Objectives: Vascularized lymph nodes transfer (VLNT) has been noticed as an effective treatment for lymphedema. Several sites of lymph nodes have been reported as donor sites, and the inguinal nodes are one of the major donor sites for upper extremity lymphedema. These nodes enable to perform VLNT and breast reconstruction by transferring an abdominal flap containing inguinal nodes. Our study aimed to recognize how many nodes could be added to the abdominal flap.
Methods: We reviewed 48 cases and 96 sides multi detector computed tomography (MDCT) images, which were taken from 2011 to 2014, to prepare for deep inferior epigastric perforator (DIEP) flap. All the cases were females. We counted the number of inguinal lymph nodes. To avoid the donor site mobility such as newly caused lymphedema, the superficial inguinal nodes sited superior to the junction of femoral vein and greater saphenous vein are appropriate.
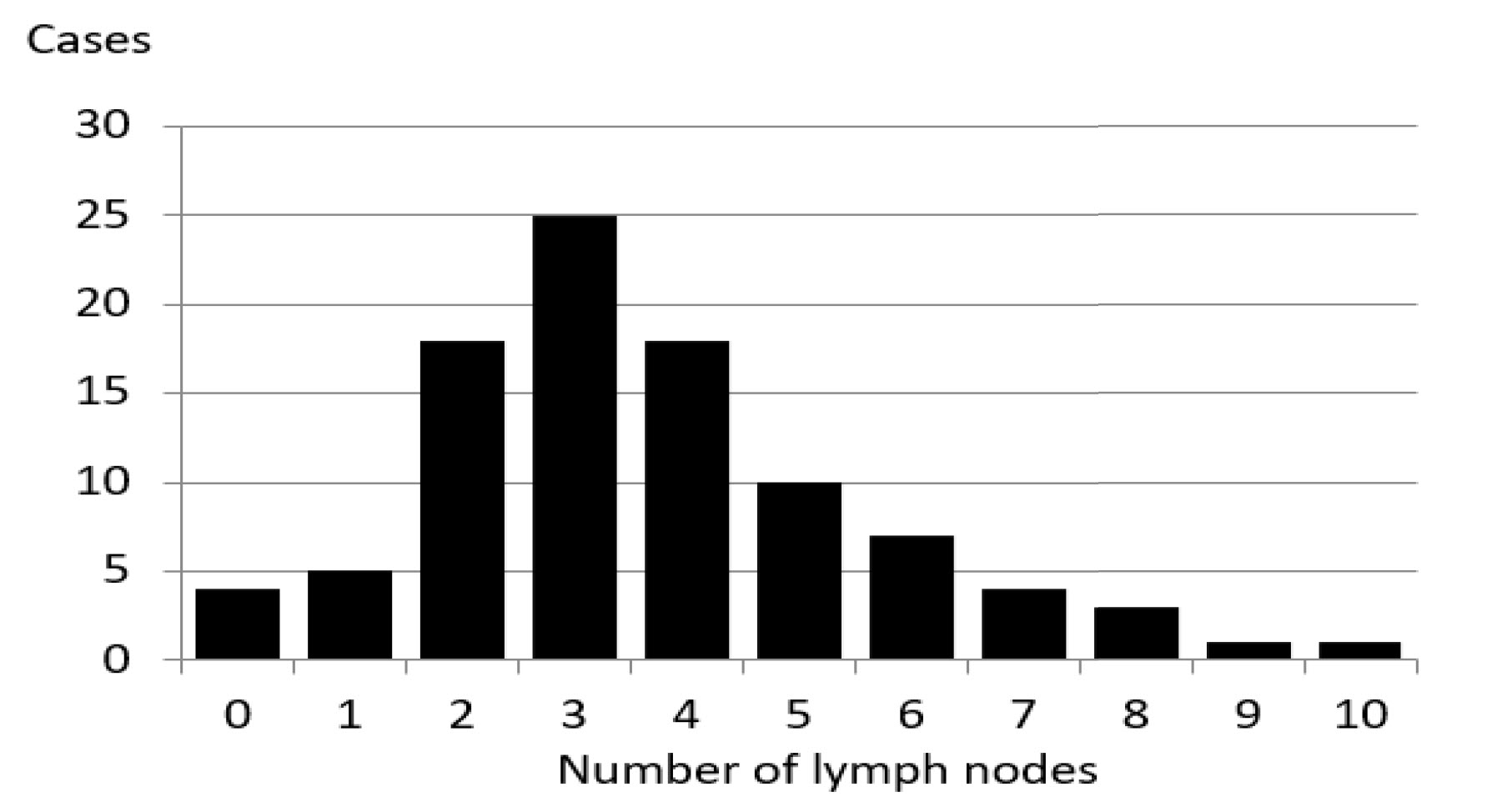
Results: The number of lymph nodes ranged between 0 and 10, with 3 in 25 sides (26%) and 4 in 18 sides (19%). The average was 3.67 for single side. No significant difference existed between left and right sides.
