Three-dimensional nasal reconstruction poses significant challenges, especially in cases involving total nasal defects accompanied by adjacent tissue loss. The complex anatomy of the nose, crucial to both aesthetics and function, complicates achieving successful outcomes. Autologous reconstruction using free flaps, such as the radial artery forearm flap (RAFF), often becomes necessary due to the scarcity of local tissue. However, conventional RAFF techniques may not adequately address extensive defects and complex anatomical disruptions. This study details the treatment of a 27-year-old patient with a total nasal defect from childhood mucormycosis using a novel tubularized RAFF technique, a method not previously documented in the literature. This technique was developed specifically to tackle the multifaceted challenges presented by significant nasal and adjacent structural damage. The reconstruction process was meticulously planned and executed in four distinct phases, each focusing on specific defect aspects to ensure a comprehensive approach. The method involved constructing stable nasal passages with skin-lined tubes, supported by temporary splints to prevent collapse, and reinforcing the nasal framework with costal cartilage to ensure structural stability. Postoperative assessments confirmed the successful integration of the radius bone into the central maxilla without any flap-related complications. The successful outcome of this case illustrates the potential of the tubularized RAFF technique to offer effective solutions for managing total nasal defects with adjacent structural deficiencies.
Nasal defects significantly affect the physical health, social interactions, and psychological well-being of patients [1]. Arising from various causes, including trauma, infections, inflammatory diseases, exposure to toxins, and neoplasms [2], these defects necessitate effective treatment to enhance the quality of life. The nose plays a crucial role in facial aesthetics, influencing appearance and self-esteem, and is indispensable for essential functions such as breathing and olfaction [3]. Addressing these defects is vital for restoring both the appearance and the essential functions of the nose, thereby improving the overall health and emotional well-being of patients.
Nevertheless, achieving both aesthetically pleasing and functionally effective reconstruction in cases of complete nasal defects presents considerable challenges. These challenges primarily arise from the unique characteristics of nasal skin, such as its texture, thickness, and elasticity, which add significant complexity to the reconstruction process. Additionally, the intricate anatomy of the nose and its pivotal role in facial symmetry further complicate surgical efforts. Addressing these complexities requires meticulous planning, detailed preoperative assessments, customized surgical strategies, and precise execution. The use of appropriate cartilage grafts is crucial in overcoming these challenges. These grafts provide the necessary support to the reconstructed nasal structure, ensuring both stability and functionality. This approach is key to achieving successful surgical outcomes.
Among the various flaps used in nasal reconstruction, the radial artery forearm flap (RAFF) is commonly used. This procedure involves harvesting tissue from the forearm and folding it to reconstruct multiple nasal components, including the nasal lining and external structure [4]. However, in cases of extensive circumferential loss of nasal lining and apertures, traditional RAFF applications may be insufficient, as they might not provide adequate coverage or structural integrity, potentially resulting in suboptimal reconstruction outcomes.
To address the limitations inherent in conventional RAFF techniques for treating complex nasal defects, the authors have developed an innovative approach. This method involves tubularizing the RAFF to facilitate comprehensive nasal reconstruction, particularly in cases following severe infections. In this study, the technique was applied to a 27-year-old patient with a total nasal defect caused by a childhood infection, resulting in significant improvements in both functional and aesthetic outcomes. The findings provide valuable insights into advanced surgical strategies, highlighting the potential of the tubularized RAFF to refine and enhance current reconstructive practices through more tailored approaches.
A 27-year-old man presented with a complex nasal defect, stemming from mucormycosis contracted in childhood. With no other significant medical history, he faced numerous barriers to receiving reconstructive surgery, leading to profound social discomfort over the years. Consequently, he often wore masks to avoid social encounters. Although he did not experience breathing difficulties, he reported frequent episodes of throat dryness, a symptom likely linked to his altered nasal anatomy and disrupted airflow dynamics.
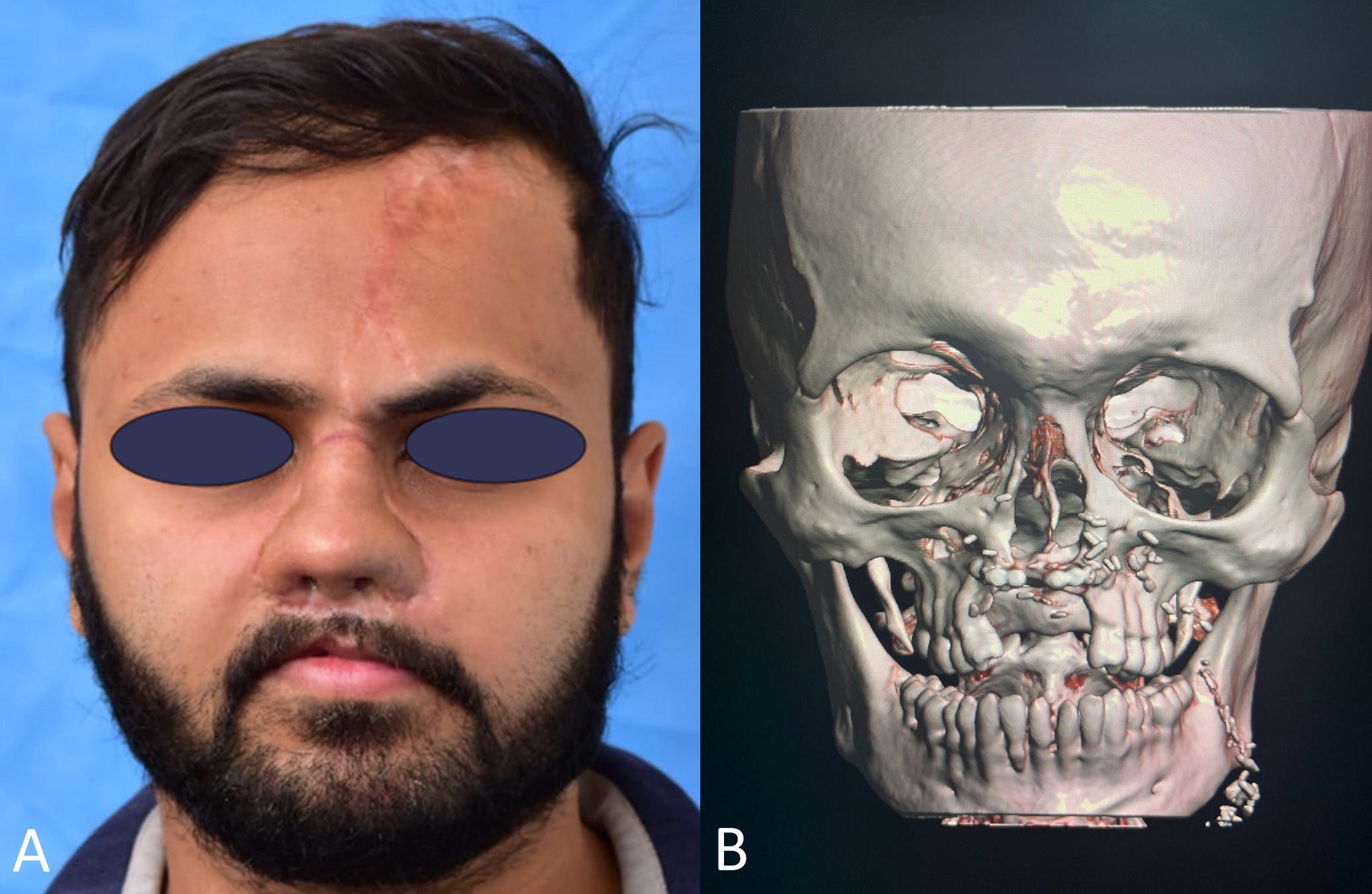
A comprehensive examination revealed a complete loss of the nasal lining, structural support, and external cover. The anterior palate, incorporating four incisors, was severely damaged and displaced into the nasal cavity (Figure 1A). Externally, the nasal airway displayed significant alterations, characterized by a solitary opening at the level of the nasal bones. Despite these extensive external distortions, both computed tomography scans and nasal endoscopy affirmed that the internal nasal anatomy was intact and preserved.
