Introduction: The anterolateral and anteromedial thigh (ALT and AMT) flaps are the most commonly used thigh free flaps for intraoral reconstruction. Recently, the profunda artery perforator (PAP) flap has been proposed as an alternative. This study aimed to compare the thickness of these thigh flaps and to identify the factors influencing flap thickness in our population.
Methods: The study sample comprised legs (n = 72) of patients who underwent head and neck reconstruction with a fibula free flap. Preoperative computed tomographic angiography was used for morphologic analysis. Pearson correlation analysis was used to assess the relationship between flap thickness and different continuous variables. A repeated measures mixed linear model analysis was performed using all the available measurements. The adjusted marginal means of each flap were estimated using a fixed-effect model.
Results: Flap thickness was more in women (p < 0.001) and was correlated with body mass index (BMI). The R2 coefficients for ALT, AMT, and PAP were 0.64, 0.69, and 0.48, respectively (p < 0.01). ALT thickness (1.61 ± 0.07 cm) was significantly lower than AMT thickness (2.05 ± 0.08 cm, p < 0.0001). PAP thickness was significantly higher than the thickness of the ALT/AMT flaps when the measurement was made over the first perforator of the adductor magnus (2.31 ± 0.12 cm, p < 0.0001), but there was no significant difference when the measurement was made over the second perforator (1.88 ± 0.09 cm, p > 0.05).
Conclusions: Thigh flaps tend to be thicker in women and in those patients with high BMI. The thigh flap that is least influenced by BMI is the PAP flap. The PAP flap harvested around the second perforator of the adductor magnus can be as thin as the ALT flap.
Soft tissue microsurgical reconstruction in the head and neck regions can be performed with different types of free flaps. For decades, the anterolateral and anteromedial thigh regions have been considered as the ideal donor sites [1,2], especially in Asian countries. Recently, the profunda artery perforator (PAP) flap harvested from the posteromedial region of the thigh has been proposed as a good choice for use in oral cavity reconstruction [3,4,5]. However, in the Western countries, thigh flaps, especially the PAP flaps, are not used as often as in the Asian countries for oral reconstruction because there are concerns regarding the greater thickness of thigh flaps as compared with the radial forearm free flaps (RFFF).
There are previous publications on anterolateral thigh (ALT) flap thickness measured with Doppler ultrasound [6,7] and only one study using computed tomographic angiography (CTA) [8]. However, none of these studies compare ALT flap thickness with PAP flap thickness in the same patient.
The aim of this study was to compare the PAP flap thickness with the thickness of other thigh flaps that were more commonly used for intraoral reconstruction and to identify the factors influencing its thickness in our population using CTA. This information would be useful to facilitate flap selection based on desired tissue volume in patients with greater thigh thickness, like our population.
Study Sample
The study sample comprised 72 legs of 36 patients. The inclusion criteria were the patients who underwent head and neck microsurgical reconstruction with a fibula free flap and a preoperative CTA. The exclusion criteria consisted of the antecedent of previous thigh flap harvested. CTA was performed on a 64-slice multiple detector computed tomography scanner (LightSpeed VCT; GE Healthcare, Milwaukee, WI, USA) using a standardized protocol. Data post-processing was done using the open-source software HorosTM v 1.1.7 (GNU Lesser General Public License, version 3).
Morphologic analysis of flap thickness and perforator location was done for the ALT flap, the anteromedial (AMT) flap, the distal superficial femoral artery perforator (d-SFAP) flap, and the PAP flap in all 72 legs. The d-SFAP flap is not commonly used for intraoral reconstruction, but it was also included in this study because of the constancy of the location of its perforator. For the ALT flap, the references were the anterior superior iliac spine (ASIS) and the superolateral border of the patella. The best perforator around the midpoint between both references was identified and its location relative to the ASIS was registered. The same references were used for the AMT flap. The cutaneous perforator of the AMT flap was located close to the intersection between the rectus femoris and sartorius muscles. The perforator’s location (relative to the ASIS) and its origin—whether arising from the lateral circumflex femoral artery (LCFA), medial circumflex femoral artery (MCFA), or superficial femoral artery (SFA) — were identified. For the PAP flap, the references were the ischial tuberosity and the superomedial border of the patella. The first and second perforators of the adductor magnus were registered. So, two PAP flaps were considered in each leg: one PAP flap based on the first proximal perforator of the adductor magnus (PAP1) and another PAP flap based on the second or distal perforator (PAP2). The d-SFAP flap was based on a direct cutaneous branch of the SFA. The references used to locate this branch were the pubic tubercle and the superomedial border of the patella (Figure 1).
