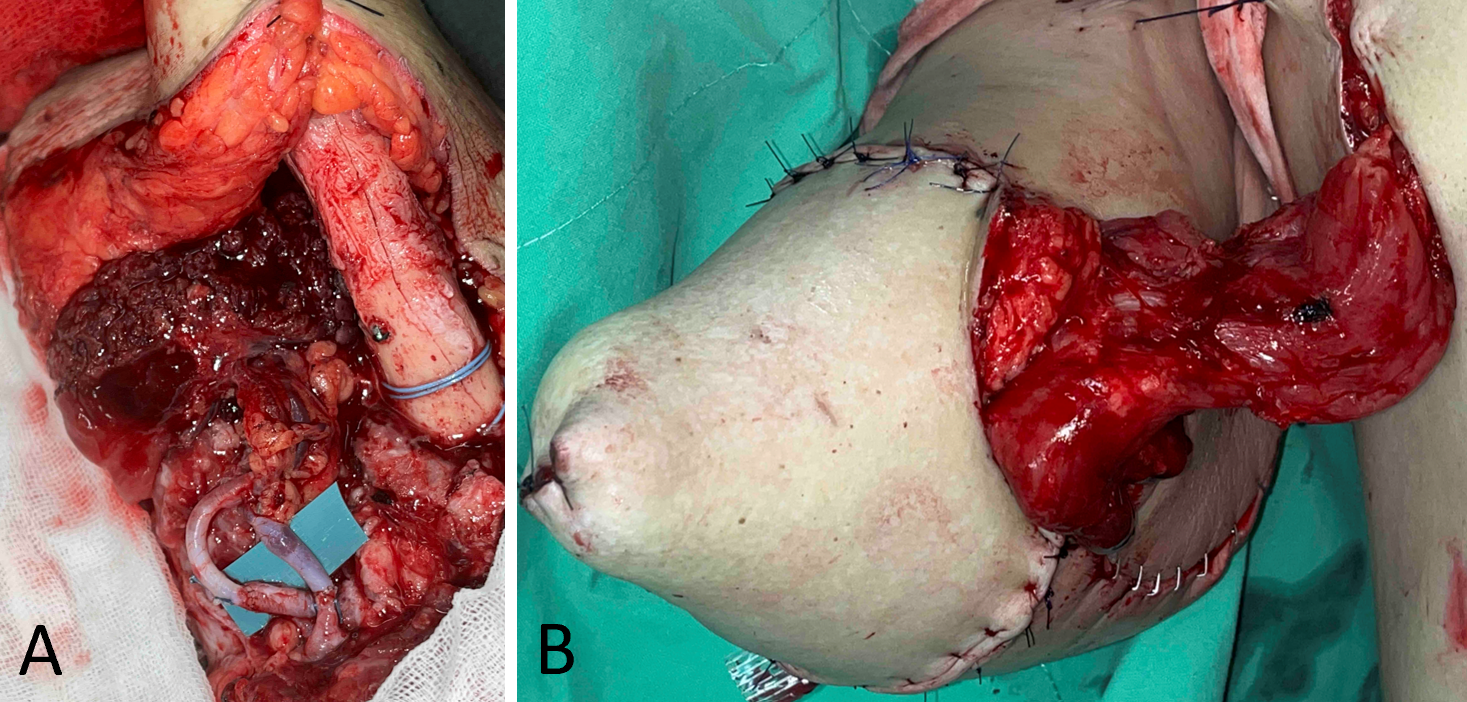
Flap Design and Reconstruction
Following the amputation, immediate reconstruction was undertaken using an LD flap, designed in an inverted T-shape with dimensions of 12 cm × 6.5 cm for the vertical strip and 20 cm × 7 cm for the double wings (Figure 3A). This design, chosen for extensive tissue coverage and optimal blood flow, is crucial for healing and minimizing the risk of flap necrosis (Figure 3B). The precise execution of the flap placement ensures the restoration of functionality and long-term viability of the reconstructed area by maintaining adequate vascularization.
