Objective: The field of microsurgery is constantly striving for innovative reconstructive techniques that offer optimal outcomes. Among these techniques, the keystone design perforator island flap (KDPIF) has emerged as a prominent solution, garnering substantial attention from surgeons worldwide. Its versatility and simplicity make it a preferred choice for soft tissue reconstruction, regardless of the underlying etiology. In this study, we aimed to share our clinical experience and report on the outcomes of the KDPIF reconstruction process, thereby contributing valuable insights to the existing knowledge base.
Methods: This retrospective study analyzed 115 adult patients who underwent KDPIF reconstruction at our clinic over a 40-month period. Patients included elective cases of soft tissue malignancies and chronic wounds, as well as emergency cases due to trauma-inflicted wounds. The surgical technique involved meticulous flap planning based on the defect's orientation, adhering to relaxed skin tension lines. Outcome measures included flap survival rate, postoperative complications, donor site morbidity, and scar assessment using the Manchester scar scale. By evaluating these parameters, we aimed to assess the efficacy and safety profile of the KDPIF technique, providing valuable insights into its clinical utility and outcomes.
Results: In our study cohort of 115 patients, male individuals constituted 73% of the participants, with an average age of 55.7 years. Notably, our findings unveiled skin malignancies as the prevailing etiology for soft tissue defects. Localization analysis revealed that most defects were situated on the trunk (49.6%), followed by the lower extremity (23.5%). Among the various reconstructive options available, Type II KDPIF emerged as the predominant choice, employed in most cases (n=85), while type IV reconstruction was only required by two patients. Medium-sized defects, ranging from 16 to 50 cm², represented a significant proportion, accounting for 47.8% of cases. Operative procedures exhibited an average duration of 56 minutes, with no significant increase observed for larger defects. Postoperative complications occurred in 13.04% of patients, primarily manifesting as infections and partial flap necrosis, which were predominantly managed conservatively. The average hospital stay was 4.7 days, and at the 6-month follow-up, patients reported no incidences of flap sensitivity issues. Additionally, a mean Manchester scar scale score of 7.8 signified favorable results for the patient cohort.
Conclusion: The KDPIF stands out as an efficient reconstructive technique, capable of addressing soft tissue defects in a single surgical procedure. Notably, its simplicity and expediency contribute to its widespread adoption. Our study reinforces the expanding indications for the use of the KDPIF, further emphasizing its clinical significance. The insights garnered from our clinical experience underscore the favorable outcomes associated with this versatile flap, establishing it as a reliable tool in the armamentarium of soft tissue reconstruction. Future research endeavors are warranted to explore and refine the application of the KDPIF in diverse clinical scenarios.
Soft tissue defects present a significant challenge for plastic surgeons due to their diverse etiology and complex nature, often requiring intricate closure techniques. With the rising incidence of skin cancer and trauma-related defects in recent years, there is an escalating demand for effective defect coverage [1,2]. Surgeons worldwide have long sought an optimal reconstructive method that can accommodate defects of varying sizes and locations, while offering simplicity of execution, minimal complications, and favorable aesthetic and functional outcomes. A pioneering solution emerged in 2003 with the introduction of the local island flap by Behan [3], which rapidly gained global recognition within the field of plastic surgery [4]. Over time, this technique has undergone several advancements and modifications, further enhancing its applicability.
Initially referred to as the arc flap, this ingenious approach earned its current name due to its resemblance to the keystone of archways. The keystone design perforator island flap (KDPIF) stands out among loco regional flaps, boasting remarkable adaptability [3,5-7]. Its design, vascular supply, and mobilization method can all be customized to suit the specific requirements of the defect and the available donor tissue in different anatomical regions [8]. This exceptional flexibility amplifies the flap's utility, empowering surgeons to master advancement, transposition, rotation, and perforator-based reconstructions using a single technique.
