This paper describes a 41-year-old man with a tympanic retraction pocket, which may have led clinicians to miss or delay diagnosing retraction-related complications. The patient had aural fullness on the left side for several years. He did not report any hearing loss or otorrhea. During follow-up at a local clinic, a tympanic retraction pocket with a clean bottom was discovered, but no progression was observed. Nevertheless, due to an increase in symptoms, the patient was referred to our medical center for further investigation and treatment. The computed tomography examination of the left temporal bone revealed extensive scutum erosion and an expanding mass of soft tissue within the mastoid. This mass was later determined to be cholesteatoma after surgical and pathological examinations. A five-year follow-up did not reveal any recurrences. The present case illustrates that tympanic retraction pockets can be unsafe even when their bottoms are clear and clean. The article discusses the reasons for the lack of consensus among otologists regarding the optimal management strategy for tympanic membrane retractions. There is a further discussion of the challenges associated with early surgical intervention.
The tympanic membrane, commonly referred to as the eardrum, is a thin, cone-shaped membrane that separates the external ear from the middle ear. The tympanic membrane is composed of three tissue layers: the cutaneous layer (outmost), the fibrous layer (middle), and the mucosal layer (innermost) [1]. The tympanic membrane serves two primary functions: (1) protecting the middle ear from foreign bodies and infection; and (2) transmitting sound from the air to the ossicles within the middle ear.
Tympanic membrane retraction occurs when negative pressure within the middle ear causes the most pliant portions of the membrane to deflate [2]. This negative pressure may be induced by Eustachian tube dysfunction (hydrops ex-vacuo), repeated inflammation, dysfunction in epitympanic recess ventilation, habitual sniffing, or a mastoid of small volume [3-6]. The most common sites of retraction pockets are the pars flaccid and the postero-superior portions of the tympanic membrane [7].
Retraction pockets with clear and clean bottoms are generally regarded as “safe” or “stable”. However, in this report, we present a case of a tympanic retraction pocket that could cause clinicians to miss or delay diagnosis of retraction-associated complications.