To allow comparisons between the patients with different thigh lengths, longitudinal measures were expressed as a percentage of the total length between the reference points for each flap. Flap thickness was measured at the point where the cutaneous perforator entered the deep fascia (Figure 2).
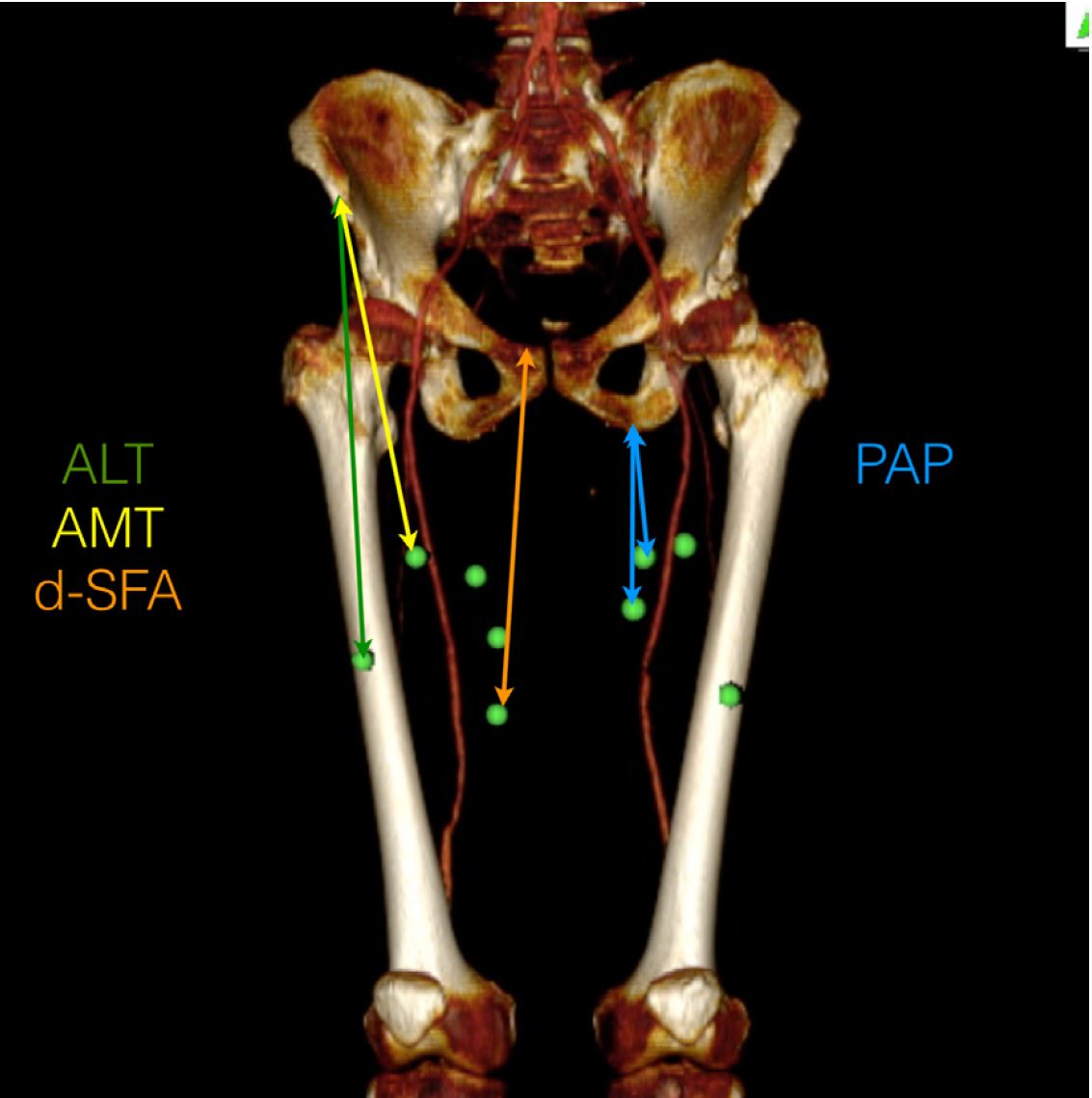
Figure 1. Example of measurements from proximal reference points to the perforators. ALT, anterolateral thigh; AMT, anteromedial thigh; d-SFAP, distal superficial femoral artery perforator; PAP1, profunda artery perforator flap based on the first perforator of the adductor magnus; PAP2, profunda artery perforator flap based on the second perforator of the adductor magnus.