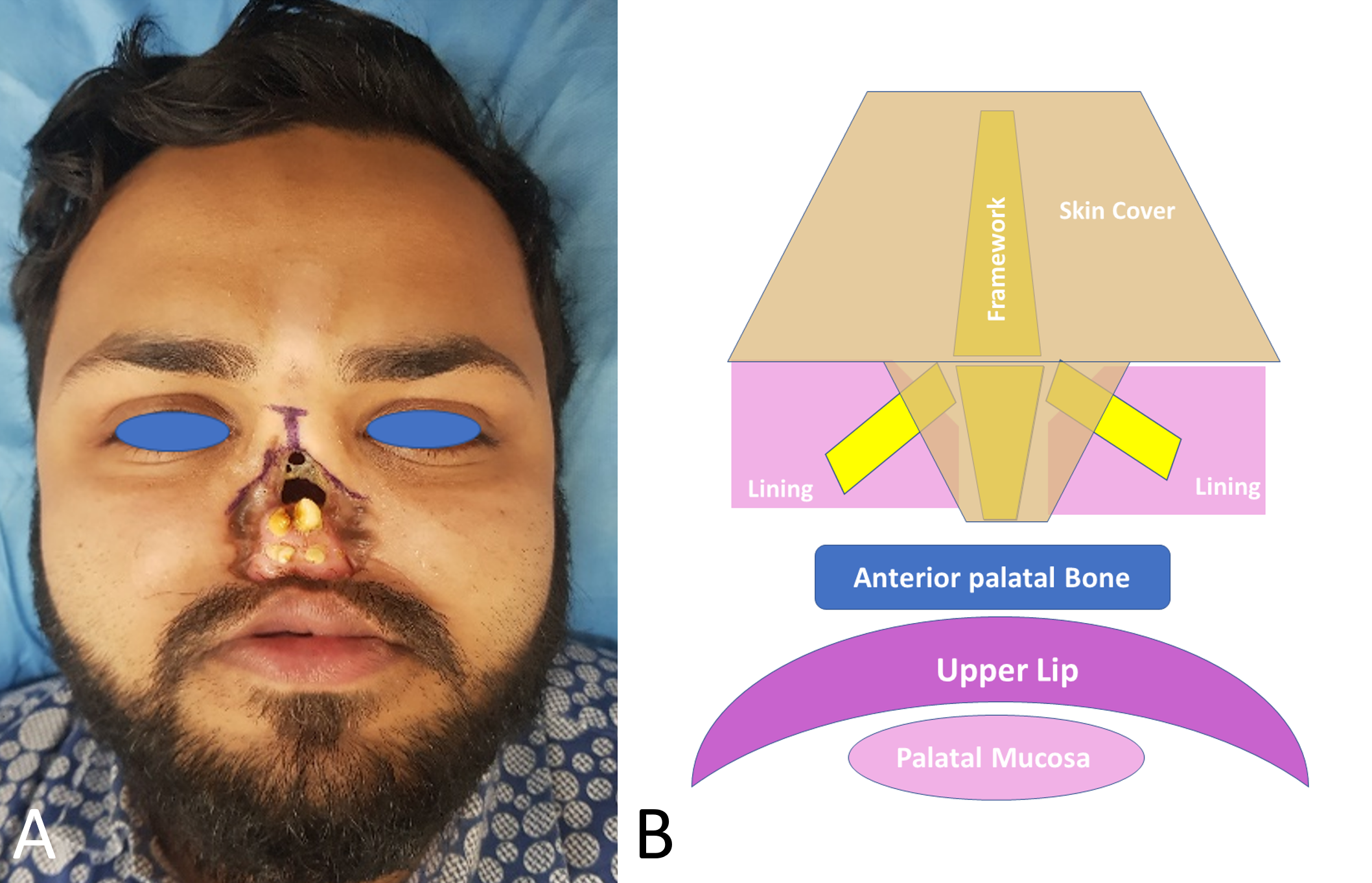
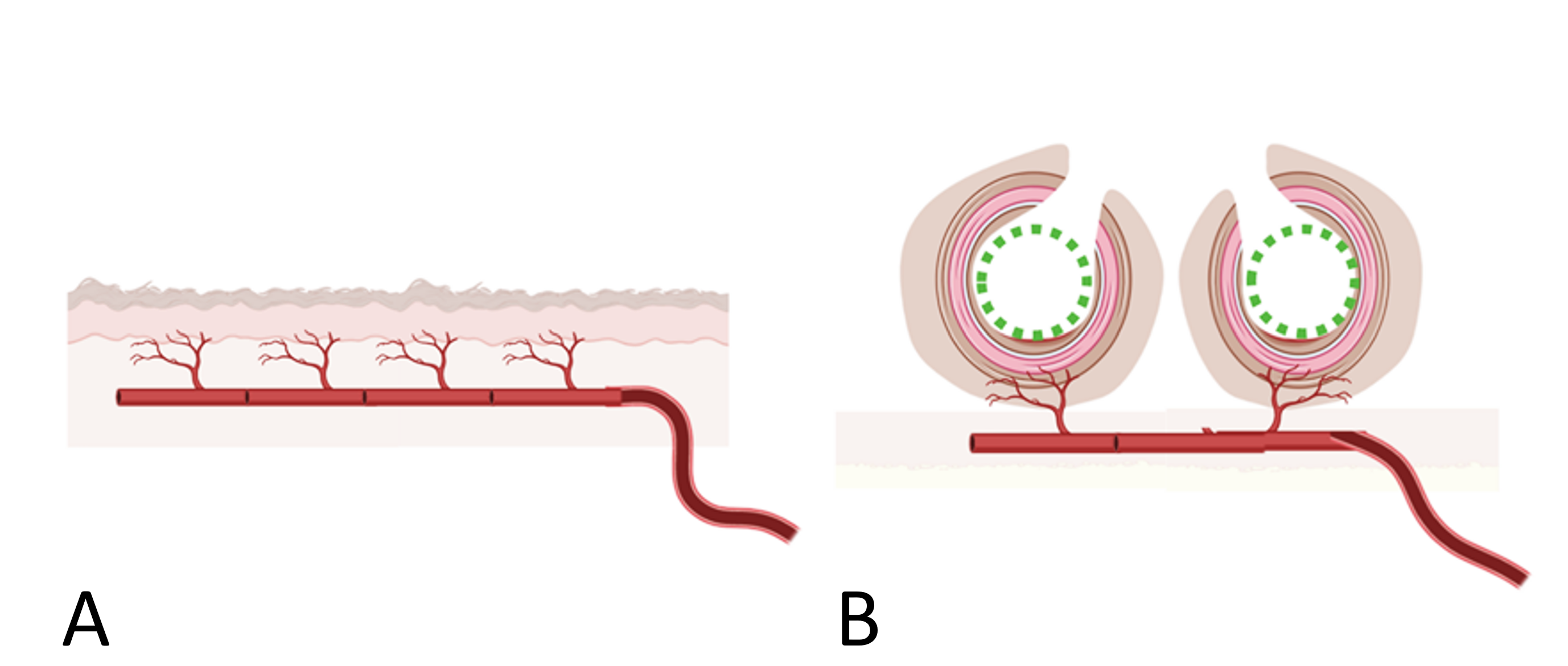
Figure 1. Preoperative nasal defect and reconstructive strategy. (A) Clinical photograph depicting a severe total nasal defect resulting from childhood mucormycosis, characterized by an extensive loss of nasal tissue, including the lining, structural support, and external coverage. The anterior palate, including four incisors, is severely damaged and displaced into the nasal cavity, further exacerbating the facial deformity. (B) Schematic diagram illustrating the planned reconstructive approach, showing the framework for nasal reconstruction with meticulously designed skin cover and lining, arranged around the essential structural components.
