We report herein a case of cholesteatoma of the right temporal bone that mimicked facial neurinoma. A 44-year-old woman complained of right facial nerve paralysis. Computed tomography (CT) scan showed a lesion along the right facial nerve of the labyrinthine and horizontal portion. The lesion widened to the right fallopian canal at that site. She underwent surgery and both surgical and histological findings were consistent with cholesteatoma. In contrast to the CT scan findings, which strongly suggested the lesion to be facial neurinoma, the diffusion-weighted magnetic resonance imaging (MRI) suggested cholesteatoma.
Facial nerve schwannoma, or facial neurinoma, is an uncommon disease that accounts for less than 1% of temporal bone tumors [1]. The age of presentation reportedly varies. It occurs at all age ranges, from children to elderly, and no gender prediction is seen [1]. Facial neurinoma commonly presents with peripheral facial palsy and hearing loss (conductive or sensorineural) and occasionally dizziness, tinnitus, and other otologic symptoms.
Cholesteatoma is a mass composed of keratinizing epithelium occurring in the middle ear. Cholesteatoma can be divided into 2 types: acquired and congenital. The acquired type of cholesteatoma originates as an inward growth of the tympanic membrane. Cholesteatoma extending to the petrous portion of the temporal bone is relatively uncommon [2]. CT scan is usually used for preoperative diagnosis of the cholesteatoma. If the diagnosis is suspicious, magnetic resonance imaging (MRI) enhanced with Gadolinium (Gd) is often performed.
We report herein a case of cholesteatoma of the skull base of the middle cranial fossa. The lesion extended along the facial nerve and mimicked facial neurinoma.
A 44-year-old woman presented with a history of mild right facial palsy (4 years) and right hearing loss (10 years). She had first noticed the mild facial palsy (House-Brackmann grade II) of the right side 4 years ago. Her facial palsy suddenly progressed (House-Brackmann grade III) one month before presentation at our hospital. She denied any history of right otorrhea and there was no history of ear pain or headache.
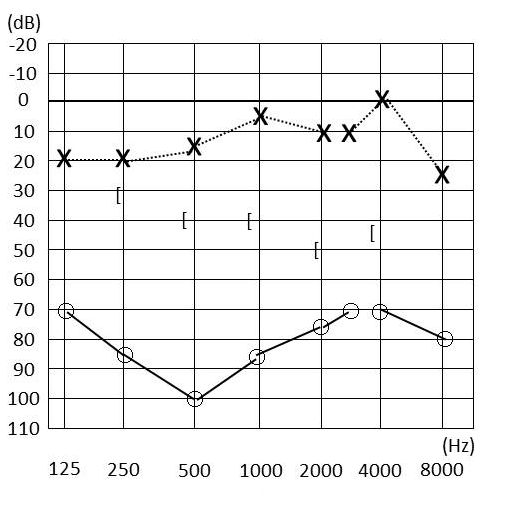
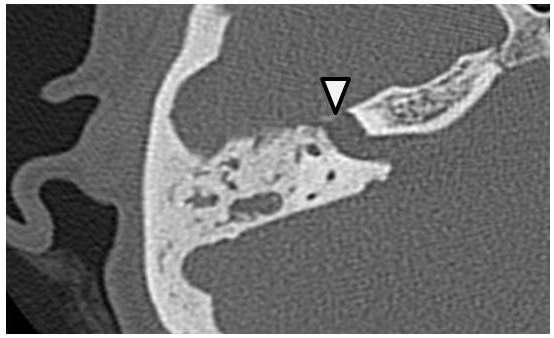
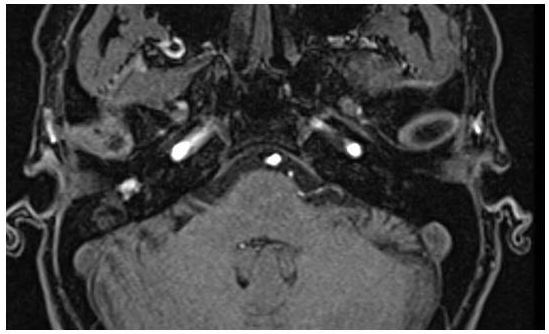
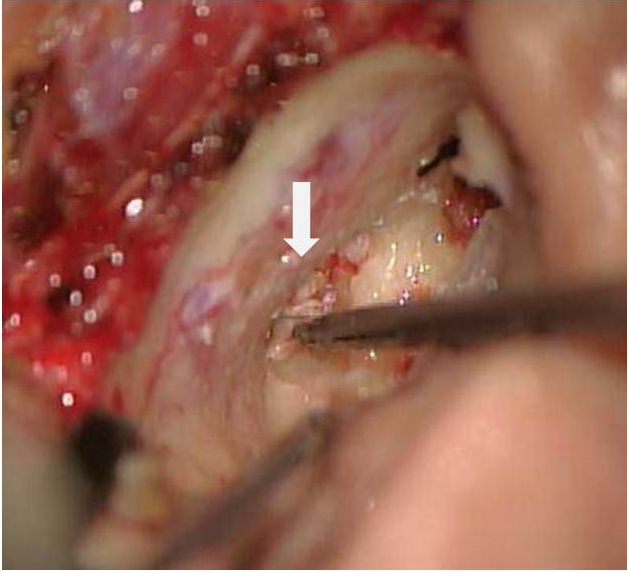
Physical examination of the right ear revealed a dry retraction pocket at the pars flaccida, and the left ear showed no abnormality. Pure tone audiometry showed mixed hearing loss of the right ear (Figure 1). Computed tomography (CT) scan of the temporal bone revealed a soft tissue density along the right facial canal extending from the horizontal to labyrinthine portion (Figure 2). MRI showed the mass to be enhanced with gadolinium (Figure 3). Diffusion-weighted MRI detected the lesion as a high-intensity mass (Figure 4). Exploratory tympanotomy was done. Intraoperatively, a whitish mass was found along the right facial nerve after drilling out the horizontal and labyrinthine portions of the nerve (Figure 4). All cholesteatoma lesion of the petrous bone was removed via translabyrinthine approach. The postoperative pathological findings were also consistent with cholesteatoma (Figure 5). The postoperative course was uneventful, but her facial palsy did not improve after the surgery.