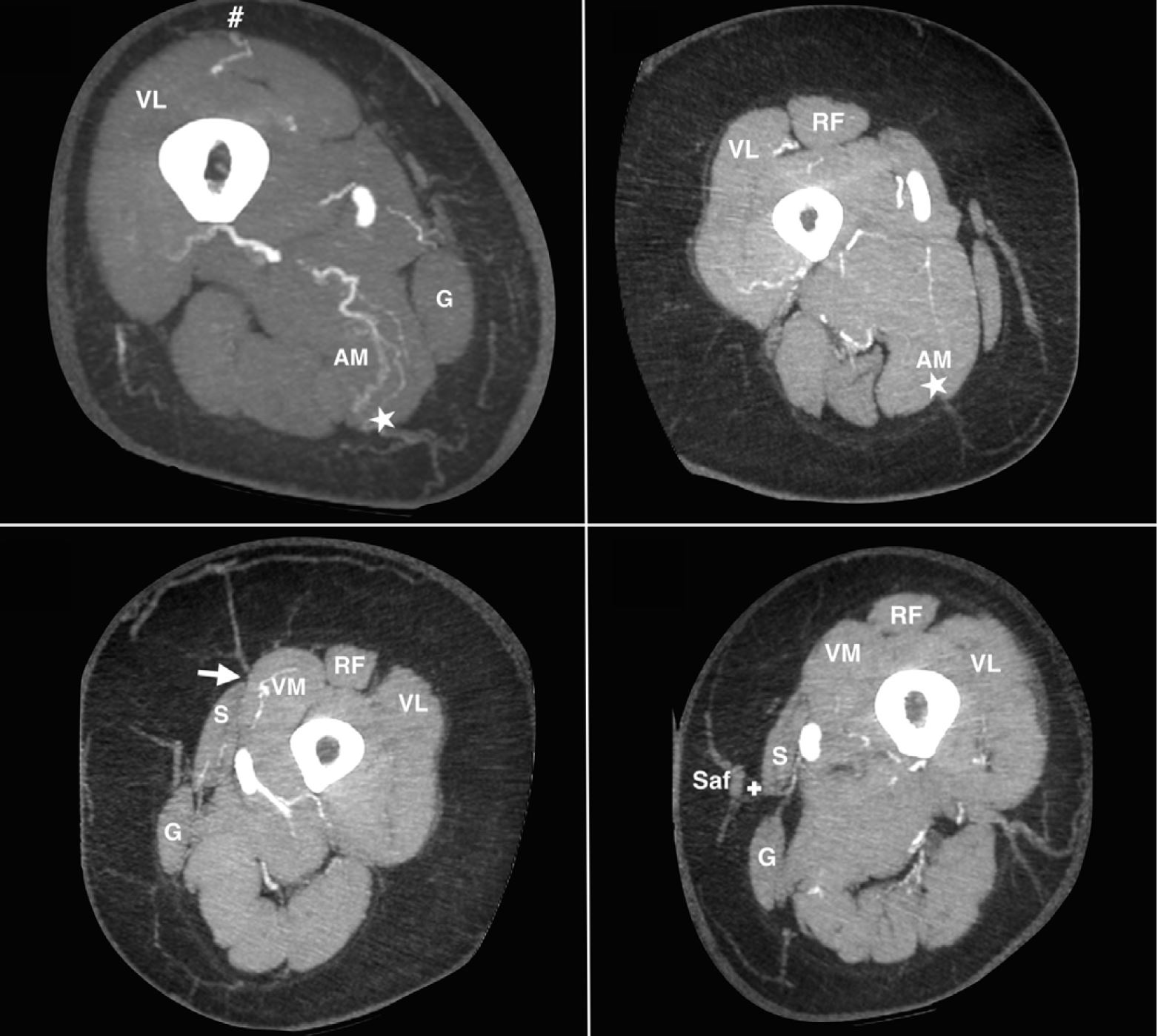
Figure 2. Axial CTA images: perforators of different thigh flaps. Thickness was measured at the point where the cutaneous perforator entered the deep fascia. The arrow indicates the anteromedial thigh perforator; the # indicates the anterolateral thigh perforator; the star indicates the profunda artery perforator; the cross indicates the distal superficial femoral artery perforator. AM, adductor magnus; G, graciligs; RF, rectus femoris; S, Sartorius; Saf, saphenous vein; VL, vastus lateralis; VM, vastus medialis.