Additionally, the patient had a vestibulo-nasal fistula, an abnormal connection between the nasal cavity and the oral vestibule. Extensive scarring extended from the nasal region to the upper lip, leading to a lack of alveolar support crucial for tooth stability. Consequently, this resulted in a retruded mid-facial profile, marked by the backward displacement of the mid-face area.
Extensive scarring and severe defects had profoundly altered the facial structure and appearance of the patient. To effectively address these multifaceted challenges, a meticulously planned and detailed reconstructive strategy was essential. Consequently, the tubularized RAFF technique was applied. This approach focused on restoring aesthetic appeal and reinstating functional capabilities, ensuring optimal outcomes for the patient.
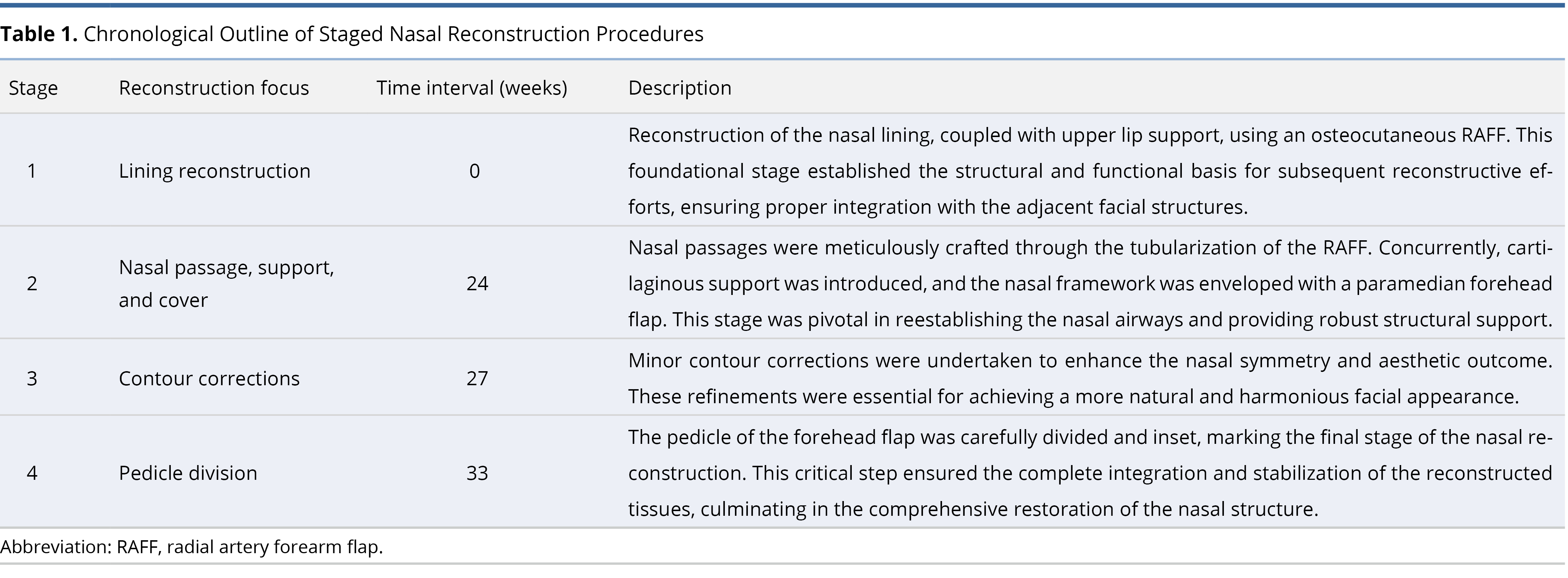
The nasal reconstruction was meticulously organized into four distinct stages, each tailored to address specific aspects of the complex defect (Table 1). The initial planning stage involved precise design and customization, aimed at achieving both functional and aesthetic outcomes. Nasal lining and external cover were methodically planned using templates, which were applied over a cartilaginous framework to replicate the nasal structure (Figure 1B). This framework provided essential support and shape, ensuring the final outcome was stable and aesthetically appealing. Detailed descriptions of the techniques and strategies used at each stage are provided in the subsequent sections.