A 41-year-old man presented with aural fullness on the left side, which had persisted for several years. The patient did not report hearing loss, otorrhea, earache, tinnitus, or vertigo, and had undergone regular otologic examinations (performed by a general practitioner using a pneumatic otoscope) over a period of several years. The tympanic membrane displayed a retraction pocket; however, there were no obvious signs of progression during years of follow-up. Nonetheless, following an increase in the intensity of symptoms, the patient was referred to the Department of Otolaryngology-Head and Neck Surgery at Taipei Veterans General Hospital for further investigation and management.
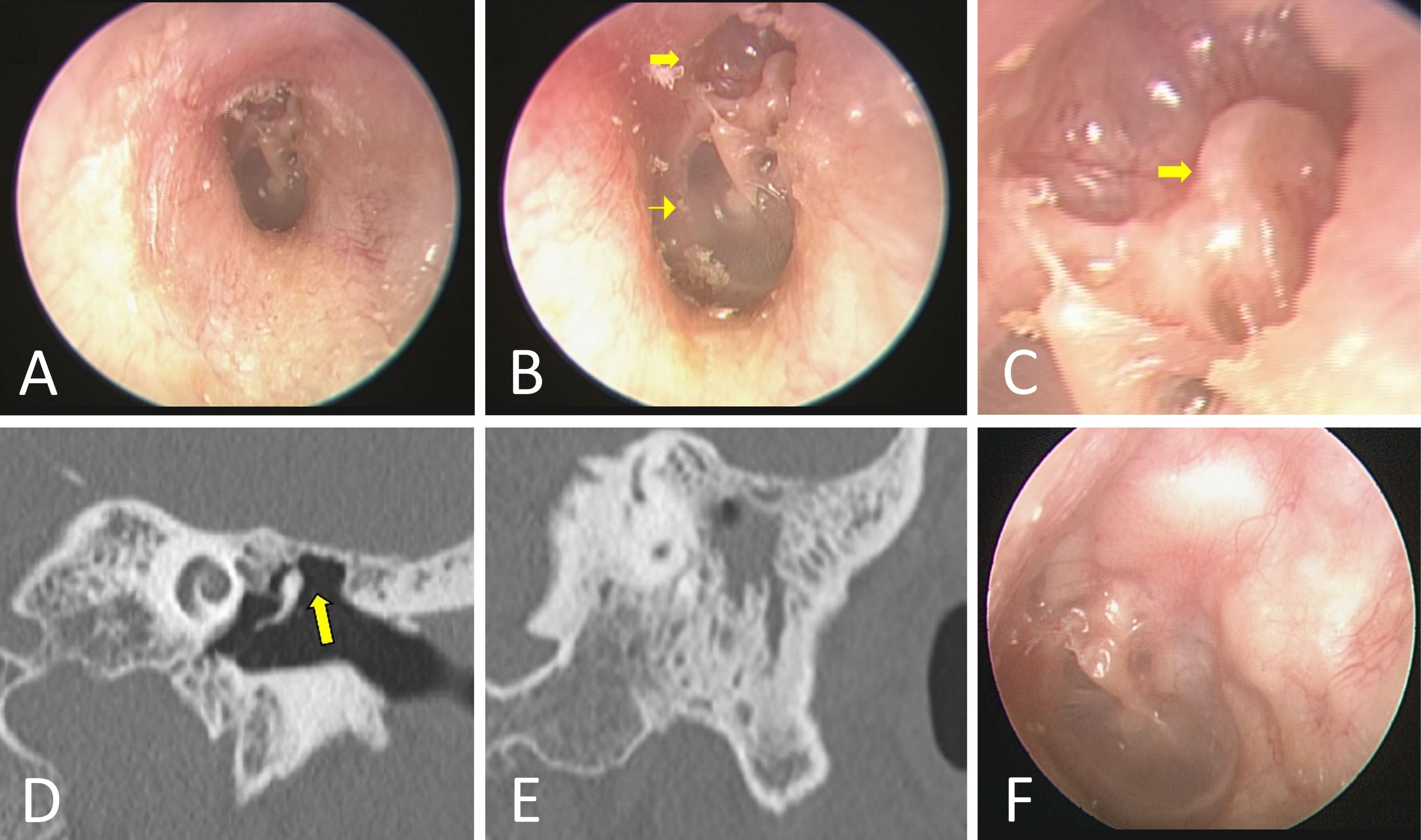
Figure 1. The otoscopic examination of the left ear reveals a deep retraction pocket in the par flaccida (A), as well as severe erosion of the scutum (arrow in panel B). While the pars tensa is normal (arrowhead in panel B), the malleus head is exposed and wrapped by the par flaccida (arrow in panel C). A clean and clear bottom is evident in the retraction pocket, and there are no signs of infection or accumulation of debris (C). High-resolution computed tomography (HRCT) images of the left temporal bone reveal scutum erosion (arrow in panel D) and a soft tissue mass in the mastoid (E). In five years of follow-up, there has been no evidence of recurrence of the disease (F).
At our hospital, an otoscopic examination of the left ear (Figure 1A) revealed a deep retraction pocket of the par flaccida with severe erosion of the scutum (arrow in Figure 1B). The bottom of the pocket was clear and clean, i.e., no signs of infection or the accumulation of debris; however, the malleus head was exposed and wrapped by the par flaccida (arrow in Figure 1C). A pneumatic otoscopy demonstrated that the mobility of the pars tensa (arrowhead in Figure 1B) was normal; and a hearing test showed that bilateral hearing was also normal. A tympanometric examination revealed bilateral normal middle ear status; and a sinoscopy showed bilateral chronic hypertrophic rhinitis with no evidence of Eustachian tube obstruction. The high-resolution computed tomography (HRCT) images of the left temporal bone revealed extensive erosion of the scutum (arrow in Figure 1D) and a soft tissue mass in the mastoid (Figure 1E), which was found to be a cholesteatoma following surgical exploration (Video 1). The presence of a cholesteatoma in the mastoid was later confirmed by histopathology. The patient exhibited no postoperative complications. During a five-year follow-up, no recurrences were observed in either the otoscopic exam (Figure 1F), the computed tomography, or the diffusion-weighted magnetic resonance imaging.