Statistical Analysis
Statistical analysis was done using R v 3.1.1. (CRAN, Vienna). Normality was assessed using the Kolmogorov-Smirnov test and by visual inspection of the shape of histograms. The independent samples t-test was used to test the statistical differences between the means of the two given groups, as in the comparison of flap thickness in men and women. Pearson correlation analysis was used to assess the relationship between flap thickness and different continuous variables. A repeated-measures mixed linear model analysis was performed using all the available measurements of the total thickness (36 subjects, 72 legs, 360 flaps). The type of flap (ALT, AMT, d-SFAP, PAP1, PAP2) and side (left or right) were included in the model as repeated measures factors. The most appropriate covariance structure for the residuals (repeated covariance type) was a first-order autoregressive structure with heterogeneous variances. Parameters were estimated using the maximum likelihood method. A fixed-effect model was built and the marginal means of each flap were estimated, taking into consideration of the covariates such as sex, body mass index (BMI), and the relative distance from the proximal reference point to the point where the thickness of each flap was measured (longitudinal measures were expressed as a percentage of the total length between the reference points for each flap). Bonferroni adjustment was used for multiple comparisons. The threshold for significance was set up to 0.05.
In this sample of 36 patients, reconstruction was necessary because of oral carcinoma (25 patients), ameloblastoma (5 patients), trauma sequelae (3 patients), or radionecrosis (3 patients). Basic descriptive statistics are summarized in Table 1 and individual data are shown in Table 2.
The best identifiable perforator of the ALT flap was located about 21.8 ± 2.57 cm (mean ± standard error) from the ASIS (50.1% of the total length between the references). A reliable perforator for the AMT flap located around the intersection between the rectus femoris and sartorius muscles was present in 52/72 legs (72.3%); the origin of the perforator was from the LCFA in 38/72 legs (52.8%), from the SFA in 10/72 legs (13.9%), and from the MCFA in 4/72 legs (5.6%). In 20/72 legs (27.7%), the best perforator for the AMT arose very distally from the SFA (far from the intersection between the rectus femoris and sartorius muscles). The perforator of the d-SFAP was located about 20.5 ± 3.17 cm from the pubic tubercle (57% of the total length between the references). The first and second perforators of the adductor magnus muscle were located about 8 ± 1.88 cm and 10.84 ± 2.32 cm, respectively, from the ischial tuberosity (26% and 35% of the total length between the references).
For each kind of flap, the thickness was significantly higher in women (p < 0.001) (Table 3). Thickness was also correlated with BMI. The R2 coefficients for ALT, AMT, d-SFAP, and PAP were 0.64, 0.69, 0.62, and 0.48, respectively (p < 0.01).