Conclusion: The lymph nodes-added abdominal flap transfer is a promising procedure, which enables breast reconstruction and lymphedema treatment at the same time. Inguinal nodes are fed by superficial circumflex iliac artery (SCIA), superficial inferior epigastric artery (SIEA), and medial artery. The commonest abdominal flap for breast reconstruction is, nowadays, deep inferior epigastric artery perforator (DIEP) flap from the view of less donor site morbidity. The added inguinal nodes are fed by retrograde flow via SCIA or SIEA. In this study, as an average, 3.67 nodes can be joined to abdominal flap. However, there were 4 percent of cases without countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
Vascularized lymph node transfer (VLNT) is known to be an effective way of treating lymphedema. Several lymph node sites have been reported as suitable donor sites [1], with the inguinal lymph nodes being one of the major donor sites for upper extremity lymphedema treatment. These nodes enable simultaneous VLNT and breast reconstruction by transferring an abdominal flap containing the inguinal lymph nodes. Recent reports suggest that to avoid donor site iatrogenic lymphedema, superficial inguinal nodes superior to the saphenous junction are suitable [2,3]. Our study aimed to identify how many nodes could be included in the abdominal flap.
We reviewed 96 multi detector computed tomography (MDCT) images taken perioperatively from the left and right sides of the abdomen of 48 cases while preparing for deep inferior epigastric perforator (DIEP) flap breast reconstruction surgery between 2011 and 2014. All the cases were females. We counted the number of superficial inguinal lymph nodes superior to the saphenofemoral