Video 1. Surgical exploration reveals a cholesteatoma in the mastoid.
Safe or Unsafe
The issue of whether retraction pockets of the tympanic membrane are safe or unsafe remains an open question. Retraction pockets that are relatively stable are generally considered “safe”, particularly if the bottom of the retraction pocket is clearly visible and does not show signs of infection or the accumulation of debris. Even after remaining undetected in a non-aggressive stable state for many years, retraction pockets may not present dangerous manifests.
In contrast, an unsafe or unstable retraction pocket may progressively drape around the ossicles, leading to bony necrosis and subsequent conductive hearing loss. Additionally, an unstable retraction pocket may deepen as desquamated keratin accumulates. The subsequent formation of a cholesteatoma may obstruct the opening of the pocket, thereby inducing ingrowth expansion into the middle ear cleft [8]. Undiscovered or untreated cholesteatomas may grow dangerously large and/or invade intratemporal structures, which can lead to intra- and extra-cranial complications [8-12].
In this case report, a retraction pocket that would normally have been regarded as “safe” was shown to be unsafe. The fact that the retraction pocket was clean and had a bottom area that was clearly visible led a non-competent ear specialist to falsely conclude that the retraction pocket was safe. The delay in diagnosing cholesteatoma for several years could have resulted in serious complications [9-13]. This case report has straightforward clinical implications. To begin with, the potentially dangerous complications associated with tympanic retraction pockets warrant clinical attention, even when symptoms appear to be mild. Early detection makes it possible to implement non-surgical measures or surgical measures that are less invasive than conventional treatments, which can reduce the risk of hearing-related complications, particularly in children [14,15]. Second, pneumatic otoscopy does not always reveal the first presentation of a tympanic retraction pocket, particularly when the examination is performed on an uncooperative infant or child. These diagnostic difficulties warrant a referral for a detailed otolaryngologic examination. Importantly, a computed tomography scan of the temporal bone should be considered for all patients suffering from tympanic membrane retraction, particularly those presenting otologic symptoms.
Surgery or Alternative Treatment Method
One important question is whether early surgical intervention is necessary in the treatment of a tympanic retraction pocket. There is no doubt that tympanoplasty (with or without mastoidectomy) is required for advanced cases with complications. Nonetheless, there is currently no consensus amongst otologists regarding the optimal management strategy for tympanic membrane retractions [16]. There are several reasons for this. First, the course of tympanic membrane retraction is unpredictable, and it has yet to be determined how long the status of a retraction pocket should be monitored. Long follow-up periods can be inconvenient, particularly for patients who do not live near an otolaryngologic clinic [15]. These points justify preventive early-stage surgical treatment. Surgical options include ventilation tube insertion and tympanoplasty with or without mastoidectomy [16]. The goal of surgery is to prevent or reduce structural damage while preserving unaffected middle ear structures; however, the choice of surgical technique tends to be guided by the preferences and experience of the surgeon.
Early surgical intervention, however, poses three levels of decision-making challenges. First, tympanic membrane retractions may be asymptomatic (i.e., hearing may be unaffected), as with the patient in this case report. Surgical intervention can damage the ossicles, which can lead to impaired hearing or even deafness. It can therefore be challenging to convince patients that surgery is necessary and/or worthwhile given the potential postoperative consequences. Conversely, no surgical procedure can guarantee the restoration of normal hearing in patients who present hearing loss associated with tympanic retraction. Third, a recent Cochrane review of high-quality but limited evidence (only two randomized controlled trials were available) could not conclusively support or refute the role of surgery in the management of tympanic membrane retraction [16].
Alternatively, a conservative watch-and-wait approach coupled with medical therapies aimed at preventing Eustachian tube dysfunction (such as decongestant nasal sprays, oral antihistamines and steroids, blowing up balloons, or inflation devices) may be adopted as a treatment strategy for tympanic membrane retraction pockets [16]. However, if patients choose early surgical intervention, surgeons should make them aware of the surgical expectations and outline all of the factors that could lead to complications. Regardless of the treatment plan, informed consent is essential for patients to ensure they understand what is involved during and after treatment.