Stage 1: Lining Reconstruction
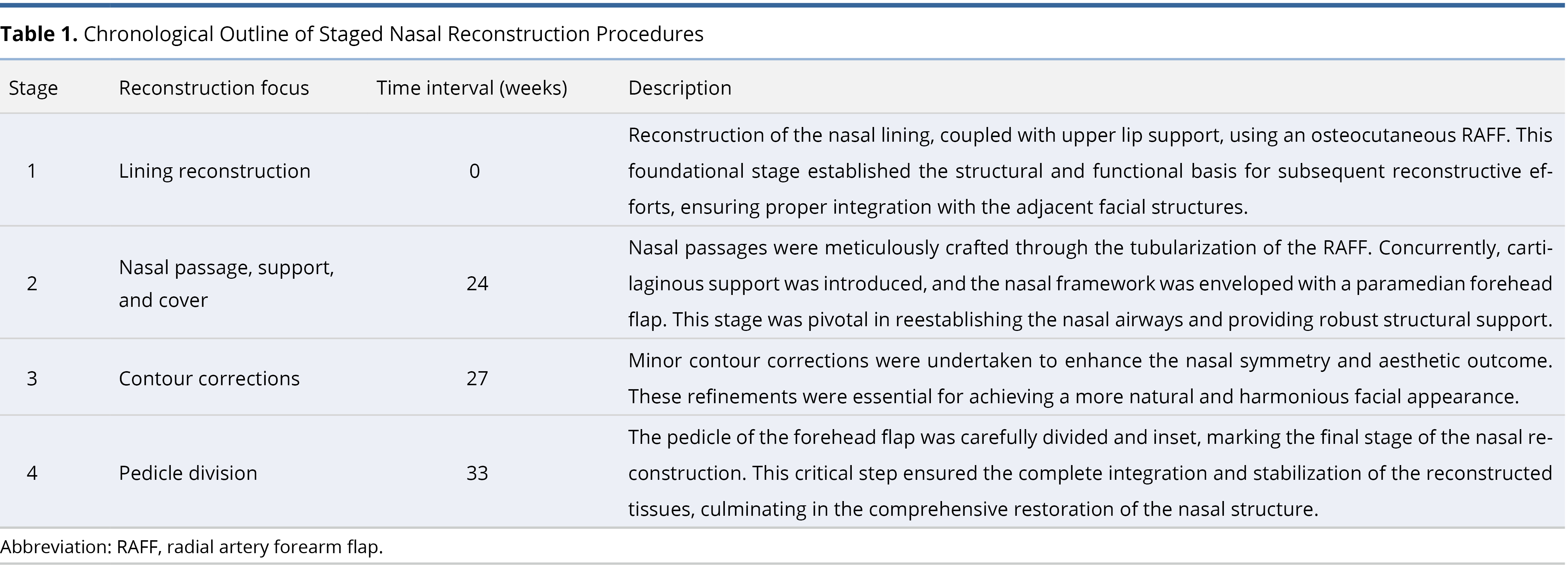
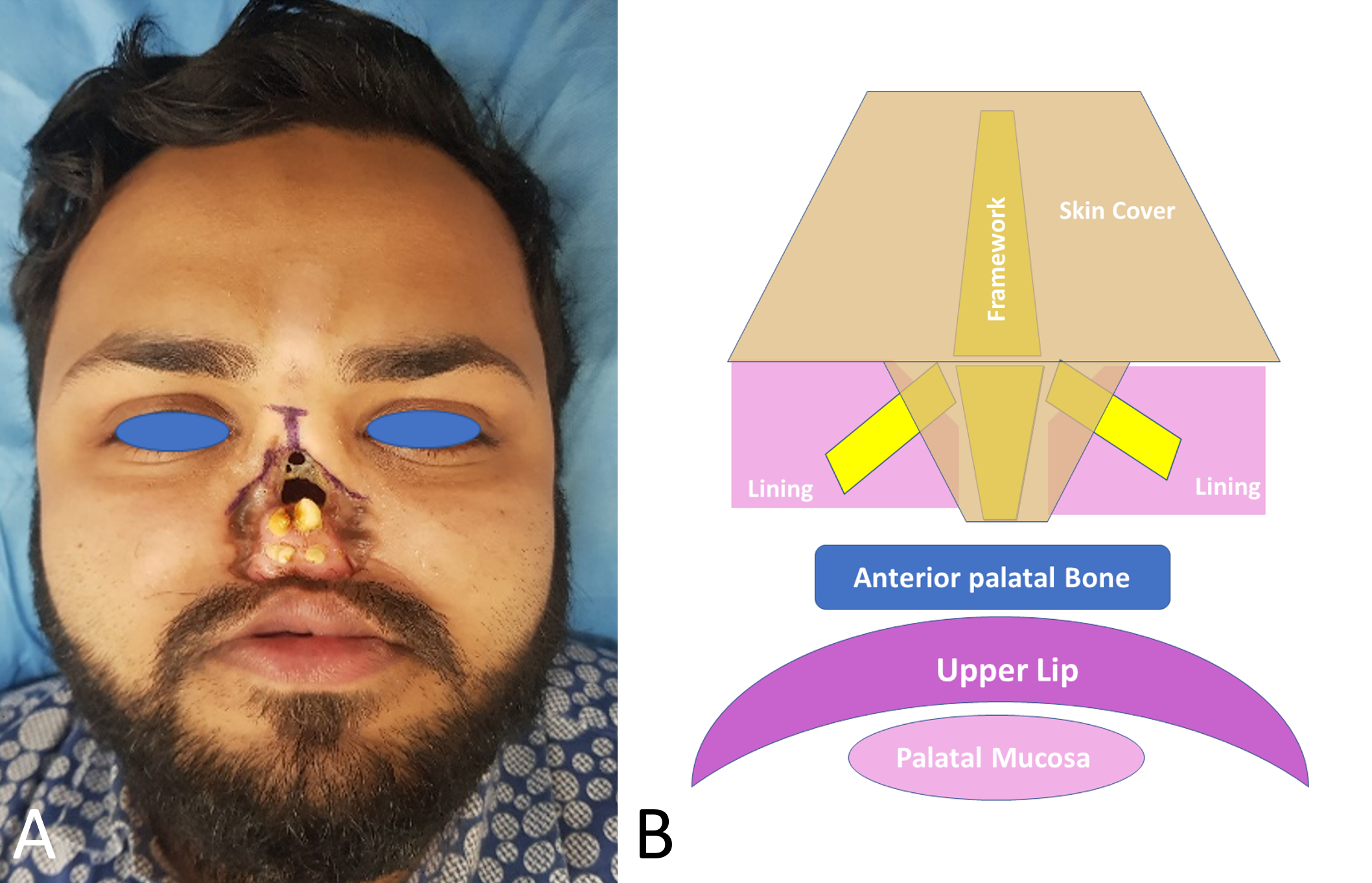
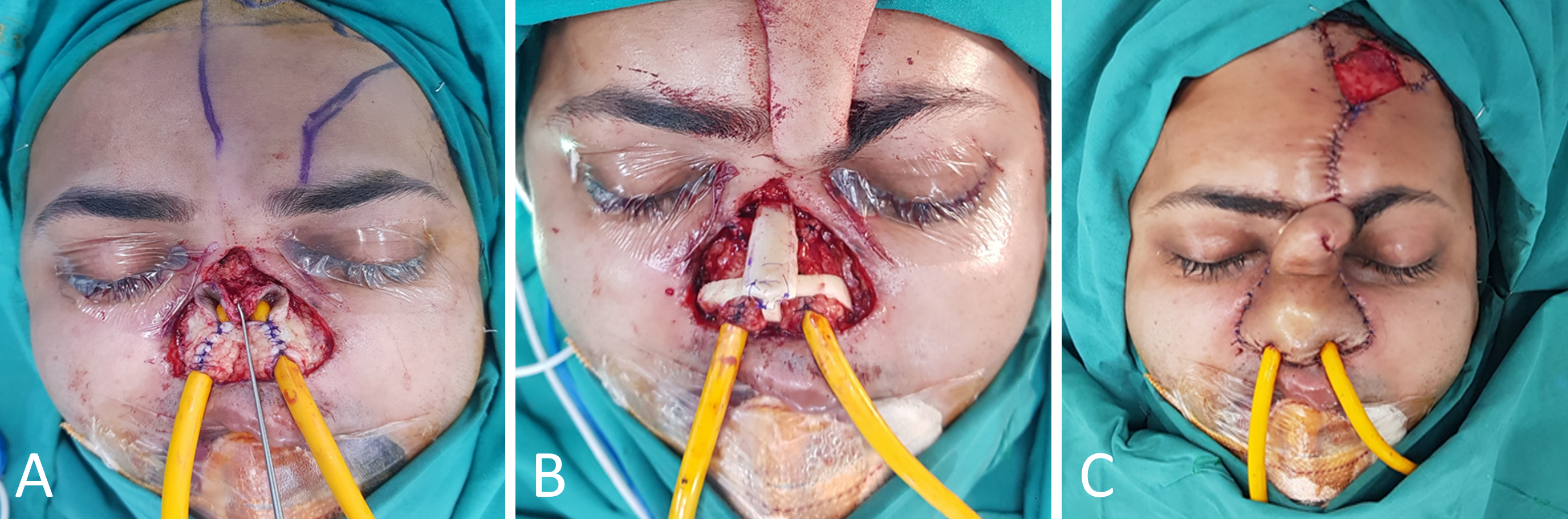
Under anesthesia, all scar tissue was meticulously excised to prepare for the reconstruction (Figure 2A). The septum was found to be absent, resulting in the nasal cavity being a single passage. An osteo-fasciocutaneous RAFF was harvested (Figure 2B). The cephalic vein was included in the flap to ensure adequate vascular supply.
The harvested flap was utilized in two distinct ways: the lateral 2 cm of the flap was used to create the palatal mucosa covering the radius bone, and the medial part of the flap was used to form the nasal lining. Additionally, a 0.5 cm strip of the flap was de-epithelialized to form the superior gingivobuccal sulcus. The pedicle of the flap was tunneled subcutaneously, and the vessels were anastomosed to the facial artery, facial vein, and a tributary of the internal jugular vein in the left submandibular region.
An opening was made in the flap at the nasal passage to facilitate breathing (Figure 2C), and a nasal stent was placed to maintain this opening. The procedure was completed without any flap-related complications. The donor site on the forearm was grafted and splinted for three weeks to ensure proper healing.