junction. These nodes were fed by the superficial inferior epigastric artery (SIEA) and the superficial circumflex iliac artery (SCIA), and could be attached to the abdominal flap.
The number of lymph nodes ranged between 0 and 10 (Figure 1), with 3 in 25 abdominal side images (26%), and 4 in 18 side images (19%). The average number of lymph nodes in a single side image was 3.67. No significant differences existed between the left and right abdominal side images. There were 4 cases with no countable lymph nodes.
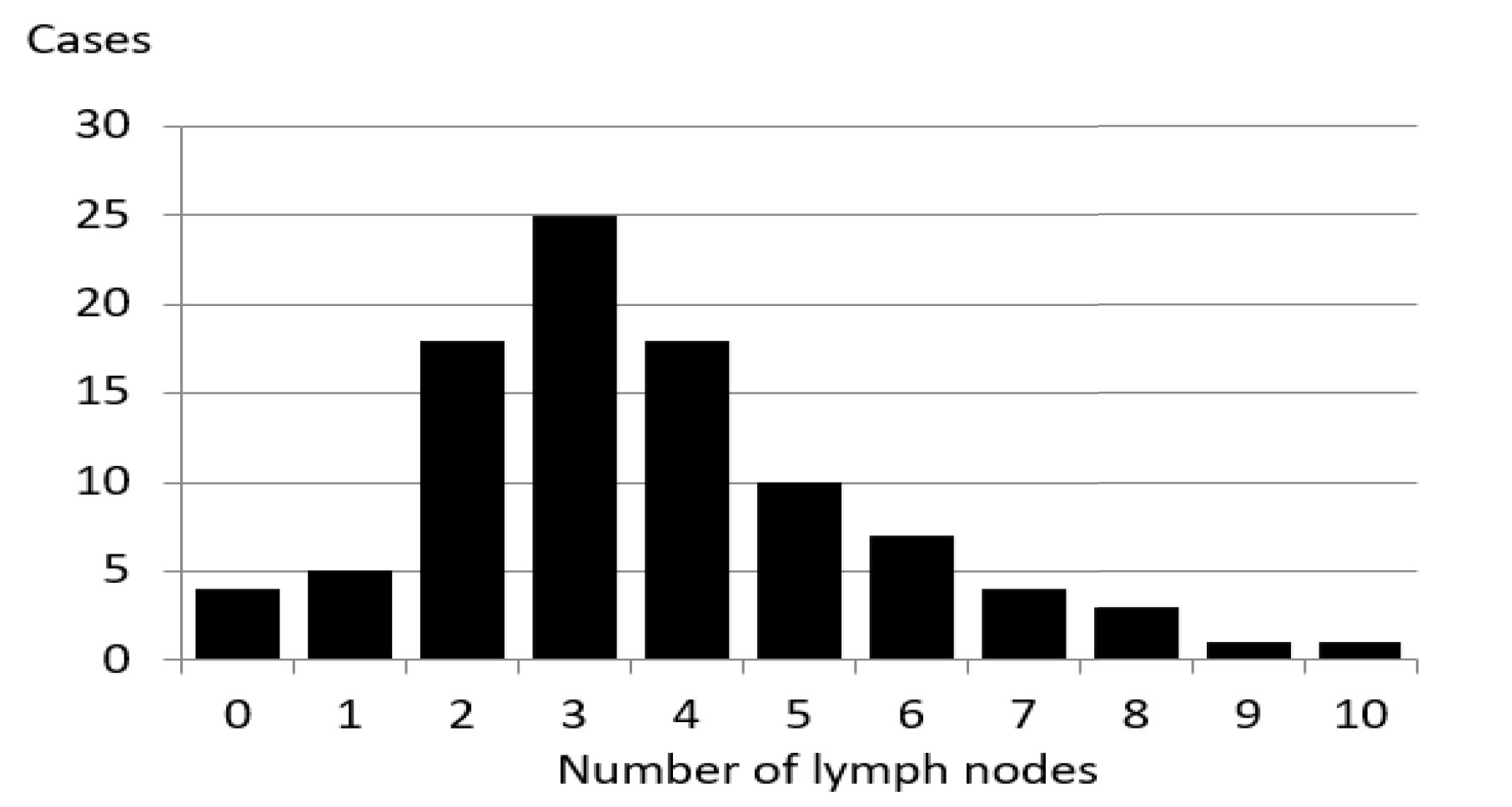
Figure 1. Number of superficial inguinal lymph nodes in superior part.
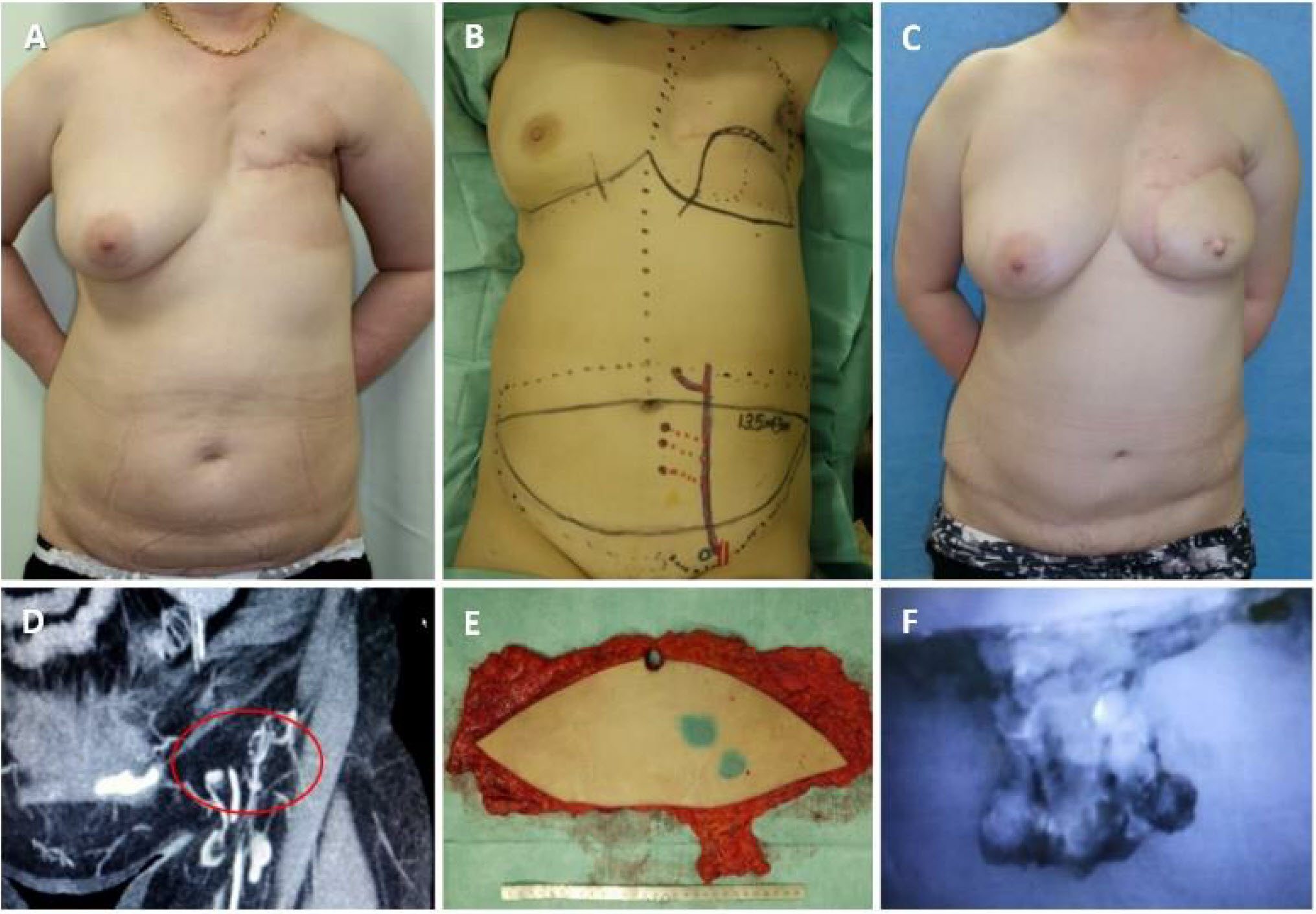
A 54-year-old woman had lymphedema in the left upper extremity caused by total mastectomy with axillary lymph node dissection for breast cancer; she had undergone surgery, chemotherapy and radiation therapy, one