It can be challenging to differentiate between safe and unsafe tympanic retraction pockets in clinical practice. In the current case report, a retraction pocket that had originally been deemed “safe” was in fact revealed to be unsafe. Clinicians need to be aware that a cholesteatoma could be hidden behind a tympanic retraction pocket. A temporal bone computed tomography scan should be considered for all patients who present with a retracted tympanic membrane, even in cases where otologic symptoms are absent. Nonetheless, given the inherent complexity and unpredictability of disease progression, further research is required to determine the optimal strategy for managing tympanic retraction pockets.
Received date: October 11, 2022
Accepted date: November 10, 2022
Published date: December 06, 2022
A portion of this work was presented by Dr. Kuo at the round table meeting at the 30th Politzer Society Meeting / 1st World Congress of Otology in Niigata, Japan, between June 30 and July 4, 2015. It should be noted that some of the figures have been published in the Preprint Archives of Clinical Images & Videos (Preprint Archives of Clinical Images & Videos 2017;1(1):1; DOI: 10.24983/scitemed.paciv.2017.00003).
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This research has received no specific grant from any funding agency either in the public, commercial, or not-for-profit sectors.
There are no conflicts of interest declared by either the authors or the contributors of this article, which is their intellectual property.
It should be noted that the opinions and statements expressed in this article are those of the respective author(s) and are not to be regarded as factual statements. These opinions and statements may not represent the views of their affiliated organizations, the publishing house, the editors, or any other reviewers since these are the sole opinion and statement of the author(s). The publisher does not guarantee or endorse any of the statements that are made by the manufacturer of any product discussed in this article, or any statements that are made by the author(s) in relation to the mentioned product.
© 2022 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). In accordance with accepted academic practice, anyone may use, distribute, or reproduce this material, so long as the original author(s), the copyright holder(s), and the original publication of this journal are credited, and this publication is cited as the original. To the extent permitted by these terms and conditions of license, this material may not be compiled, distributed, or reproduced in any manner that is inconsistent with those terms and conditions.
Video 1. Surgical exploration reveals a cholesteatoma in the mastoid.
The present study demonstrated that TEES could be a satisfying alternative to traditional microscopic surgery for the management of congenital cholesteatoma, even in pediatric patients. However, one-handed surgery demands greater skill and requires more practice to achieve a good outcome.
This study investigates the efficacy of conservative management using 5-fluorouracil (5-FU) for treating cholesteatoma in ambulatory care settings, offering an alternative for patients who prefer to avoid surgery. Over 13 years, 15 ears of 14 patients were treated with a 5% 5-FU cream and assessed using Takahashi's efficacy criteria. The results revealed positive outcomes, with 87% of cases deemed good and 13% as fair, with no poor evaluations. This approach may be suitable for specific populations, such as older adults and individuals in remote areas with limited access to specialized healthcare services.
The clinical significance of otitis media with effusion (OME), a complication associated with cleft lip/palate (CLP), is often overlooked in children. The author reviews the pathogenesis, clinical manifestations, and diagnoses of OME in children with CLP as well as the controversies surrounding treatment. He also provides a flowchart to guide the management of OME in children with CLP.
This report describes the case of a 41-year-old patient with a tympanic retraction pocket with complications related to retraction that may have been missed or delayed by clinicians in diagnosing the patient. The tympanic retraction pocket was discovered to have a clean bottom by a local clinic, but there was no evidence of progression of the condition. On a CT scan of the left temporal bone, it was revealed that the scutum had been extensively eroded. In addition, there was an expanding mass of soft tissue within the mastoid cavity. This mass was diagnosed as cholesteatoma by surgical and pathological examination. In this case, the tympanic retraction pocket with a clearly visible bottom was potentially unsafe. I believe this is an interesting case report that may be of interest to readers. My concern is whether early surgical intervention is necessary to treat a tympanic retraction pocket. In general, relatively stable retraction pockets are considered to be "safe", particularly when the bottom of the pocket is clearly visible and there are no signs of infection. Retraction pockets may present no signs of danger even after remaining undetected for many years in a non-aggressive stable state. It is for this reason that there is no consensus among otologists as to the most appropriate treatment strategy for tympanic membrane retractions. In regard to this issue, I am wondering what the authors' thoughts are on the matter.