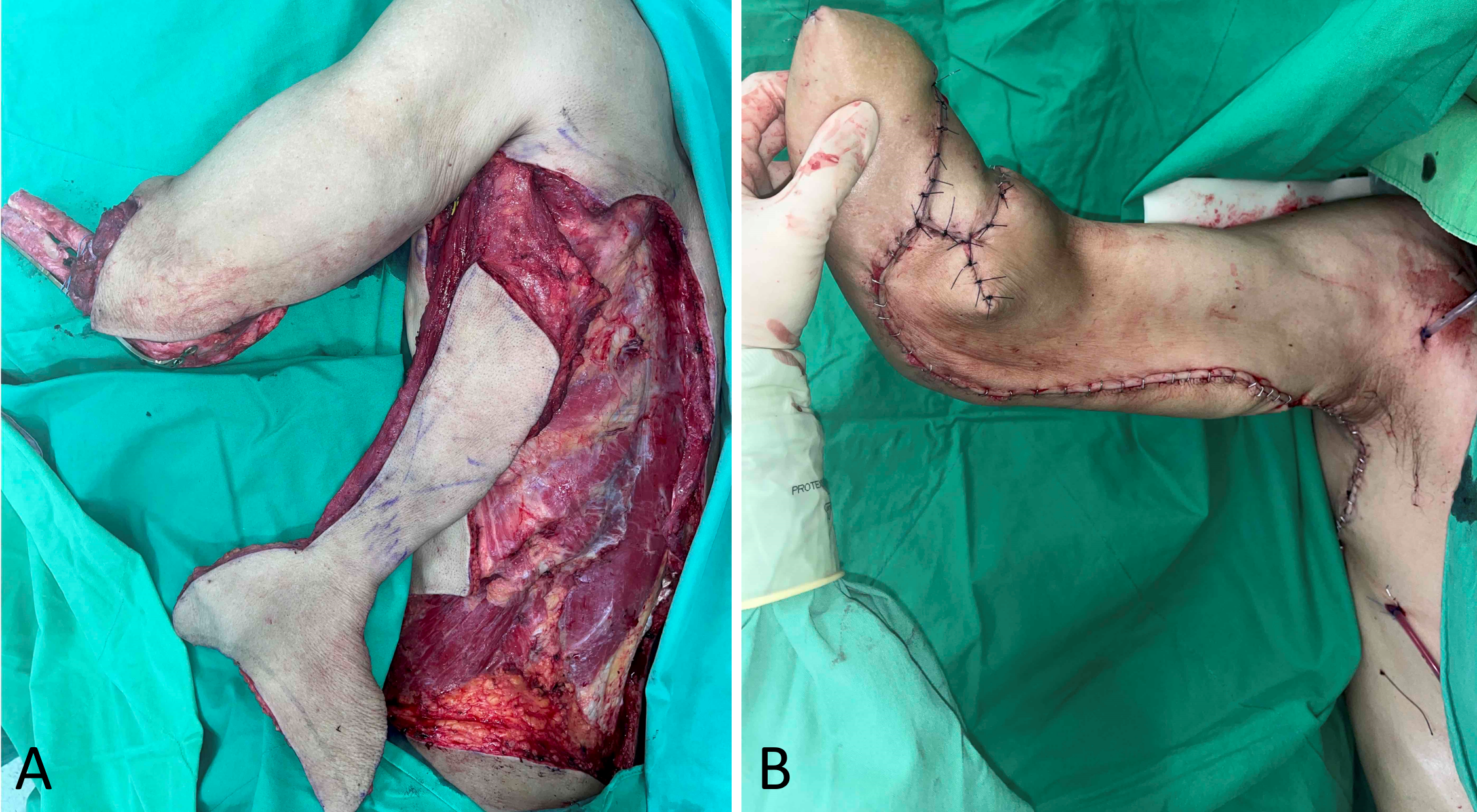
Figure 3. Flap design of the extended pedicle latissimus dorsi myocutaneous flap. (A) The flap includes an inverted T-shaped skin paddle featuring a 12 cm x 6.5 cm vertical strip over the muscle and 20 cm x 7 cm double wings for extensive tissue coverage. (B) The postoperative image demonstrates successful coverage of the radioulnar autograft with the flap, without any signs of plate exposure or ischemia, highlighting the design's effectiveness in enhancing vascularization and healing.
Early Flap Complications
On the first postoperative day, compromised distal perfusion was detected, likely due to excessive tension on the flap and inadequate soft tissue coverage over the exposed bone. This condition, worsened by pressure from the bone graft and soft tissue edema, further impeded circulation. As the week progressed, these issues led to progressive partial necrosis, affecting approximately 60% of the flap, particularly in the distal double wings. Despite early detection, the extensive tissue damage necessitated immediate corrective measures to prevent further complications.