year earlier. There was no improvement in the symptoms following conservative treatment with compression therapies. There was significant fibrosis in the upper extremity and shallow pitting edema was observed, indicating a reversible state of lymphedema. We defined end-to-side lymphaticovenular anastomosis of this patient's lymphedema stage as IIb in ILS scale.
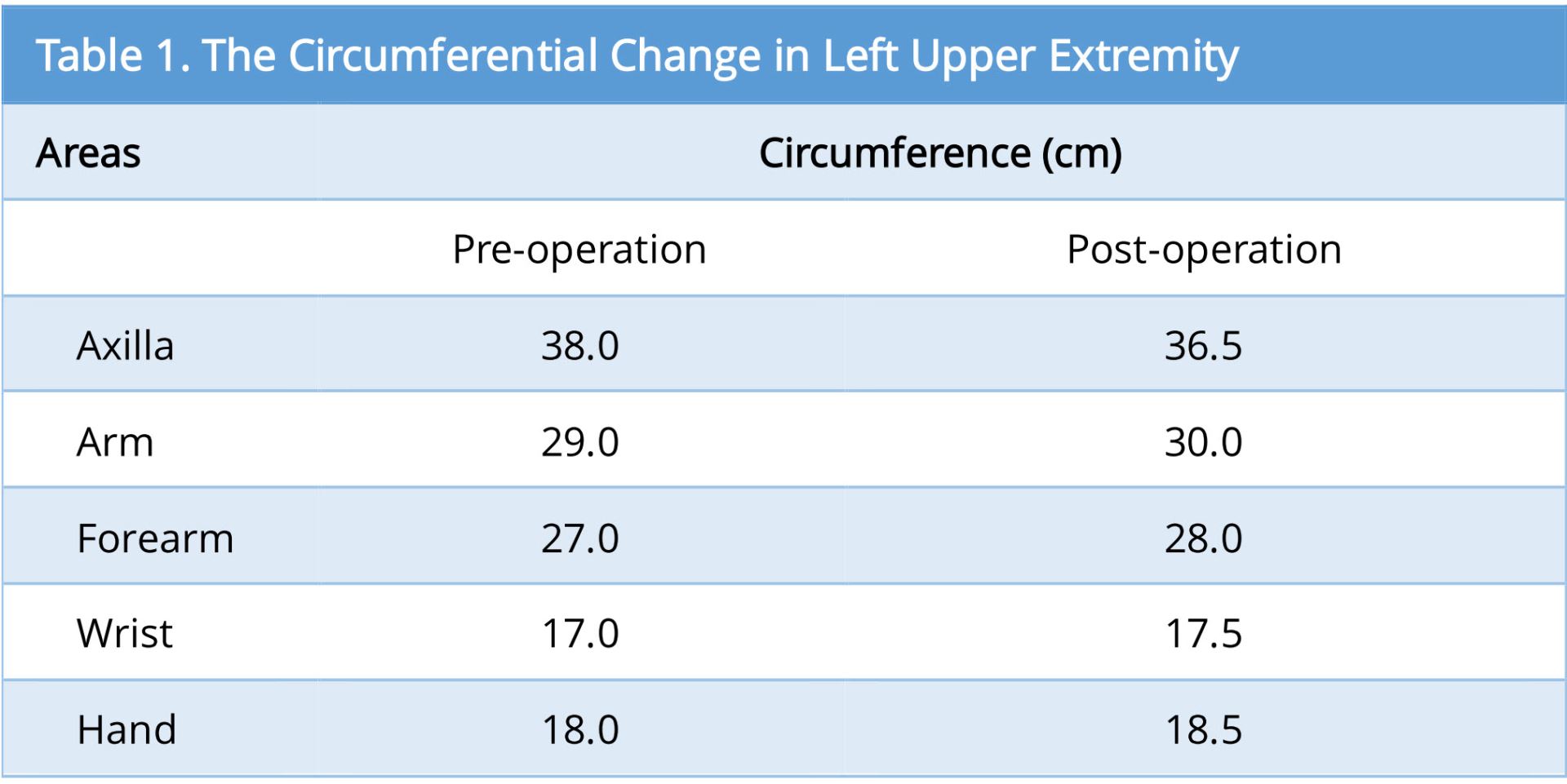
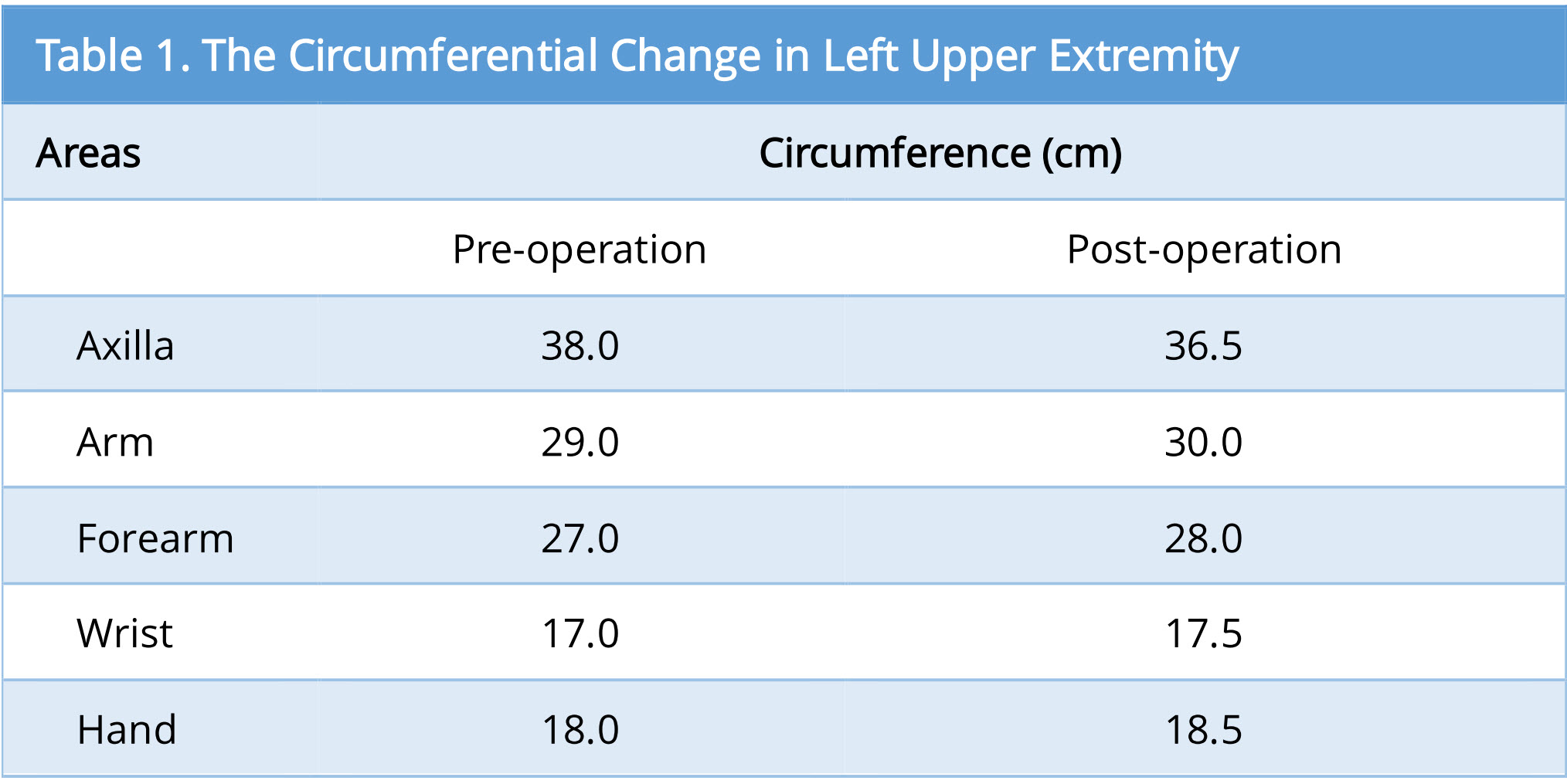
As the surgical therapy for the lymphedema, two were performed in the left dorsum of her hand (Figure 2A). Slight improvement in her hand was felt as decrease in swell, but insufficient. One year later, DIEP flap with lymph nodes along SIEA was transferred (Figure 2B and 2E). We planned to include 4 lymph nodes in the flap according to enhanced MDCT (Figure 2D). The lymph nodes were well enhanced by intravenous injection of indocyanine green (ICG) after harvesting of the flap. We could detect at least 3 lymph nodes in the flap (Figure 2F). The flap was set in longitudinal position. The subcutaneous tissue in axilla region was too hard and thin to dissect it safely, probably due to the late effect of radiation therapy. So, a pocket for lymph node flap was made just under the axilla, and the lymph nodes were inserted to it. Slight decrease in circumference was observed mainly in her upper arm after 1-year postoperatively (Figure 2C). The circumferential change in left upper extremity was mentioned (Table 1). Donor site complication, such as newly caused lymph edema in the lower extremity or seroma in the abdomen, was not experienced. In this case, improvement of the circumference was limited in just around the axilla, probably due to insufficient subcutaneous dissection in the area.