ResponseYour insightful comments are much appreciated. As we agree, there is a critical question to be addressed in the context of tympanic retraction pockets, namely whether early surgical intervention is necessary to treat the condition. Early surgical interventions present three levels of decision-making challenges from a clinical perspective. First, tympanic membrane retractions may be asymptomatic (i.e., hearing may be unaffected), as with the patient in this case report. Surgical intervention can damage the ossicles, which can lead to impaired hearing or even deafness. It can therefore be challenging to convince patients that surgery is necessary and/or worthwhile given the potential postoperative consequences. Conversely, no surgical procedure can guarantee the restoration of normal hearing in patients who present hearing loss associated with tympanic retraction. Third, a recent Cochrane review of high-quality but limited evidence could not conclusively support or refute the role of surgery in the management of tympanic membrane retraction. Alternatively, a conservative watch-and-wait approach coupled with medical therapies aimed at preventing Eustachian tube dysfunction (such as decongestant nasal sprays, oral antihistamines and steroids, blowing up balloons, or inflation devices) may be adopted as a treatment strategy for tympanic membrane retraction pockets. However, if patients choose early surgical intervention, surgeons should make them aware of surgical expectations and outline all of the factors that could lead to complications. Regardless of the treatment plan, informed consent is essential for patients to ensure they understand what is involved during and after treatment.
A 41-year-old male was diagnosed with a tympanic retraction pocket and complications related to retraction that may have been missed or delayed by clinicians. The bottom of the tympanic retraction pocket was clean, and there was no evidence of progression. CT scans of the left temporal bone revealed extensive erosion of the scutum. Following surgical and pathological examinations, cholesteatoma was diagnosed in the mastoid cavity. An unsafe tympanic retraction pocket with a clearly visible bottom could be seen in this case. After carefully analyzing the case report, I believe there is a lot of value to be gained from it, and I believe it deserves to be published. There is, however, one point that needs to be discussed further before publication, which is the importance of an effective management strategy when managing tympanic retractions. Many surgeons choose to consider surgical interventions as preventative measures rather than waiting until a serious problem occurs. However, in my experience as an otolaryngologist, it may be more beneficial to follow up regularly on patients who do not have any immediate complications over the long term. I am of the opinion that patients with retraction pockets may be overtreated by procedures such as tympanoplasty or the insertion of ventilation tubes. For patients without obvious signs of complications, a conservative watch-and-wait strategy may be a suitable option. I believe that a more detailed discussion of this topic would be of interest.
ResponseIt is greatly appreciated that you shared your views with us. For cases with advanced levels of complications, there is no doubt that tympanoplasty (with or without mastoidectomy) should be performed. However, otologists have not yet developed a definitive consensus regarding the most effective management strategy for tympanic retractions. The reasons for this can be attributed to a number of factors. As a first concern, the course of tympanic retraction is unpredictable. It is not yet known how long a retraction pocket should be monitored. For those patients who do not live near an otolaryngology clinic, following up on a regular basis for an extended period of time may be inconvenient. As a preventive measure, we believe that these points justify the need for early surgical intervention. Surgery options include the insertion of a ventilation tube and tympanoplasty (with or without mastoidectomy). The goal of surgery is to prevent or reduce structural damage while preserving unaffected middle ear structures; however, the choice of surgical technique tends to be guided by the preferences and experience of the surgeon.
Kuo CL, Lien CF. Safe tympanic retraction may be unsafe: A false sense of security in a patient with cholesteatoma. Arch Otorhinolaryngol Head Neck Surg 2022;6(2):3. https://doi.org/10.24983/scitemed.aohns.2022.00168