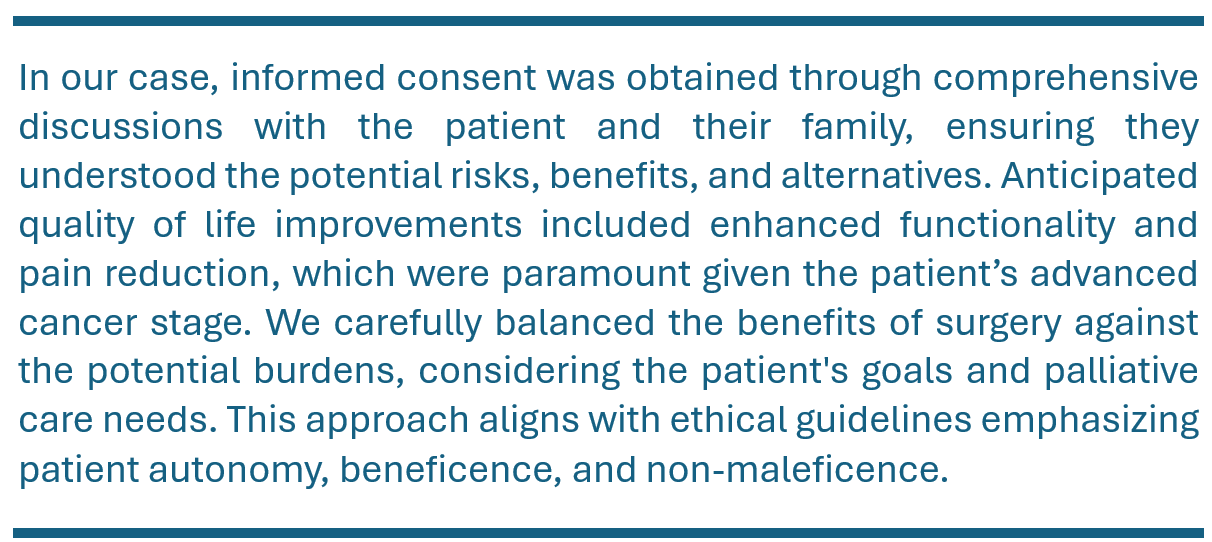
Revision Surgery
To address the critical complications, a flap revision was performed one week after the initial surgery. The corrective procedure utilized a pTRAM flap, based on the superior epigastric vessel, to provide additional vascularized tissue. The pTRAM flap was enhanced with supercharging and superdrainage techniques, establishing additional vascular connections between the deep inferior epigastric and brachial vessels (Figure 4A).
Additionally, a split-thickness skin graft (STSG) was harvested from the right lateral thigh. The graft, measuring about 0.2 millimeters in thickness, was carefully meshed and applied to cover the exposed area of the pTRAM flap (Figure 4B). This intensive surgical approach concluded with the division of the externalized pedicle four weeks later, marking the final step in the revision process.
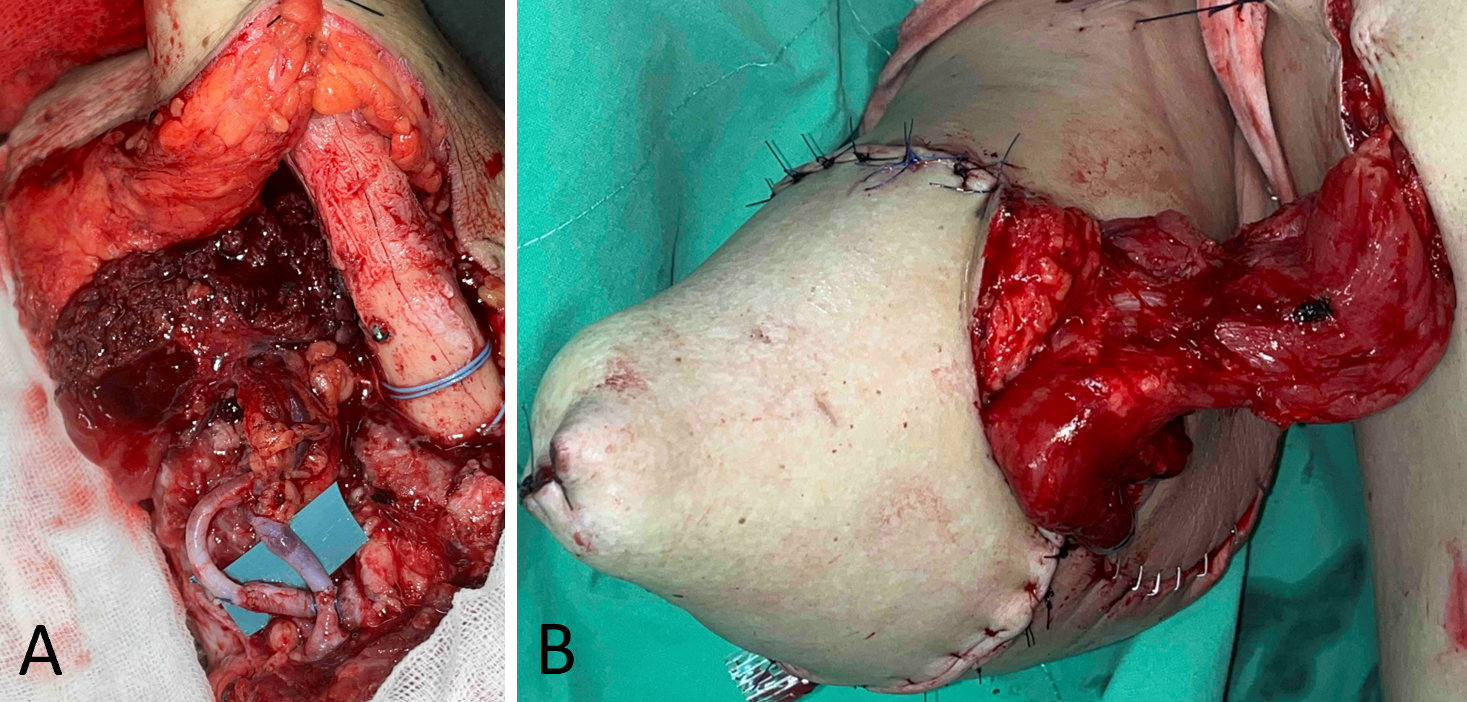
Figure 4. Revision surgery using a pedicled transverse rectus abdominis myocutaneous flap. (A) Intraoperative application of supercharge and superdrainage techniques between the deep inferior epigastric and brachial vessels to enhance vascular supply to the flap. (B) Externalized rectus abdominis pedicle, later covered with a split-thickness skin graft harvested from the right lateral thigh.
Surgical Outcomes and Oncological Treatment Progress
One month after the pTRAM revision surgery, the flap had fully healed, indicating a favorable recovery. The wound was stabilized with no signs of further complications, enabling the patient to seamlessly resume his oncological treatment. Consequently, he commenced the sixth cycle of chemotherapy, which included ifosfamide and epirubicin, without any delays. This timely recovery was crucial for maintaining the continuity of cancer treatment and enhancing the overall treatment outcome.
Rehabilitation and Performance Status
Four months after surgery, the patient began a structured rehabilitation program that included preparation for prosthesis fitting. This program was crucial for helping the patient adapt to the functional changes resulting from the amputation and for optimizing his ability to perform daily tasks. At the one-year follow-up, the patient maintained an Eastern Cooperative Oncology Group (ECOG) performance status of 1.
The ECOG performance status is a standardized tool used to assess a patient’s physical capability, particularly their ability to care for themselves and perform everyday activities [5]. The scale ranges from 0 to 5, with 0 indicating full activity without restriction and 5 indicating death. A status of 1 signifies that the patient is limited in physically strenuous activities but remains ambulatory and capable of light or sedentary work.
This status reflects the patient’s resilience in overcoming the physical challenges post-surgery and underscores the effectiveness of the rehabilitation program. Maintaining an ECOG score of 1 highlights the success of the surgical and rehabilitative interventions in enabling the patient to achieve a satisfactory level of independence and functionality.
Functional Recovery and Prosthesis Use
At the one-year postoperative assessment, the patient effectively used a functional prosthesis, as demonstrated by a Disabilities of the Arm, Shoulder, and Hand (DASH) score of 34.2 out of 100.