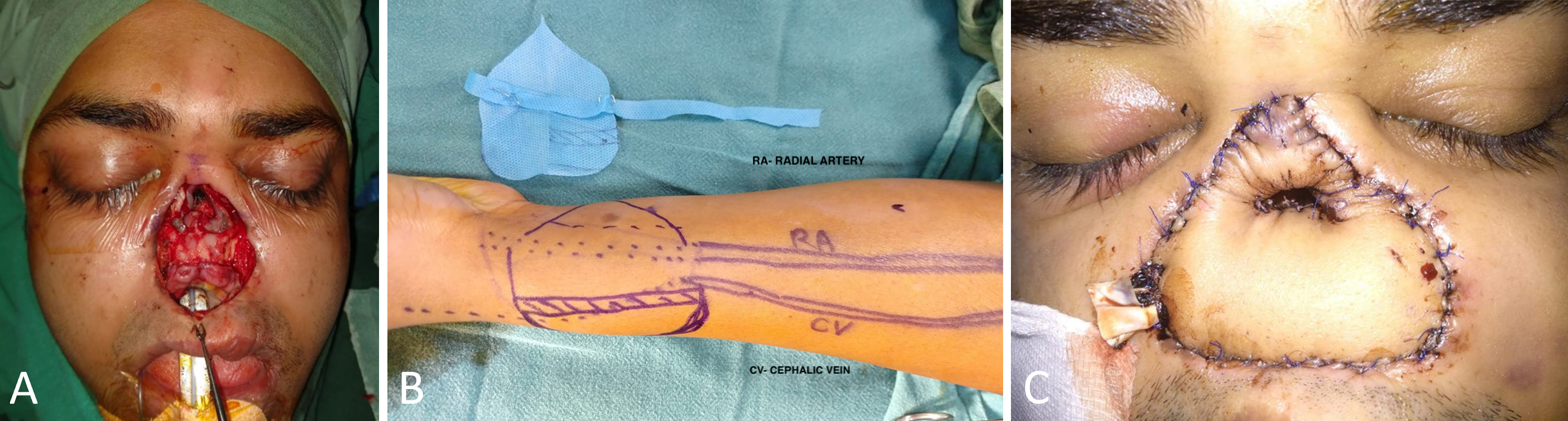
Figure 2. Intraoperative views during the first stage of nasal reconstruction using a tubularized radial artery forearm flap (RAFF). (A) View immediately following the excision of scar tissue, displaying the exposed nasal cavity prepared for RAFF placement. The nasal cavity appears as a single passage due to the absence of the septum. (B) Diagram showing the design and markings on the forearm for the osteo-fasciocutaneous RAFF, emphasizing the inclusion of the cephalic vein to ensure adequate vascular supply. (C) Postoperative view following the first stage of reconstruction, showing the correctly positioned RAFF with completed anastomoses to the facial artery, facial vein, and a tributary of the internal jugular vein. An opening for breathing was created to maintain the patency of the nasal passage.
Stage 2: Nasal Passage, Support, and Cover
Six months subsequent to the initial procedure, the second stage of nasal reconstruction was initiated. This phase involved the strategic placement of two 18 French catheters through the opening of the nasal cavity, serving as stents for the nascent nasal passages. To accommodate these structures, the flap was incised to a partial thickness (Figure 3A).
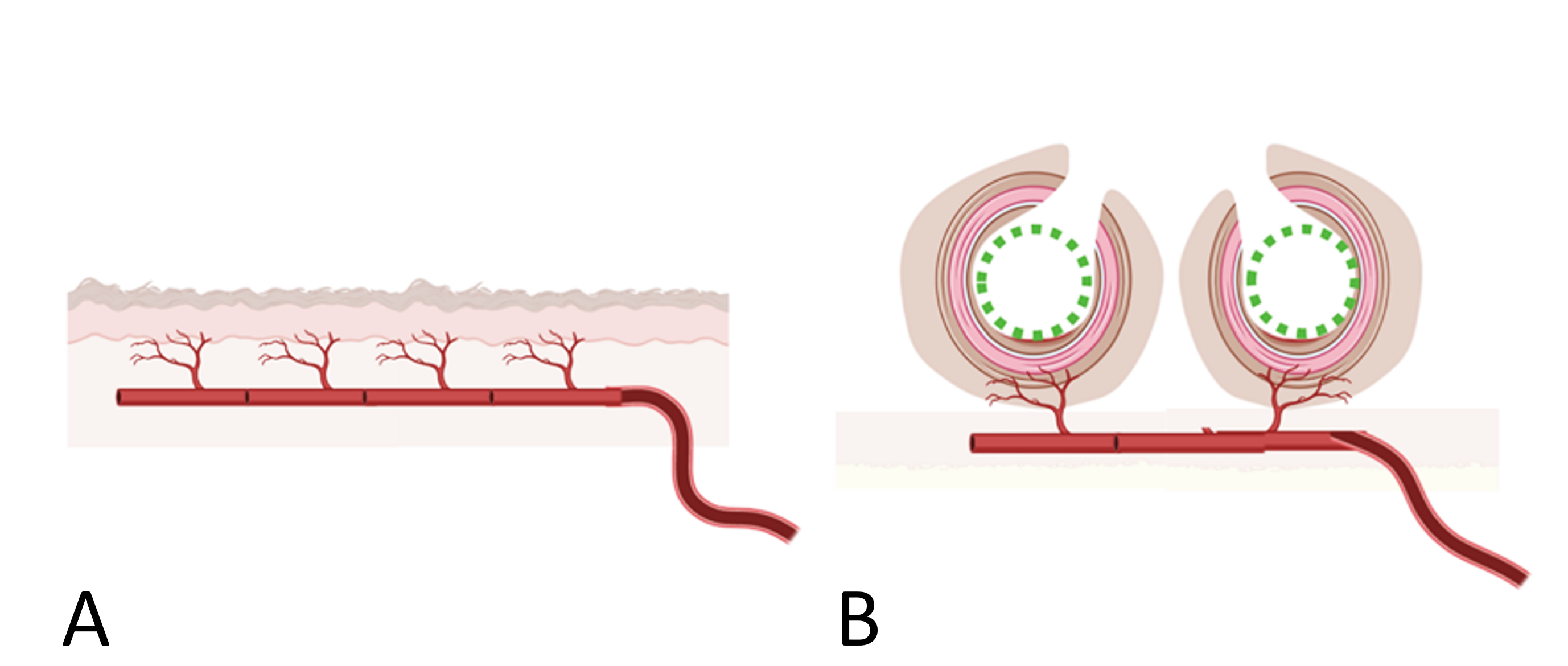
Figure 3. Application of tubularized radial artery forearm flap (RAFF) in the second stage. (A) Diagram illustrating the RAFF in its original flat configuration, highlighting the ladder-like distribution of perforators along the pedicle vessel axis. (B) Detailed view of the RAFF tubularization process to form two distinct nasal passages. The flap is meticulously wrapped around an 18 French Foley catheter, ensuring structural integrity and preventing collapse during the initial healing phase.
The skin, along with underlying subcutaneous tissue, was meticulously shaped around these catheters, effectively forming two distinct nasal channels. These were lined with RAFF epithelium to ensure an effective lining (Figures 3B, 4A).
Following this, a framework of costal cartilage was sculpted, providing essential structural support for the nose (Figure 4B). This framework was precisely engineered based on standard nasofrontal and nasolabial angle measurements obtained from cephalograms, with templates guiding the meticulous carving and placement of the cartilage. A paramedian forehead flap was fashioned and applied to the nasal structure (Figure 4B). This flap contributed an extra layer of integration, blending the newly formed nasal passages with adjacent facial features (Figure 4C).
To maintain the patency and functionality of these passages throughout the healing period, customized silicone nasal splints were utilized for three months. These devices were crucial in preventing the collapse of the structural channels, thus preserving airflow and ensuring the integrity of the surgical enhancements. The deployment of these splints was pivotal in achieving outcomes that were both aesthetically pleasing and functionally robust.

Figure 4. Intraoperative views during the second stage of nasal reconstruction using a tubularized radial artery forearm flap (RAFF) and a forehead flap. (A) Display of the tubularized RAFF using 18 French catheters as stents to sculpt and stabilize the newly formed nasal passages. The skin, along with some subcutaneous tissue, is meticulously molded around the catheters, forming two distinct nasal channels. These channels are lined with RAFF epithelium, ensuring structural stability and the integrity of the nasal lining during the second stage of reconstruction. (B) The cartilaginous framework is meticulously planned based on nasofrontal and nasolabial angle measurements obtained from cephalograms, ensuring anatomical precision. Following this planning, a costal cartilage framework is installed to provide essential structural support for the nasal reconstruction. This element is crucial for maintaining both the integrity and aesthetic alignment of the reconstructed nose. (C) Display of the paramedian forehead flap application during the second stage of nasal reconstruction. This phase showcases the final application of the forehead flap, completing the external coverage, encapsulating the previously positioned tubularized RAFF, and integrating it with the facial anatomy to finalize the reconstruction.