ANOVA showed significant differences between the thicknesses of the four kinds of thigh flaps (Figure 3). ALT thickness (1.61 ± 0.07 cm) was significantly lower than AMT thickness (2.05 ± 0.08 cm) and d-SFAP thickness (2.8 ± 0.09 cm, p < 0.0001). The thickness of the PAP flap was significantly higher than that of the ALT flap when the measurement was made over the first perforator (2.31 ± 0.12 cm, p < 0.0001), but it was not significantly different from the ALT/AMT flaps when the measurement was made over the second perforator (1.88 ± 0.09 cm, p > 0.05)
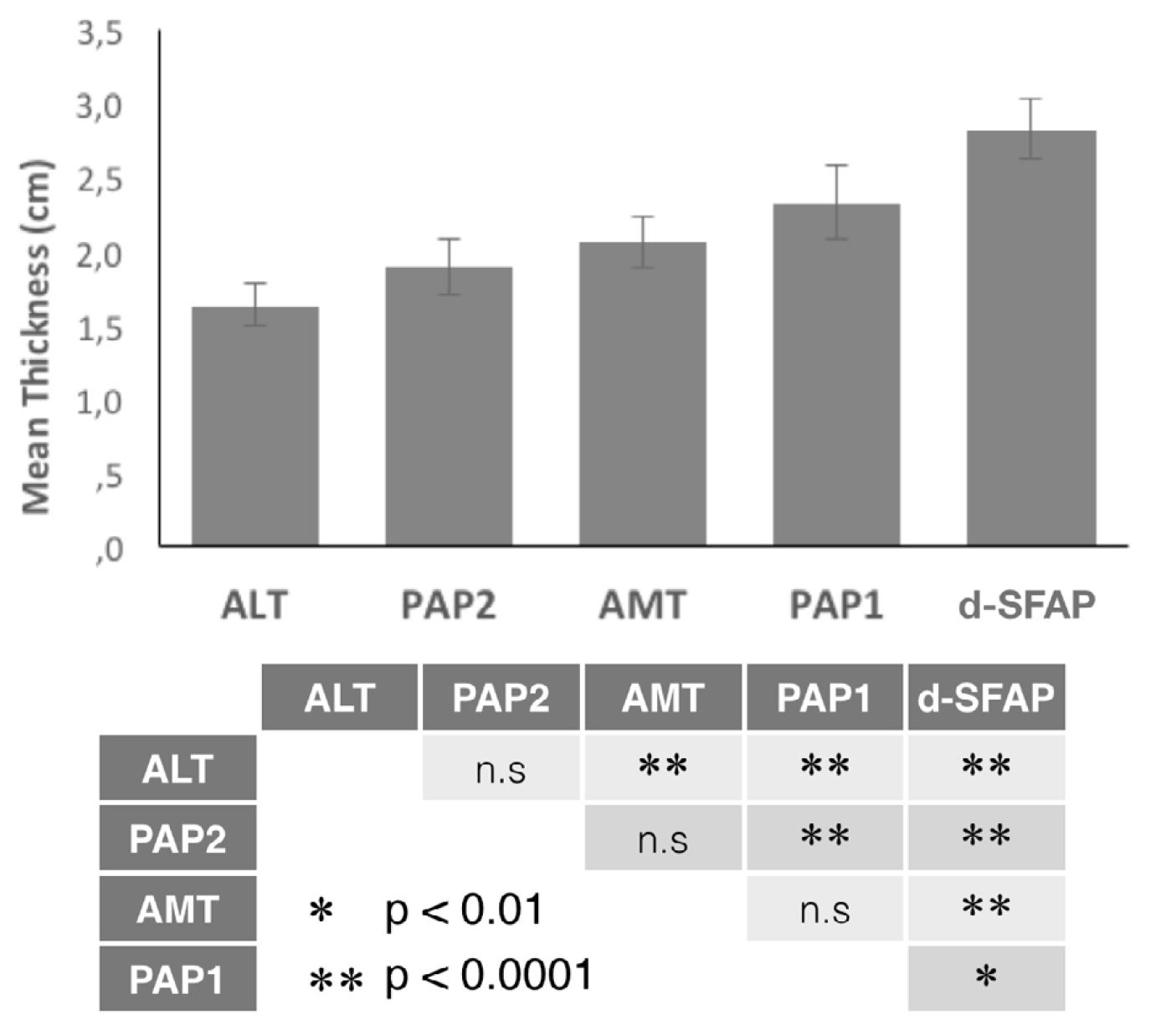
Figure 3. Graph illustrates the differences in thickness measured in the location of the perforator artery of each flap in a single patient. Estimated marginal means of flap thickness were adjusted using the following covariates: relative distance from proximal reference at mean 43.1, BMI at mean 26.7, and sex using a repeated-measures mixed linear model analysis (n = 36, F = 69.264; p < 0.001; -2 log likelihood = 473.217). The table below the graph shows the results of the post-hoc tests with Bonferroni adjustment for multiple comparisons. ALT, anterolateral thigh; AMT, anteromedial thigh; BMI, Body mass index (kg/m2); d-SFAP, distal superficial femoral artery perforator; n.s, not significant; PAP1, profunda artery perforator flap based on the first perforator of the adductor magnus; PAP2, profunda artery perforator flap based on the second perforator of the adductor magnus.