The DASH score, a widely recognized and standardized tool, assesses upper-limb disability and symptoms [6]. It is extensively applied in both clinical practice and research to evaluate patient outcomes and functional recovery. The assessment includes 30 items that measure the patient’s ability to perform daily activities, the severity of symptoms, and the impact on social and occupational roles. Scores on the DASH scale range from 0 to 100, where lower scores indicate better function and fewer disabilities, and higher scores suggest greater disability and functional limitations.
A score of 34.2 indicates moderate disability. This underscores that although the patient experienced some functional limitations, he was still capable of performing certain tasks independently. This score provides valuable insight into the patient’s level of functional recovery and the effectiveness of the prosthesis in helping him regain a degree of independence in daily activities.
Rebuilding Function Through Multi-Stage Surgery
One year after surgery, the patient regained the ability to perform tasks such as writing and holding a cup, which represents a notable improvement in his recovery (Figure 5). This progress highlights the success of the surgeries, designed both to alleviate symptoms and achieve local oncological control, and to enhance hand functionality through a tailored prosthesis. The strategy effectively balanced oncological management with reconstructive outcomes, prioritizing the improvement of the patient’s quality of life by restoring intricate hand movements. Through careful planning and skilled execution, the surgical team significantly improved the patient’s physical independence and overall well-being.

Figure 5. Functional recovery of the patient one year after surgery, demonstrating the use of a prosthesis. (A) The patient is shown writing, illustrating restored hand functionality. (B) The patient independently holds a cup and drinks water, highlighting successful rehabilitation and improved daily living capabilities postoperatively.
Challenges in Extremity Reconstruction After Amputation
Recent advancements in the survival rates of patients with malignant giant cell tumors of the bone have underscored the need for durable and functional reconstruction methods following tumor resection [2]. As treatments evolve, the emphasis has shifted towards enhancing long-term functionality and improving quality of life for patients undergoing extensive surgeries. Effective techniques must not only achieve the primary oncological goal of tumor removal but also ensure the structural and functional rehabilitation of the affected limb.
However, reconstructing extremities post-amputation remains challenging due to limited availability of soft tissue and the presence of exposed bone or hardware, which complicates healing and increases the risks of infection and graft failure. Additionally, exposed hardware can disrupt tissue integration, leading to further complications such as wound dehiscence. Developing innovative reconstruction strategies to address these issues is critical for optimizing both patient outcomes and long-term limb viability.
Innovative Techniques for Reconstruction
To address challenges in reconstructing extremities with limited soft tissue and exposed bone, Igarashi et al. introduced frozen autografting in 1999 [7]. This method involves freezing excised bone in liquid nitrogen after curettage for later re-implantation. The autograft, once thawed, is secured with locking plates and screws to maintain structural integrity in the absence of ample soft tissue. This technique reduces local recurrence risks and supports complex reconstructions involving exposed bone.
In our case, frozen autografting combined with stabilization using an AO olecranon locking plate effectively preserved the limb’s structural integrity after excising a malignant giant cell tumor. Reattaching the biceps brachii to the radial tuberosity and annular ligament also restored limb functionality, demonstrating the technique’s ability to maintain both structure and function.
A retrospective multicenter study by Takeuchi et al. supports the use of tumor-devitalized autografts, analyzing 310 patients with benign and malignant bone tumors [8]. The study reported graft survival rates of 87% at five years and 81% at ten years, proving frozen autografting to be a reliable method for preserving bone integrity and function over the long term. These findings emphasize the durability and clinical utility of frozen autografts in complex bone reconstructions post-tumor resection.
Flap Choice for Soft Tissue Coverage
Innovative techniques such as frozen autografting provide robust solutions for bone integrity and functional restoration. However, ensuring adequate soft tissue coverage remains a critical aspect of successful limb reconstruction. It is essential to provide sufficient soft tissue to cover exposed bones and hardware to prevent complications like infection, wound dehiscence, and mechanical failure of the reconstruction. While preserving bone structure through autografting is crucial, the significance of soft tissue reconstruction, especially in cases requiring large donor areas for optimal coverage, is paramount.
In our case, the unique dome shape of the remaining forearm stump necessitated a larger donor tissue area compared to a simpler, flat defect. Initially, we considered free flaps such as the LD myocutaneous flap, deep inferior epigastric perforator flap, and anterolateral thigh flap. However, due to concerns over potential flap loss, treatment delays, and the technical demands of these procedures, we explored alternative solutions. We ultimately selected the pedicled LD flap, which provided significant vascularized muscle volume for effective radioulnar graft coverage without the need for microvascular anastomosis [9]. We also evaluated simpler elevation pedicled flaps like the thoracodorsal artery perforator flap and lateral intercostal artery perforator flap, but their smaller volumes made them less suitable [10].