Stage 3: Contour Corrections
Three weeks following the forehead flap procedure, minor contour corrections were implemented to refine the nasal shape and enhance symmetry. These adjustments entailed precise reshaping of the nasal framework, aimed at producing a more natural and aesthetically pleasing appearance. The corrections specifically targeted irregularities and asymmetries that had emerged post-initial reconstruction, meticulously refining the nasal contour to better align with the facial features.
This stage proved critical in achieving a final result that successfully restored both functional and aesthetic qualities. Through diligent modifications to the nasal framework, the surgical team ensured that the reconstruction met the requisite functional and aesthetic standards, markedly enhancing patient satisfaction with the outcome.
Stage 4: Pedicle Division
Six weeks following minor contour corrections, the pedicle of the forehead flap was divided and set into its final position. This critical procedure involved meticulously detaching the flap from the donor site and securing it precisely to form the desired nasal structure. To ensure the newly formed nasal passages remained open and functional, nasal splints were maintained for an additional three months, safeguarding against any potential collapse or obstruction during the crucial healing phase. This stage was essential for the stabilization and final integration of the reconstructed nasal tissues, pivotal in concluding the reconstruction process effectively.
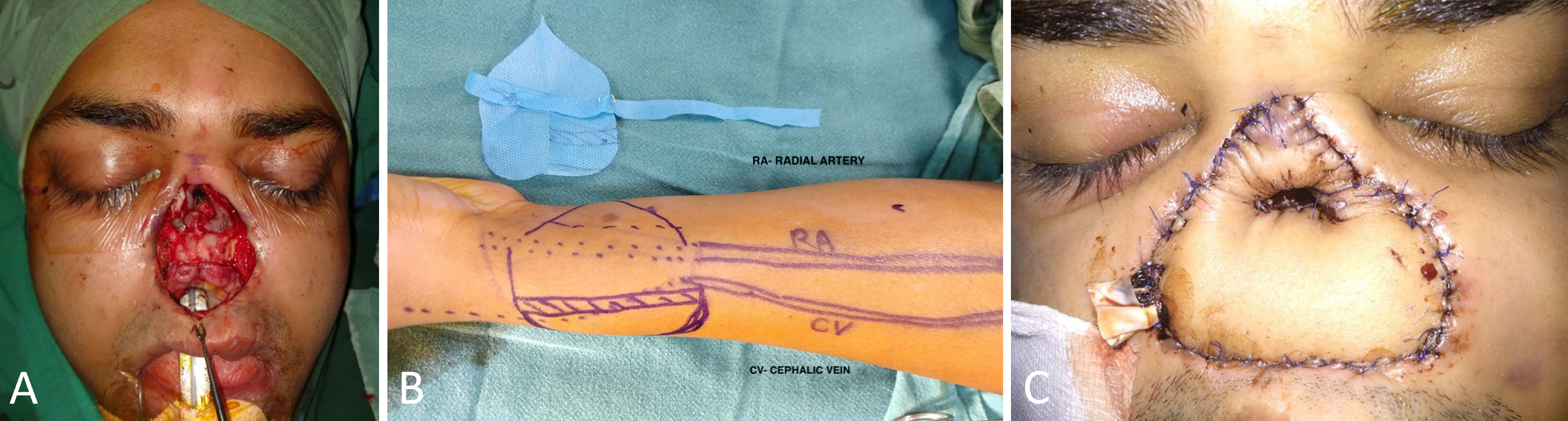
Figure 5A presents the frontal view of the patient six months post-operatively, following the completion of all stages of nasal reconstruction utilizing the tubularized RAFF technique. By this phase, the forehead flap pedicle had been divided and inset, reflecting a fully healed and substantially restored nasal structure. The nasal passages remained patent without any signs of collapse, contributing to a symmetrical and aesthetically pleasing nasal contour.
Six weeks post the final stage of nasal reconstruction using the tubularized RAFF technique, nasal endoscopy assessed the patency and function of the nasal passages. A follow-up at two years, documented in Video 1, confirmed their sustained openness and functionality, highlighting the enduring success of the surgical intervention. Further visual evidence from this assessment is provided in Video 1, available at https://doi.org/10.24983/scitemed.imj.2024.00189.
Video 1. Nasal endoscopy conducted two years after the final stage of nasal reconstruction using the tubularized radial artery forearm flap (RAFF) technique. This video illustrates the sustained patency and functionality of the nasal passages, affirming the long-term success of the surgical intervention in preserving clear and unobstructed airways.
A three-dimensional reconstructed computed tomography scan of the skull, conducted six months after surgery, confirmed successful bone healing and integration in the central maxilla (Figure 5B). The scan revealed that the radius bone was well-integrated with adjacent bone structures, showcasing stable and effective integration. This effective integration is pivotal for the long-term functionality and stability of the nasal architecture.
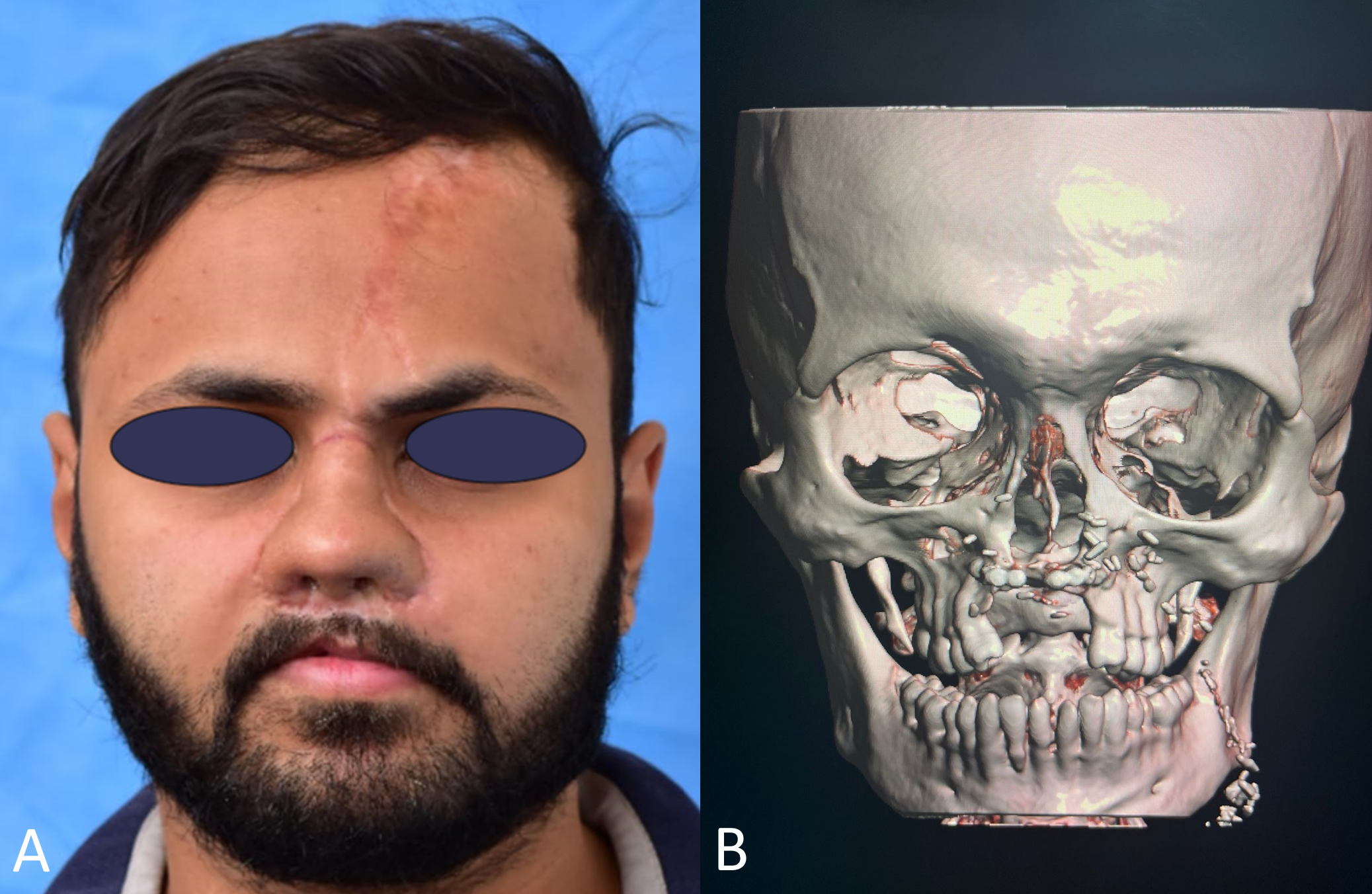
Figure 5. Postoperative outcomes and computed tomography evaluation six months following the completion of all stages of nasal reconstruction utilizing the tubularized radial artery forearm flap (RAFF) technique. (A) After the division and inset of the forehead flap pedicle, the patient exhibits well-healed surgical sites and a symmetrical nasal structure. This view captures the results following the completion of all nasal reconstruction stages, with the forehead flap pedicle seamlessly integrated and without visible complications. (B) A three-dimensional reconstructed computed tomography scan of the skull demonstrates the successful integration of the radius bone into the central maxilla, confirming stable bone healing and the absence of complications in the reconstructed nasal and maxillary structures.