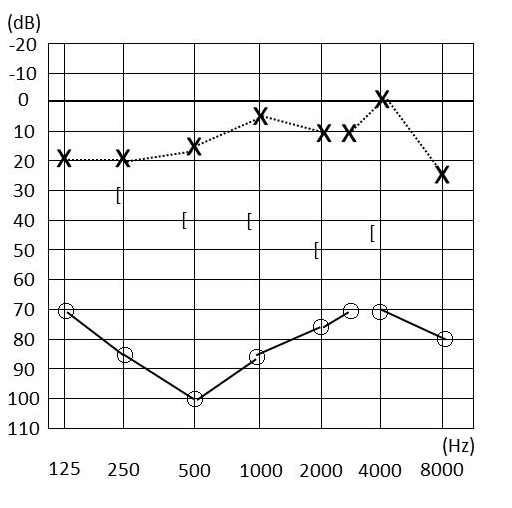
Figure 1. Pre-operative pure-tone audiogram. The audiogram showed mixed hearing loss of the right ear.
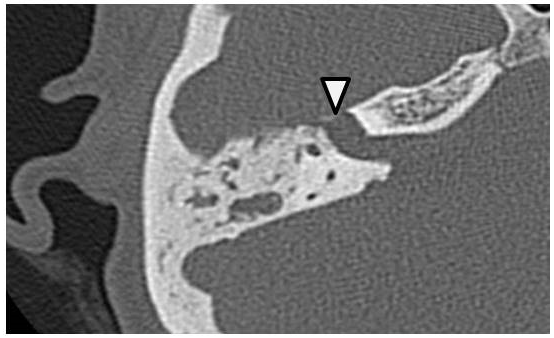
Figure 2. CT scan of the right temporal bone. Facial canal was widened by the lesion (arrowhead).
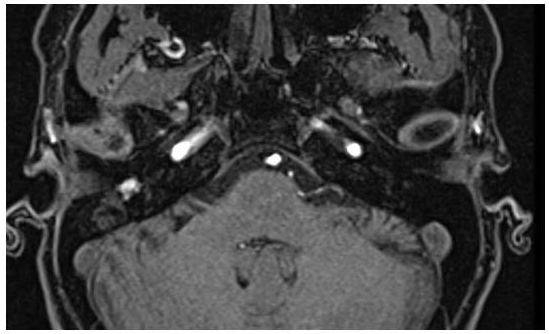
Figure 3. Gadolinium-enhanced T1 weighted MRI. A part of the lesion was well enhanced by gadolinium.

Figure 4. Diffusion-weighted MRI. The lesion was detected as a high-intensity mass (arrowhead).
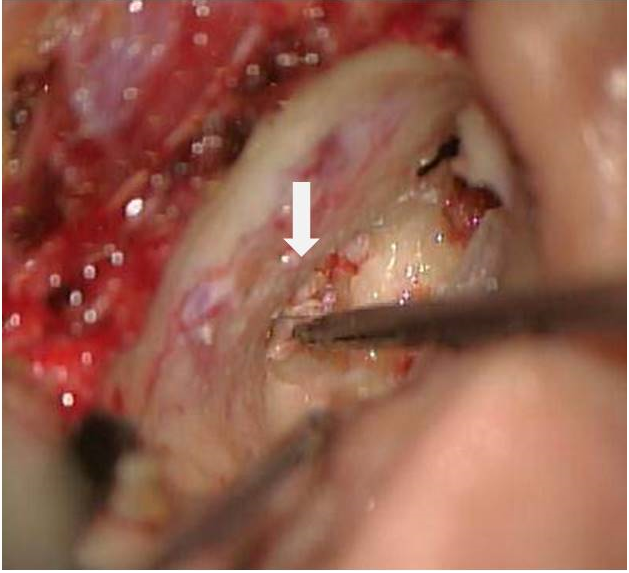
Figure 5. The operative finding. Whitish cholesteatoma pearl was noticed. The lesion was removed via translabyrinthine approach.