This focus on flap selection underscores a key aspect of this case, as successful soft tissue coverage significantly impacts overall outcomes in extremity reconstruction. Achieving optimal results in complex limb reconstructions demands a careful balance between advanced bone reconstruction techniques and strategic flap selection.
Advancements in Flap Monitoring Techniques
Despite rigorous preoperative planning, we encountered partial flap loss, likely due to compromised blood flow from extended harvest times. This highlights the importance of advanced intraoperative monitoring to promptly detect perfusion issues. Indocyanine green angiography (ICGA) stands out as a valuable tool in this context. It provides objective assessment of vascular patency in free flaps and identifies ischemic areas in pedicle flaps. By offering real-time data on blood flow, ICGA can identify intraoperative hypoperfusion, a key factor that significantly increases the risk of distal flap necrosis and healing delays [11,12].
The utility of ICGA in reducing postoperative flap necrosis has been substantiated by clinical studies. A Cochrane review of nine non-randomized cohort studies, involving 1,589 women and 2,199 breast reconstructions, compared the efficacy of ICGA with traditional clinical evaluations [13]. The review indicated that ICGA might reduce the incidence of necrosis, reoperation, and infection. Although promising, further investigation via randomized controlled trials is crucial to comprehensively validate the benefits of ICGA in surgical outcomes.
As we refine our flap monitoring techniques, the team continues to evaluate potential modifications to the fasciocutaneous component of the LD flap to enhance perfusion in its distal regions. These enhancements are designed to increase blood flow, which may reduce complications such as flap necrosis and improve overall tissue integration. However, it is vital to carefully assess these modifications, as they could lead to increased morbidity at the donor site. A comprehensive evaluation of these risks versus the benefits is essential to ensure that any changes do not compromise patient safety and recovery.
Enhancing pTRAM Flaps: Supercharging and Superdrainage
To address the partial loss of the initial LD flap, we utilized a pTRAM flap based on the superior epigastric vessel. This approach provides additional vascularized tissue and ensures adequate perfusion. Unlike traditional breast reconstruction, which enhances vascular supply through a subcutaneous tunnel, our method employs an externalized pTRAM flap. This allows for direct visualization of both arterial inflow and venous outflow, facilitating improved monitoring and reducing the risk of vascular compromise due to soft tissue pressure.
Since Hartrampf et al. introduced the pTRAM flap in 1982, it has seen various modifications, including adaptations for free flaps, aimed at reducing donor-site morbidity and enhancing flap viability [14]. However, maintaining sufficient distal perfusion remains challenging, particularly when the flap relies on a single vascular anastomosis. In response, Beegle introduced the “supercharging” technique in 1991 [15]. This method creates an additional anastomosis between the epigastric system and either the internal mammary or thoracodorsal systems, thereby enhancing blood flow to the distal regions of the flap. Several case reports have affirmed the effectiveness of this technique in improving perfusion [16,17].
In our implementation, we employed the supercharging technique to enhance arterial blood flow and secure the viability of the pTRAM flap. We also incorporated the “superdrainage” technique to improve venous outflow, critical for preventing venous congestion. Venous congestion can lead to complications such as flap edema and necrosis if not adequately managed. Despite the clear benefits of superdrainage, retrospective studies suggest that up to 38% of cases may still exhibit persistent or worsened perfusion post-application [18]. This underscores the technique’s value and potential risks. Therefore, careful patient selection, precise surgical execution, and thorough postoperative monitoring are imperative to minimize the risks associated with venous insufficiency and optimize overall flap outcomes.
Ethical Considerations in Advanced Cancer Surgery
Surgical intervention for advanced malignant giant cell tumor of bone presents significant ethical considerations, especially when weighing the limited life expectancy of patients against the potential benefits of surgery. The primary ethical challenge centers on the appropriateness of aggressive surgical interventions, such as tumor resection and limb reconstruction, in cases where the disease is generally incurable. Although surgery can alleviate symptoms, enhance functionality, and potentially improve quality of life, it also prompts scrutiny over the physical burden and risks associated with extensive procedures given the patient’s prognosis.