Efficacy of Tubularized RAFF Technique
The study focuses on a 27-year-old man who underwent a four-stage nasal reconstruction using the tubularized RAFF technique to address a total nasal defect. Postoperative evaluations confirmed that the nasal passages remained open and that bone grafts integrated seamlessly without any flap-related complications. These outcomes significantly improved both functional and aesthetic aspects of the nose, substantially enhancing the patient’s quality of life.
This research provides robust evidence supporting the efficacy of the tubularized RAFF technique in managing complex nasal reconstructions. It demonstrates the technique’s ability to effectively tackle both functional and aesthetic challenges in severe cases, highlighting its value in facial reconstructive surgery.
Strategies for Free Flap Selection
Successful reconstruction of the nose, a complex three-dimensional structure, necessitates a profound understanding of its anatomy. Functional and aesthetically pleasing outcomes in nasal reconstruction present significant challenges, particularly in cases of total nasal defects. The complexity of these procedures is further exacerbated by the loss of adjacent tissue, complicating the restoration process.
In cases involving nasal defects accompanied by the loss of adjacent tissue, autologous reconstruction using free flaps often becomes the only viable option due to the scarcity of local tissue options. Various free flaps, such as the RAFF, temporoparietal flap, and anterolateral thigh flap, are commonly used in these intricate reconstructions. Other options, including dorsal metacarpal flaps, osteocutaneous femur flaps, posterior auricular flaps, and fascial flaps, may also be employed based on the specific demands of each case [5].
For subtotal or complete nasal defects, prefabricated scalping and forehead flaps have been valuable, providing additional versatility and support for reconstructive efforts [6]. These techniques facilitate the comprehensive restoration of both form and function, effectively addressing the multifaceted challenges inherent in three-dimensional nasal reconstruction.
RAFF Techniques for Nasal Reconstruction
The RAFF is a versatile option for reconstructing the entire nose, applicable either in a single-stage procedure or through a multi-staged approach where a forehead flap serves as the external cover. For extensive nasal defects, the traditional technique involves folding the RAFF in two planes to reconstruct the nasal vault, columella, floor, and external cover, thereby enabling a thorough reconstruction of the nasal structure.
In the initial stage, the strategic placement of a primary dorsal cartilage graft between the folded layers of the RAFF enhances both the structural support and the anatomical form of the nasal framework, as detailed in previous studies [7]. When addressing adjacent tissue defects, local flaps or de-epithelialized sections of the same flap are utilized, tailored to address these specific challenges and ensure a reconstruction that harmonizes functionality with aesthetic appeal [4].
In nasal reconstruction, the RAFF is recognized for effectively blending essential structural and aesthetic elements. This technique ensures that the reconstructed nasal framework is both durable and visually appealing, meeting the stringent criteria required in advanced facial reconstructive procedures.
Challenges With Traditional RAFF Technique
The traditional RAFF technique often falls short in managing extensive nasal reconstructions due to the complexity of defects encountered. In this case, the patient exhibited a substantial nasal defect compounded by significant damage to palatal mucosa and bone structures. Complications were further exacerbated by a superiorly displaced pyriform aperture and a misaligned anterior alveolus, adding to the reconstruction challenges.
Furthermore, addressing a vestibulo-nasal fistula and establishing a stable nasal lining presented formidable challenges with the conventional RAFF method. To counter these issues, the surgical plan incorporated bony reconstruction of the alveolus and meticulous scar tissue removal. This strategic approach adheres to Menick’s principle, emphasizing that nasal reconstructions built on an unstable foundation are prone to yielding suboptimal results [8].
In response to these foundational structural issues, we implemented the tubularized RAFF technique, specifically designed to restore functionality and enhance aesthetic outcomes. This modified approach proved effective, ensuring a stable and satisfactory reconstruction.
Tubularized RAFF for Nasal Reconstruction
The RAFF is classified as a type C flap, distinguished by its ladder-type distribution of perforators along the pedicle vessel axis (Figure 3A) [9]. This unique vascular architecture enables segmentation of the flap into multiple paddles, enhancing its versatility for complex nasal reconstructions. In this instance, the unique anatomy of the RAFF was employed to create tubularized sections that formed the nasal passages, which were temporarily supported by splints to maintain structural integrity (Figure 3B).
Given the restricted dimensions of the pyriform aperture and the absence of a nasal passage, a simple superstructure reconstruction was inadequate. The creation of skin-lined tubes faced challenges due to their natural tendency to contract and potentially collapse [10]. To counteract this, the flap was meticulously thickened to 0.8 mm and expanded by an additional 10% to compensate for potential shrinkage. This modified flap was then securely wrapped around an 18 French Foley catheter, which was maintained as a stent for six weeks to ensure structural stability and prevent collapse.
Following the initial stenting phase, the Foley catheter was replaced with silicone stents, retained for three more months to safeguard the structural integrity of the nasal passages. This strategic measure was critical to prevent the collapse of the nascent structures, thereby ensuring the functional efficacy and structural stability of the reconstruction.
Importance of Nasal Skeletal Framework
The nasal skeletal framework is essential for providing the structural integrity, projection, and contour that are vital for both the functional and aesthetic aspects of the nose. Materials such as cartilage or bone are typically used to achieve these critical features [11]. In the case described, costal cartilage was selected for its ease of harvest and proven reliability in previous applications. This cartilage was meticulously crafted into key structural components, including the dorsal nasal strut, columellar strut, and alar support grafts, ensuring the nasal structure was both stable and visually pleasing.
Challenges in Addressing Unresolved Nasal Stuffiness
Prior to surgical intervention, the patient experienced chronic nasal stuffiness, a symptom potentially indicative of empty nose syndrome [12]. Empty nose syndrome develops when extensive damage to the nasal turbinates impairs their regulatory functions in airflow and air humidification. Characteristically, empty nose syndrome manifests as a paradoxical feeling of excessive nasal openness coupled with inadequate air intake, which can result in dryness, burning sensations, and a persistent feeling of suffocation despite seemingly unobstructed nasal passages. The fundamental problem in empty nose syndrome involves the disruption of “cool air” receptors and a loss of nerve fibers essential for airflow detection. This alteration undermines the critical feedback mechanism for sensing airflow, leading to perceived blockages and profoundly affecting quality of life.
Despite surgical efforts to correct the nasal structure, the issue of stuffiness persisted postoperatively. This ongoing challenge could be due to the absence of sensory restoration in the reconstructed flap, affecting airflow perception and maintaining the sensation of stuffiness even after anatomical adjustments. Other postoperative structural changes or healing processes might also alter airflow experience, contributing to persistent nasal congestion.