The objective of this case series was to present an overview of our extensive experience in employing the KDPIF in our clinical practice thus far. We aimed to delve into the fundamental principles, surgical techniques, and modifications associated with this approach, while exploring its versatility in addressing defects of varying sizes and anatomical regions. Furthermore, we examined the simplicity of its execution, as well as its inherent limitations, offering readers valuable insights into this remarkable reconstructive tool.
Study Design and Patients
In this compelling retrospective investigation, we presented the outcomes of a comprehensive study involving 115 patients who underwent surgical procedures at our clinic. Throughout a continuous duration spanning 40 months, these individuals underwent the implementation of the KDPIF as their preferred modality for reconstructive interventions. All participants included in this study were adults, surpassing the age of 18, who provided informed consent for their respective surgeries. Crucially, they were diligently monitored throughout the postoperative phase for a minimum duration of 6 months.
While the primary focus of elective surgery revolved around patients afflicted with soft tissue malignancies and chronic wounds, the scope of this study also encompassed a subset of cases involving emergency procedures for trauma-induced wounds. By incorporating this diverse patient population, we aimed to provide a comprehensive evaluation of the KDPIF's efficacy across a range of clinical contexts.
Surgical Technique
The flap was meticulously designed to align its long axis parallel to the long axis of the defect, ensuring concordance with the relaxed skin tension lines. This strategic approach minimized tension and promoted mobility, thereby reducing the risk of complications. In the case of upper and lower extremities, a longitudinal excision was generally employed. Surgical excisions were performed as ellipses, with the excision axis parallel to cutaneous nerves, veins, and known vascular perforators. Subsequently, the short axis was measured. The length of the short axis was projected into three points from the edge of the defect, transversally, at a 90° angle to the edge. The three points were then conjoined to get a convex line parallel to the defect edge. When the defect ends were connected, the keystone shape was achieved.
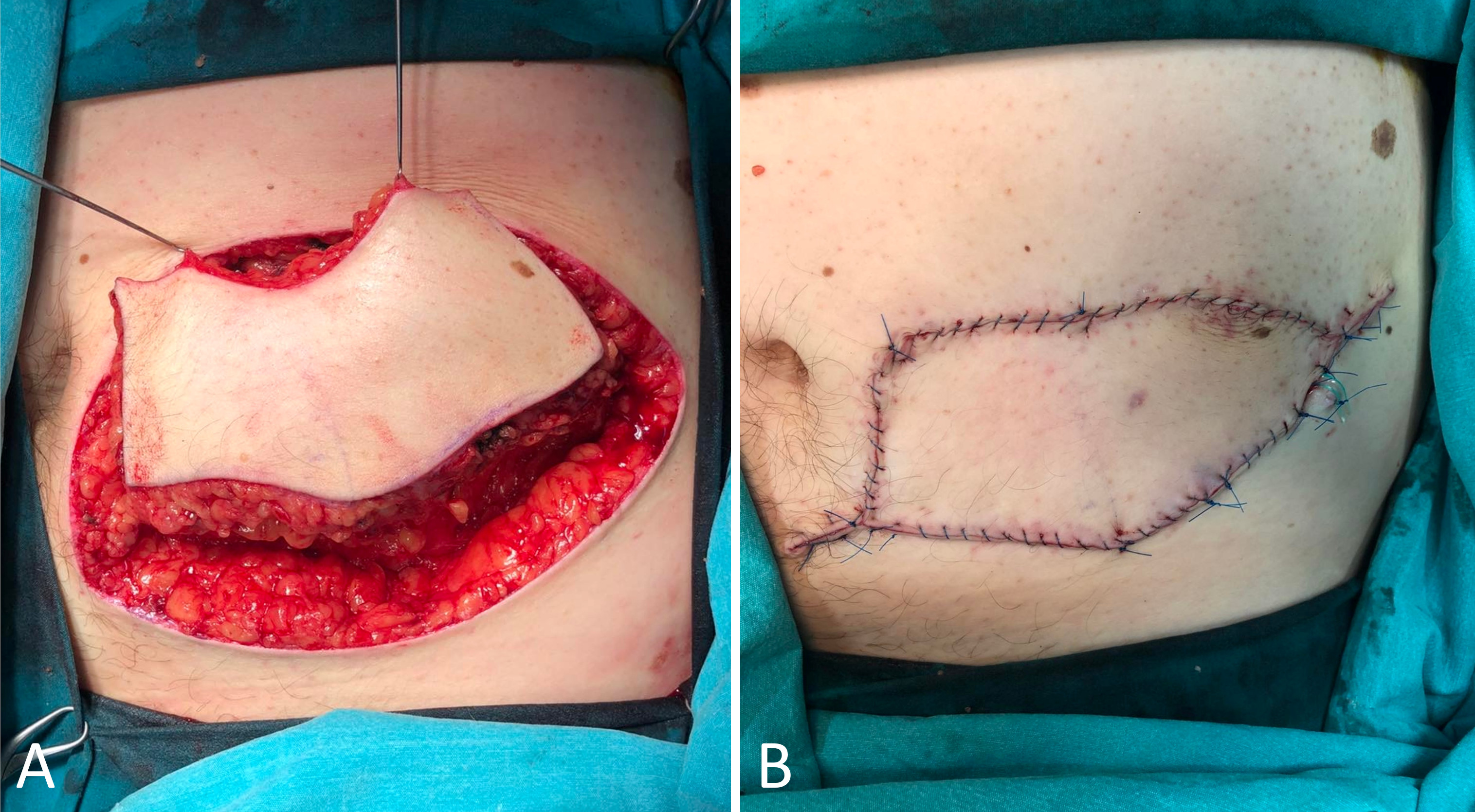
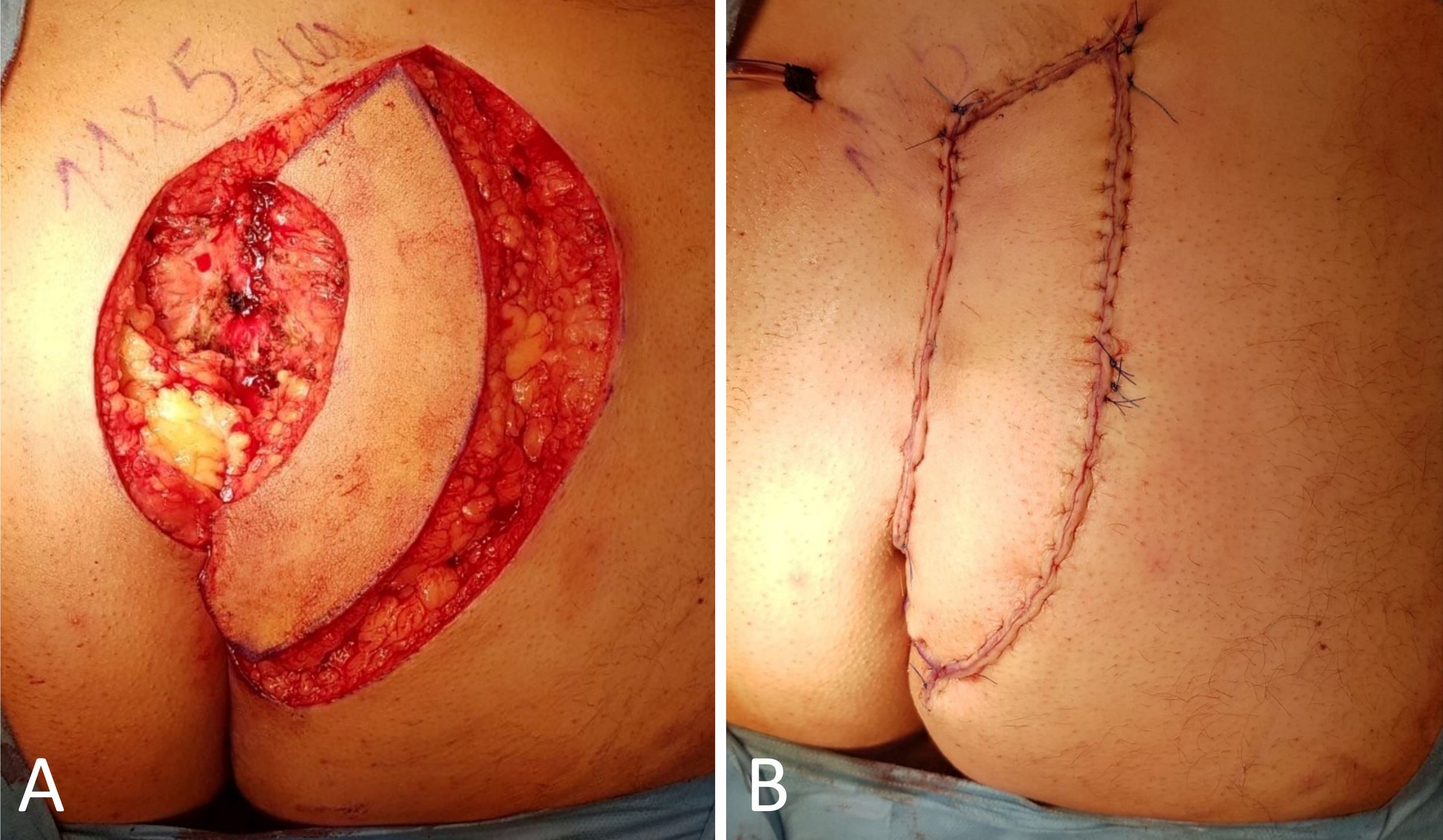
Irrespective of the anatomical location of the defect, the flap was intentionally designed with a minimum width ratio of 1:1 relative to the size of the defect. Following incision of the skin along the marked lines, the subcutaneous tissue was meticulously dissected. The flap, acting as an island, was then mobilized towards the primary