The geniculate ganglion fossa is the most common location for facial nerve neurinoma [3,4]. They have reported that facial neurinoma originating in the geniculate ganglion fossa often shows extension to the tympanic and/or labyrinthine segments and that isolated involvement of the geniculate ganglion fossa at the time of the presentation is very rare. They emphasized that facial neurinoma should be suspected whenever a middle cranial fossa mass is associated with facial nerve dysfunction and/or otologic symptoms.
Our patient exhibited with facial weakness and hearing loss of long duration and both these symptoms were often present with facial neurinoma. The location of the disease, as detected by CT scan and
In conclusion, we reported a case of cholesteatoma that mimicked facial neurinoma. To avoid confusion in such cases, diffusion-weighted MRI may be useful in preoperative differential diagnosis.
Received date: August 28, 2017
Accepted date: September 26, 2017
Published date: October 04, 2017
© 2017 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).

The present study demonstrated that TEES could be a satisfying alternative to traditional microscopic surgery for the management of congenital cholesteatoma, even in pediatric patients. However, one-handed surgery demands greater skill and requires more practice to achieve a good outcome.
Newly discovered epidemiological evidence linking cholesteatoma to depression suggests that routine screening and monitoring of psychological status among cholesteatoma patients is warranted. Policies aimed at the early detection and timely treatment of comorbid depression following diagnosis with cholesteatoma could enhance health promotion and disease prevention.
The author reports a case involving a 59-year-old man with delayed presentation of a huge mastoid cholesteatoma complicated by skull base erosion and cerebrospinal fluid leakage. Delayed presentation of this disease entity can have negative health consequences for patients. Regular otologic examinations, audiologic follow-up, and imaging examinations are viewed as the most effective strategies for the prevention of this type of situation. Early recognition of cholesteatomas is essential, as appropriate and timely treatment can prevent this rare comorbid condition from becoming fatal.
The authors report a case of otogenic Lemierre's syndrome in a male patient who presented with atypical symptoms and was subsequently treated aggressively with antibiotics and surgery. In this article, the authors demonstrate how they could have avoided serious complications by diagnosing and treating the patient earlier. The authors suggest key points that should be noted in clinical practice in order to prevent misdiagnosis or delayed diagnosis of Lemierre's syndrome.
The authors describe a 41-year-old man who suffered retraction-related complications that may have been missed or delayed. The present case illustrates the potential dangers associated with tympanic retraction pockets, despite the fact that their bottoms are clear and clean. The article discusses the reasons for the lack of consensus among otologists regarding the appropriate way to treat tympanic membrane retractions. There is further discussion regarding the challenges associated with early surgical intervention.
This study investigates the efficacy of conservative management using 5-fluorouracil (5-FU) for treating cholesteatoma in ambulatory care settings, offering an alternative for patients who prefer to avoid surgery. Over 13 years, 15 ears of 14 patients were treated with a 5% 5-FU cream and assessed using Takahashi's efficacy criteria. The results revealed positive outcomes, with 87% of cases deemed good and 13% as fair, with no poor evaluations. This approach may be suitable for specific populations, such as older adults and individuals in remote areas with limited access to specialized healthcare services.
This is an interesting case, which is easily misdiagnosed on the base of routine imaging examination. In the present report, the authors show that DWI MRI has a greater advantage on the precise diagnosis of cholesteatoma. The conclusion is of great guiding significance in otoneurosurgery.
It is an interesting case report. However, some important details are missing in this manuscript.
Introduction section: Please provide references of the first sentence and second paragraph.
ResponseReferences have been added.
Case Report section: Do you have information about tympanogram, acoustic reflex or any electrophysiological test? Is it possible to know more details about the surgical procedure? Any image? What about surgical results, postoperative evaluation and follow up?
ResponseWe did not conduct tympanometry, acoustic reflex test, and ABR. We conducted translabyrinthine approach to the petrous bone region. We have added the following sentences and figure 5. “All cholesteatoma lesion of the petrous bone was removed via translabyrinthine approach.” We have added the following sentence. “The postoperative course was uneventful, but her facial palsy did not improve after the surgery.”
The author has made the correction as suggested. It can be accepted for publication.
This article can be accepted for publication.
Tabuchi K, Hirose Y, Hara A. Cholesteatoma mimicking facial neurinoma: A case report. Arch Otorhinolaryngol Head Neck Surg 2017;1(3):2. doi:10.24983/scitemed.aohns.2017.00039