Intraoral reconstruction can be performed using different types of thigh flaps. Flap thickness is an important factor to be considered during flap selection. In this paper, we present our anthropomorphic analysis of different thigh flaps in a Spanish population.
The locations of the best identifiable perforators for the ALT flap in our sample are similar to those described in the previous reports [1]. For the AMT flap, the most common origin of the perforator found at the intersection between the rectus femoris and sartorius muscles was the LCFA, which was similar to the previous reports [9]. Mojallalal et al. [10] have described the constancy of the location of the d-SFAP flap perforator at a mean distance of 22.79 ± 1.55 cm from the pubic tubercle and in close relation with the saphenous vein, which is comparable to the mean distance of 20.5 ± 3.17 cm in our study. Our data are also consistent with other studies that have found most of the perforators of the PAP flap located 8-10 cm from the pubic crease [3].
Previous researchers have used ultrasonography to evaluate the thickness of the ALT free flap. In 2002, Nakayama et al. [6] performed an ultrasonography study of living head and neck cancer patients and reported the mean thickness of skin and subcutaneous tissue of the ALT flap in their population as 7.1 ± 3.4 mm. Aladimi et al. [7] reported a mean thickness of 14.5 ± 4.2 mm for the ALT flap; this relatively high value was probably because the volunteers in their study were all healthy and Americans. Hsu et al. [8] reported a lower mean thickness of 9.8 ± 4 mm in 202 healthy volunteers from Taiwan. These data from Doppler ultrasound studies suggest that the flap thickness varies with ethnic origin and health status and it appears to be less in Asian patients than in Westerners.
There was only one previous study using CTA to assess flap thickness and it was performed in a Western population (106 patients) to assess only the ALT flap [11]. The mean thickness of ALT flaps in men and women in that study were 9.9 and 19.9 mm, respectively, which were comparable with our findings. However, there were no previous publications to assess flap thickness with CTA on other thigh flaps.
Similar to our study, earlier studies have also demonstrated thicker subcutaneous fat in the anterior thigh region in female patients than in male patients [8,11,12,13], and also the ALT flap thickness has been correlated with BMI [8,11,13,14]. In the present study, we have demonstrated for the first time that there exists a correlation between flap thickness and BMI and gender in all thigh flaps studied, including the PAP flap. Moreover, the PAP flap appears to be the least correlated with BMI.
In addition, the difference in thickness of subcutaneous fat between upper and lower parts of the anterior thigh has been reported [12,13]. Nevertheless, to date, there has not been any anthropomorphic analysis of the thickness of PAP as compared to the thickness of ALT or AMT free flaps in the same patient.
The PAP flap has become an ideal choice for autologous tissue breast reconstruction as an alternative to the deep inferior epigastric perforator flap [15]. However, there are few reports regarding its use for intraoral reconstruction [3,4,5]. The main concern in our population could be its greater thickness compared to the ALT flap, but with our results, we can show that there is not much difference when the PAP flap is designed around a distal perforator. Our current results may encourage the decision for harvesting a PAP flap as an alternative to an ALT flap when the indication is made for intraoral reconstruction.
In our study, the population included oncological patients. Nutritional status of these patients could be influencing our final results. Nevertheless, one of the most common reasons for microsurgical reconstruction of the head and neck in an adult patient is head and neck carcinoma. However, future research on correlating nutritional status with skin thickness will be useful in order to clarify the differences between series with healthy and/or head and neck cancer patients.