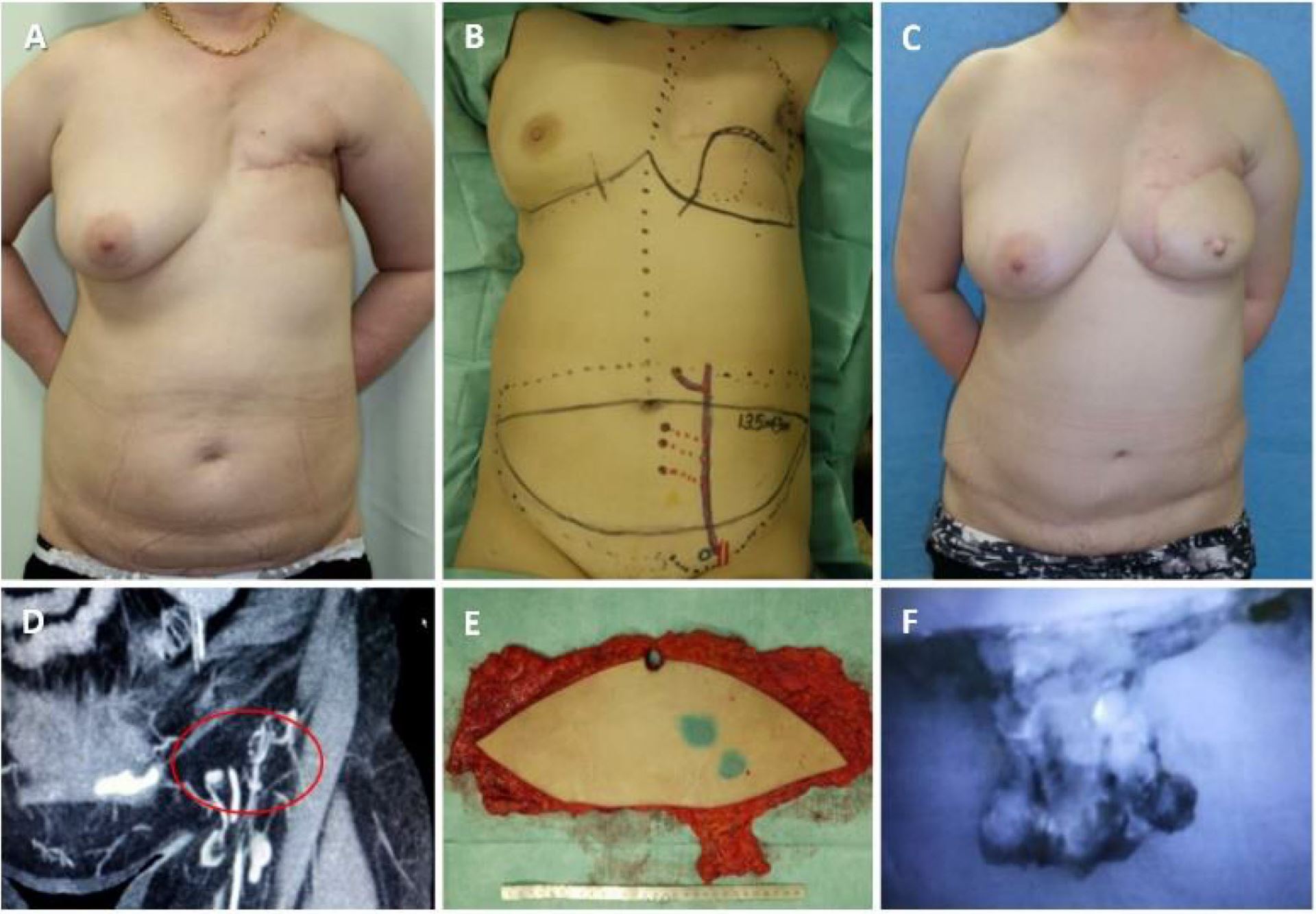
Figure 2. A 54-year-old female, after total mastectomy for her left breast cancer. Post chemotherapy and radiation. Lymphaticovenular anastomoses were performed formerly in her left dorsum of hand (A). DIEP flap with lymph nodes (LNs) along SIEA was transferred (B and E). We planned to include 4 LNs in the flap according to enhanced MDCT (D). The LNs were well enhanced by intravenous injection of ICG (F). The flap was set in longitudinal position, and the LNs were inserted to axilla. Slight decrease of circumference was observed in mainly in her upper arm postoperative one year (C).
The lymph nodes-added abdominal flap transfer is a promising procedure, which enables simultaneous breast reconstruction and lymphedema treatment. The superficial inguinal lymph nodes are fed by the SCIA, SIEA, and the medial artery [4]. Recent studies have shown that nodes in the inferior-medial and the central areas of the saphenofemoral junction should not be selected as donor sites for VLNT, because they are the primary superficial nodes draining the lower limb [2,3]. Nodes in the superior area of the saphenofemoral junction are said to be safe, but they can be the draining nodes for the lower limb in 15% of the cases [3]. Scaglioni et al. [5] showed that the superficial inguinal lymph nodes could be divided into three subgroups: abdominal, medial thigh, and lateral thigh nodes. The dominant lymph nodes draining the leg were in the lower part of the inguinal triangle. To avoid iatrogenic lymphedema, reverse lymphatic mapping is useful to distinguish between “dangerous” nodes and nodes suited to VLNT [6]. In our case report, we couldn’t use this method, because it was performed before publishing the method.