The decision to proceed with surgery must prioritize patient autonomy, informed consent, and alignment with the patient’s goals, ensuring a comprehensive understanding of the realistic outcomes and limitations. In this instance, despite the advanced stage of the disease, the surgery significantly improved daily function and quality of life, illustrating that surgery can offer substantial palliative benefits even with a limited life expectancy. However, such decisions should be made on an individual basis, supported by thorough multidisciplinary discussions that emphasize the ethical principles of beneficence and non-maleficence. This approach aims to maximize patient well-being while minimizing potential harm.
Study Limitations
This study underscores the collaborative efforts between orthopedic and plastic surgeons in employing multimodal complex flap reconstruction for extensive soft tissue and bony defects. While this approach resulted in a favorable functional outcome for the amputee patient, several limitations warrant mention. The preoperative planning was deemed adequate; however, the absence of advanced postoperative circulation monitoring tools, such as ICGA, limited early detection of perfusion-related issues. Earlier identification and intervention could potentially have mitigated the risk of tissue loss. Looking ahead, incorporating advanced monitoring technologies like ICGA is essential. These measures are expected to enhance flap viability and improve overall patient outcomes in similar complex reconstructive surgeries. Focusing on these improvements is crucial for reducing complications such as necrosis and ensuring the long-term efficacy of surgical interventions.
This case illustrates the utilization of established reconstructive techniques, such as frozen autografting and LD flaps, in managing complex limb defects after tumor resection. Despite encountering complications like flap necrosis, revision surgery that incorporated pTRAM flaps with supercharging and superdrainage techniques was crucial in restoring vascular perfusion and salvaging the limb. This strategic and adaptable approach underscores the importance of early detection of perfusion-related issues, multidisciplinary collaboration, and continuous refinement of existing flap techniques in complex reconstructions. Furthermore, this case highlights how patient-centered decision-making, careful surgical planning, and timely interventions can significantly enhance functional recovery in high-risk scenarios.
Received date: July 15, 2024
Accepted date: August 08, 2024
Published date: September 24, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)’ autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.


A significant increase in peripheral nerve surgery has occurred in recent years due to improvements in surgical techniques. In most reconstructive procedures, sensory restoration is frequently neglected in preference to restoring motor function. Along with increasing the risk of developing injuries to the body, patients who lose protective sensations are more likely to develop neuropathic pain and depression, which adversely affect their quality of life. As regaining sensory function is important, the study examines a variety of techniques that may be useful for restoring sensory function across various body parts.
This study introduces an advanced tubularized radial artery forearm flap (RAFF) technique, marking an enhancement over traditional methods in addressing complex nasal reconstructions. It integrates functional and aesthetic considerations through a structured, multi-stage reconstruction process, emphasizing the use of tubularized flaps. Key learning points include the detailed crafting of stable nasal passages, strategic use of costal cartilage for robust structural support, and tailored postoperative care with silicone splints. The tubularized RAFF technique not only optimizes patient outcomes and quality of life but also provides plastic surgeons with critical insights to refine their techniques in facial reconstruction. Indispensable for professionals in the field, this article enriches the understanding of sophisticated reconstructive challenges and solutions.
This article presents a crucial case report on potential wound healing complications linked to fremanezumab, a calcitonin gene-related peptide-targeting antibody for migraine prevention. It documents the first known instance of delayed wound healing following a free flap breast reconstruction, underscoring the need for heightened clinical vigilance and individualized patient assessment in perioperative settings. Highlighting significant safety data gaps, the report advocates for comprehensive research and rigorous post-marketing surveillance. The findings emphasize the importance of balancing the risks of delayed wound healing with the need for effective disease control, especially when using biologic agents for chronic conditions. This article is essential for medical professionals managing patients on biologic therapies, offering critical insights and advocating for a personalized approach to optimize patient outcomes. By presenting novel observations and calling for further investigation, it serves as a vital resource for enhancing patient care and safety standards in the context of biologic treatments and surgical interventions.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
The likelihood of donor site ischemia following the harvesting of a fibula flap is extremely low, but it is potentially lethal if it occurs. The authors describe a case of ischemia of the lower extremity following a free fibula harvest for head and neck reconstruction. The authors discuss preoperative, intraoperative, and postoperative strategies to assist in diagnosing and managing risks associated with free fibula flap harvesting in this paper.