Exploring surgical interventions to reconstruct or simulate the functions of the turbinates could be beneficial, especially in complex cases like this. However, fully mimicking the intricate functionality of natural turbinates is extremely challenging due to their complex structure and the delicate balance required for proper airflow and sensory feedback. Further advancements in surgical techniques and materials are necessary to improve functional and aesthetic outcomes, potentially including strategies to address turbinate dysfunction in conditions like empty nose syndrome.
Study Limitations
This study was based on a single case with a relatively short-term follow-up. A longer follow-up is necessary to fully assess the effectiveness of this procedure. Additionally, the potential relationship between associative factors, such as allergies and seasonal variations, and persistent nasal stuffiness should be further investigated.
This study presents the innovative tubularized RAFF technique for nasal reconstruction, a method not previously described in the literature. This technique has shown considerable promise, particularly in addressing total nasal defects that pose complex structural challenges beyond the scope of traditional methods. It successfully preserved the patency of nasal passages while meeting both functional and aesthetic objectives. Despite its effectiveness, the study observed some postoperative issues, including persistent nasal stuffiness and lack of sensation in the reconstructed flap. These findings underscore the need for further research and extended follow-up studies to fully assess and refine the technique’s efficacy and adaptability. Advancing this technique could potentially establish it as a preferred method for managing intricate nasal reconstructions.
Received date: November 30, 2023
Accepted date: August 01, 2024
Published date: September 02, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)’ autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Video 1. Nasal endoscopy conducted two years after the final stage of nasal reconstruction using the tubularized radial artery forearm flap (RAFF) technique. This video illustrates the sustained patency and functionality of the nasal passages, affirming the long-term success of the surgical intervention in preserving clear and unobstructed airways.
The senior author (Dr. Isao Koshima) designed a tibial osseo-periosteal (TOP) flap. TOP flap has a favorable anatomical position with a thin skin around it, hence it is a good option for an island flap. TOP flap can be used for various mild to moderately sized osteo-cutaneous defects with low morbidity. In this article, the authors describe their experience of the first reported cohort of TOP flaps in clinical practice.
Smartphones and cellular technology have revolutionized flap monitoring. Smartphones provide low-cost thermal imaging alternatives to flap monitoring. It remains unclear, however, whether this method is accurate or reliable. It may be challenging to use smartphone thermal imaging when clinicians fail to communicate clinically relevant events. The authors demonstrate three instances in which the thermal imaging information on smartphones was misleading. Each case is analyzed to determine how clinical decisions should be made.
The likelihood of donor site ischemia following the harvesting of a fibula flap is extremely low, but it is potentially lethal if it occurs. The authors describe a case of ischemia of the lower extremity following a free fibula harvest for head and neck reconstruction. The authors discuss preoperative, intraoperative, and postoperative strategies to assist in diagnosing and managing risks associated with free fibula flap harvesting in this paper.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
A significant increase in peripheral nerve surgery has occurred in recent years due to improvements in surgical techniques. In most reconstructive procedures, sensory restoration is frequently neglected in preference to restoring motor function. Along with increasing the risk of developing injuries to the body, patients who lose protective sensations are more likely to develop neuropathic pain and depression, which adversely affect their quality of life. As regaining sensory function is important, the study examines a variety of techniques that may be useful for restoring sensory function across various body parts.
This article presents a crucial case report on potential wound healing complications linked to fremanezumab, a calcitonin gene-related peptide-targeting antibody for migraine prevention. It documents the first known instance of delayed wound healing following a free flap breast reconstruction, underscoring the need for heightened clinical vigilance and individualized patient assessment in perioperative settings. Highlighting significant safety data gaps, the report advocates for comprehensive research and rigorous post-marketing surveillance. The findings emphasize the importance of balancing the risks of delayed wound healing with the need for effective disease control, especially when using biologic agents for chronic conditions. This article is essential for medical professionals managing patients on biologic therapies, offering critical insights and advocating for a personalized approach to optimize patient outcomes. By presenting novel observations and calling for further investigation, it serves as a vital resource for enhancing patient care and safety standards in the context of biologic treatments and surgical interventions.
This manuscript showcases an advanced surgical approach for treating malignant giant cell tumor of bone, emphasizing precision and ethical considerations. It leverages innovative pedicled flap technologies, as opposed to free flaps, enhancing limb functionality and patient quality of life. This technique equips surgeons with evidence that tailored surgical strategies can significantly improve outcomes in complex cases. The paper discusses technical challenges and highlights the application of supercharging and superdrainage techniques in limb reconstructions, methods well-established in microsurgery but infrequently used in oncological contexts. These techniques are crucial for optimizing flap viability and ensuring surgical success. Additionally, the manuscript underscores the profound impact of these advancements on patient lives, offering hope and showcasing tangible benefits. This narrative, blending scientific analysis with patient stories, enriches the understanding of limb reconstruction innovations in oncological surgery, making it invaluable for surgeons.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
The likelihood of donor site ischemia following the harvesting of a fibula flap is extremely low, but it is potentially lethal if it occurs. The authors describe a case of ischemia of the lower extremity following a free fibula harvest for head and neck reconstruction. The authors discuss preoperative, intraoperative, and postoperative strategies to assist in diagnosing and managing risks associated with free fibula flap harvesting in this paper.
This manuscript showcases an advanced surgical approach for treating malignant giant cell tumor of bone, emphasizing precision and ethical considerations. It leverages innovative pedicled flap technologies, as opposed to free flaps, enhancing limb functionality and patient quality of life. This technique equips surgeons with evidence that tailored surgical strategies can significantly improve outcomes in complex cases. The paper discusses technical challenges and highlights the application of supercharging and superdrainage techniques in limb reconstructions, methods well-established in microsurgery but infrequently used in oncological contexts. These techniques are crucial for optimizing flap viability and ensuring surgical success. Additionally, the manuscript underscores the profound impact of these advancements on patient lives, offering hope and showcasing tangible benefits. This narrative, blending scientific analysis with patient stories, enriches the understanding of limb reconstruction innovations in oncological surgery, making it invaluable for surgeons.
The case highlights a sophisticated total nasal reconstruction technique employing a tubularized radial artery forearm flap (RAFF), which represents a modified approach compared to the traditional RAFF method. This approach stands out due to its intricate design, aimed at addressing the challenge of restoring both the nasal structure and internal lining, potentially leading to enhanced outcomes in terms of appearance and functionality. Its suitability for publication is based on its valuable contribution to the medical field by introducing an alternative technique that has the potential to influence future practices in nasal reconstruction surgeries. This case can serve as an educational resource for surgeons in this field. However, there are specific issues that need to be addressed before it can be published in its current state.
I enjoyed reading the article on the approach to total nasal structural defects, especially in terms of reconstructing the inner lining and osteocartilaginous skeleton. It was enlightening to see how the work proposes subtle variations in the steps of establishing the inner liner, referencing radial forearm free flap (RFFF) tabularization, and how it thoughtfully integrates techniques that are well-established in the field. Moreover, the article builds upon Menick's substantial research in a particular fashion. I offer a few observations and thoughts that could enhance the quality of this work.
This article presents a nasal reconstruction technique for total nasal defects, addressing their significant physical impact. It showcases a case study of a patient with mucormycosis-induced nasal loss, highlighting the transition from social embarrassment to restoration. The use of a tubularized radial artery forearm flap (RAFF) for reconstruction demonstrates surgical expertise. While the article is promising, certain aspects require further refinement. In summary, I believe it deserves publication because this RAFF approach holds the potential to establish itself as the preferred method for addressing difficult cases characterized by total nasal defects and concomitant structural challenges. It offers a promising avenue for restoring both form and function.
Chandrasekar S, Tiwari R, Singhal M. Innovative tubularized radial artery forearm flap technique for comprehensive reconstruction of total nasal and anterior palatal defects: A case study. Int Microsurg J 2024;8(2):1. https://doi.org/10.24983/scitemed.imj.2024.00189