All thigh flaps, including the PAP flap, tend to be thicker in women and in those patients with high BMI. The thigh flap that is least correlated with BMI is the PAP flap. Besides, the PAP flap thickness is not significantly different from that of the ALT/AMT flaps when the measurement is made over the second perforator of the adductor magnus muscle. Hence, harvesting the PAP flap around a distal perforator makes it easier to obtain a flap as thin as the ALT flap used in the same patient. Because of the similarity in thickness, the PAP flap can be considered in our population to be a good alternative of the ALT flap for intraoral reconstruction.
Received date: March 26, 2019
Accepted date: September 02, 2019
Published date: November 25, 2019
This study adhered to the principles of the Declaration of Helsinki in terms of medical protocols and ethics and was approved by the institutional ethics committee (Reference number 3965) from the Reina Sofia University Hospital, Córdoba, Spain.
The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors report no financial or other conflict of interest relevant to this article, which is the intellectual property of the authors.
Partial content of this manuscript was presented at the 24th Congress of the European Association for Cranio Maxillo Facial Surgery, 18-21 September 2018, Munich, Germany under the title of “Thigh Free Flap Thickness in Western Population: Customizing Free Flaps for Tongue Reconstruction”.
© 2019 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Pedicled anterolateral thigh flap is a versatile option for reconstruction of complex soft tissue defects in varied anatomical regions. Its wide arc of rotation and less donor site morbidity are its added advantages.
Patients with gynecological abdominal wall malignancies can benefit significantly from radical resection and autologous reconstruction. The pedicled anterolateral thigh flap is the preferred donor site, offering a reliable solution to abdominal wall reconstruction in this setting. The satisfactory results should prompt a more aggressive surgical approach for these patients. This article describes the authors' experiences with the abdominal reconstruction following surgical resection of gynecological abdominal wall malignancy using pedicled anterolateral thigh flap.
Division of the lateral plantar artery does not jeopardize the foot circulation because of anastomosis of the lateral plantar artery with the dorsalis pedis artery at the first intermetatarsal space. However, care should be taken with patients with peripheral artery occlusive disease and the flow of dorsalis pedis artery should be confirmed before surgery. Given the advantages of sizable vessel, easy dissection, and proximity to the defect, we believe that the lateral plantar artery might be a valuable option as recipient vessel for lateral plantar forefoot reconstruction.
The authors reviewed the MDCT images to show the number of lymph nodes superior to the saphenofemoral junction. In this study, on average, 3.67 nodes existed. However, there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
The authors proposed a new less invasive island flap, namely the first metatarsal artery capillary perforator flap. The advantages of this flap include the preservation of the first metatarsal artery and the adiposal tissue in the web space, thereby preventing compression around the remaining deep peroneal nerve.
A thin profunda artery perforator flap harvested from the left thigh is shown in this video. Preoperative computed tomographic angiography is used to assess morphology of the perforators and its branches, pedicle length and vertical location of the two branches from the ischial tuberosity. These measurements are translated on to the patient. Locations of both branches are confirmed with a handheld doppler. The authors concluded that preoperative computed tomographic angiography is a useful technique to provide detailed anatomic information on morphology of perforators, course through the septum or muscle above the deep fascia and skin thickness. Computed tomographic angiography allows quick and easy assessment of the whole vascular anatomy of the leg and helps to arrive at the decision about selection of the best flaps based on the characteristics of the defect and on the individual anatomy of the patient.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
This systematic review and meta-analysis provide a pragmatic evaluation of drain-free versus drain-based DIEP flap techniques for breast reconstruction, challenging the traditional reliance on drainage. By analyzing postoperative outcomes, the study highlights the potential for refining surgical strategies to enhance patient comfort and recovery without compromising safety. The findings offer a neutral perspective, suggesting that clinical practice may not necessarily depend on the use of drains. This revelation prompts medical professionals to reassess existing surgical approaches and may catalyze a paradigm shift in postoperative care. Presented with clear narrative and rigorous data analysis, the article encourages readers to consider the broader implications of surgical innovations on patient care protocols.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
Heredero S, Falguera MI, Sanjuan A, Dean A, Solivera J. Comprehensive analysis of profunda artery perforator flap thickness based on CTA. Int Microsurg J 2019;3(3):2. https://doi.org/10.24983/scitemed.imj.2019.00120