Nowadays, the workhorse flap for breast reconstruction is the DIEP flap due to less subsequent donor site morbidity. The added inguinal nodes are fed by retrograde flow via SCIA or SIEA. This study shows that, on average, 3.67 nodes can be included in the abdominal flap. The number of nodes ranged between 0 and 10. Chen et al recently reported that the number of vascularized lymph nodes transferred correlated positively with the degree of volume reduction in rats [7]. The side with more lymph nodes should be chosen for transfer. It was worth noting that there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is recommended for this procedure.
We reviewed the MDCT images to show the number of lymph nodes superior to the saphenofemoral junction. In this study, on average, 3.67 nodes existed. However, there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
Received date: April 30, 2017
Accepted date: September 15, 2017
Published date: November 07, 2017
© 2017 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Authors report a case of lower extremity lymphedema treated by LVA that preoperatively mapped not only lymphatic vessels by PDE, but also veins and venules using Veinsite™ .
Combining intraoperative ICG lymphography with NIR vein visualization can aid supermicrosurgeons in identifying lymphatic vessels and superficial venules to guide LVA incision placement. This guided approach significantly improves successful creation of LVAs when compared to the blind (anatomic) approach. In addition, the absence of linear ICG lymphographic patterns does not prevent formation of successful LVAs.
Immediate limb compression following the LVA procedure facilitates lymphatic drainage and increases the surgical efficacy by increasing the number of functioning anastomoses, and is a recommended postoperative practice.
This case report demonstrates an important supermicrosurgical technique for lymphedema, which was established by Isao Koshima in 1994. So far, over 2,000 cases of limb edema have been treated by this surgical method.
LVA and vascularized lymph node transfer VLNT are established lymphedema treatments. However, LVA is only effective for early disease and VLNT can cause donor-site lymphedema and contour deformity. VLVT is free of these limitations. The authors described their experience of a new VLVT technique.
ICG lymphography is an invaluable tool in lymphedema management. Both immediate and delayed scans are needed when performing the study. The delayed scan needs to be performed at the time of the lymphographic plateau to appreciate the full extent of the pathology. Using a recumbent cross trainer, the lymphographic plateau can be achieved in 15 minutes following ICG injection. We have found this exercise enhanced ICG lymphography protocol worthwhile of adoption by high volume lymphedema centers to raise diagnostic accuracy and efficiency.
This article holds critical relevance for healthcare professionals, particularly in the fields of microsurgery, oncology, and vascular medicine. It thoroughly examines the diagnostic challenges faced in distinguishing between recurrent lymphedema and deep vein thrombosis in elderly cancer patients following lymphovenous anastomosis surgery. It highlights the significant risk of misdiagnosing deep vein thrombosis as lymphedema, a mistake that can delay critical treatment due to their clinical similarities. The case study of a 79-year-old patient emphasizes the importance of a comprehensive reassessment, considering the patient's entire medical history, including the effects of cancer treatments like immunotherapy. The article stresses the need for a holistic approach to patient management and the utilization of advanced diagnostic tools for accurate diagnosis and treatment. It is essential reading for its insights into the complex dynamics of postoperative care and the critical importance of accurate diagnosis in treating elderly cancer patients effectively.
LVA and vascularized lymph node transfer VLNT are established lymphedema treatments. However, LVA is only effective for early disease and VLNT can cause donor-site lymphedema and contour deformity. VLVT is free of these limitations. The authors described their experience of a new VLVT technique.
The authors describe various patient and breast-related factors that influence surgical outcomes while also addressing some techniques and principles for aesthetic microsurgical reconstruction.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
I accept the revised version for publication
Accepted. Please go ahead and publish it.
Tanakura K, Matsumoto A, Kuramoto Y, Sawaizumi M. The number of lymph nodes that can be added to an abdominal flap for breast reconstruction: Review of enhanced MDCT images. Int Microsurg J 2017;1(3):1. https://doi.org/10.24983/scitemed.imj.2017.00041