This study introduces an advanced tubularized radial artery forearm flap (RAFF) technique, marking an enhancement over traditional methods in addressing complex nasal reconstructions. It integrates functional and aesthetic considerations through a structured, multi-stage reconstruction process, emphasizing the use of tubularized flaps. Key learning points include the detailed crafting of stable nasal passages, strategic use of costal cartilage for robust structural support, and tailored postoperative care with silicone splints. The tubularized RAFF technique not only optimizes patient outcomes and quality of life but also provides plastic surgeons with critical insights to refine their techniques in facial reconstruction. Indispensable for professionals in the field, this article enriches the understanding of sophisticated reconstructive challenges and solutions.
The article provides groundbreaking insights into complex limb reconstruction by emphasizing innovative surgical techniques and multidisciplinary collaboration. It highlights the successful application of pedicled flaps, particularly the thoracoabdominal flap, to salvage elbow function and forearm length following sarcoma resection. This approach demonstrates the flap’s efficacy as a viable alternative to free flaps, underscoring the critical importance of adaptability and precision in surgical planning. The meticulous techniques detailed offer significant improvements in quality of life for patients with similar conditions, showcasing both surgical ingenuity and the resilience of medical practice. This article is indispensable for its detailed procedural insights, balancing cutting-edge techniques with patient-centered care. Its publication is justified, contingent upon addressing minor clarifications and methodological details, thereby demonstrating the authors' expertise and significant contribution to advancing reconstructive surgery.
The authors' work presents notable advancements in limb reconstruction, yet several critical issues must be addressed for publication. The manuscript lacks detailed information on the patient’s medical condition, such as cancer stage, tumor size, and relevant history, including prior treatments and comorbidities. The rationale for the timing of secondary reconstruction requires clarification, explaining the decision for a four-week interval. Additionally, a thorough analysis of complications related to compromised distal perfusion and bone graft compression is needed, including contributing factors and mitigation strategies. Addressing these points will enhance the manuscript's clarity and rigor. As it stands, these concerns suggest the article is not yet ready for publication in its current form.
The authors present a valuable contribution with "Salvage of elbow function and forearm length by using pedicled flaps after sarcoma resection," highlighting innovative techniques in limb reconstruction. This article is particularly valuable for plastic surgeons as it demonstrates advanced methods for addressing complex reconstructive challenges, emphasizing the importance of multidisciplinary approaches and meticulous planning. Despite a few concerns, the article remains suitable for publication after minor revisions. The Discussion should acknowledge study limitations and insights gained. Clarification on recovery milestones, including wound healing, rehabilitation start, and timing of ECOG 1 and DASH scores, is needed. Additionally, specifying when Figure 5 was taken post-surgery is crucial for contextualizing recovery. The article demonstrates expertise and is nearly ready for publication, requiring only minor tweaks.
My concerns have been meticulously addressed, leading to a significant improvement in the manuscript's clarity and depth. Comprehensive details on the patient's medical condition, including cancer stage, tumor size, treatment history, and comorbidities, have been included. The rationale for the timing of secondary reconstruction has been clarified, offering insight into the specific patient conditions that required early intervention. Additionally, the authors have elaborated on the complications of compromised distal perfusion and bone graft compression, detailing contributing factors and mitigation strategies. These detailed revisions underscore the thoroughness and robustness of the study, indicating that the manuscript is now suitable for publication.
The authors have effectively resolved the issues raised in my previous review, implementing substantial modifications that improve both the clarity and rigor of the manuscript. They have added a detailed discussion on the study's limitations and the lessons learned, which enriches the narrative and provides a balanced perspective. The timeline for the patient's recovery milestones, including wound healing, initiation of rehabilitation, and the assessment timings for the ECOG 1 and DASH scores, has been clearly delineated. Additionally, they have clarified that Figure 5 was taken one year post-surgery, which contextualizes the recovery process effectively. Moreover, the substitution of X-ray images with MRI enhances the visual accuracy and precision of the data presented. These revisions collectively ensure that the article meets the high standards required for publication and offer valuable insights into advanced reconstructive techniques
Lee HY, Chao SC. Upper extremity reconstruction post-tumor resection: Innovations and challenges in limb preservation for advanced-stage malignant giant cell tumor of bone. Int Microsurg J 2024;8(2):2. https://doi.org/10.24983/scitemed.imj.2024.00191