defect, and secured with sutures. The outer angles of the flap acted as two V-Y advancement flaps (Figure 1). Depending on the specific case, the island and surrounding tissue may be undermined. Once hemostasis was successfully achieved, the flap was subsequently secured in its intended position through meticulous suturing. The placement of a surgical drain was recommended to optimize postoperative care (Figure 1).
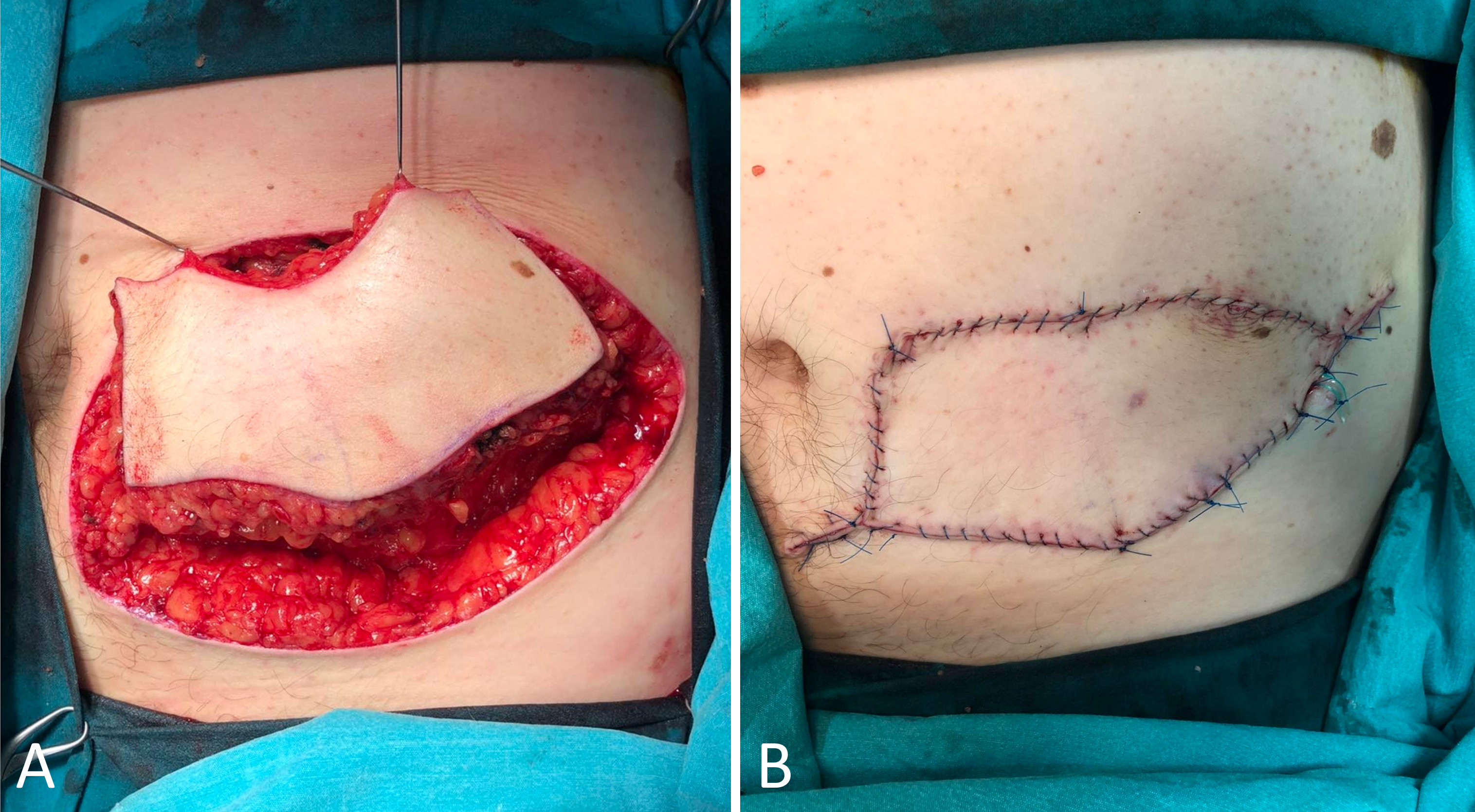
Figure 1. Type IIa keystone design perforator island flap technique for reconstructing tissue defects after melanoma excision from the trunk. (A) The surgical intervention commences by executing precise incisions along the designated markings, coupled with a meticulous dissection of the subcutaneous tissue. Subsequently, the flap, functioning as an island, is skilfully mobilized towards the primary defect. (B) The immediate post-operative results are displayed, demonstrating the effectiveness of Type IIa keystone design perforator island flap technique, which typically involves primary closure of the secondary defect. Two V-Y advancement flaps are formed by the outer angles of the flap, playing a crucial role in the surgical procedure. To optimize postoperative care, the placement of a surgical drain is advised.
Outcome Assessments
In our comprehensive study, we meticulously gathered a diverse array of data encompassing age demographics, gender distribution, etiology, indications for surgery, the specific type of KDPIF employed, and the duration of hospitalization. Our data collection further encompassed key outcome measures such as flap survival rates, rates of complications including necrosis, sensation loss, donor site morbidity, and postoperative pain at the operative site.
To provide a comprehensive assessment, we employed the Manchester scar scale to evaluate scar characteristics. This robust scale evaluates seven distinct scar parameters, including the presence of single or multiple scars, scar size, color, texture, margins, and their relationship to the surrounding skin. The Manchester scar scale score ranges from 4 to 18, with higher scores indicating more unfavorable scar outcomes. Our study leveraged the Manchester scar scale as a valuable tool for postoperative scar assessment, enabling a comprehensive evaluation of the aesthetic and functional aspects of the scars under investigation [9].
Statistical Analysis
A Pearson correlation analysis was conducted to explore the relationship between the size of the defect and the type of flap utilized for reconstruction. All statistical analyses were carried out utilizing a commercially available software package (SPSS version 29.0, SPSS, Inc., Chicago, Ill., USA). Statistically significant findings were determined based on a threshold of P values less than 0.05.
Demographic Insights
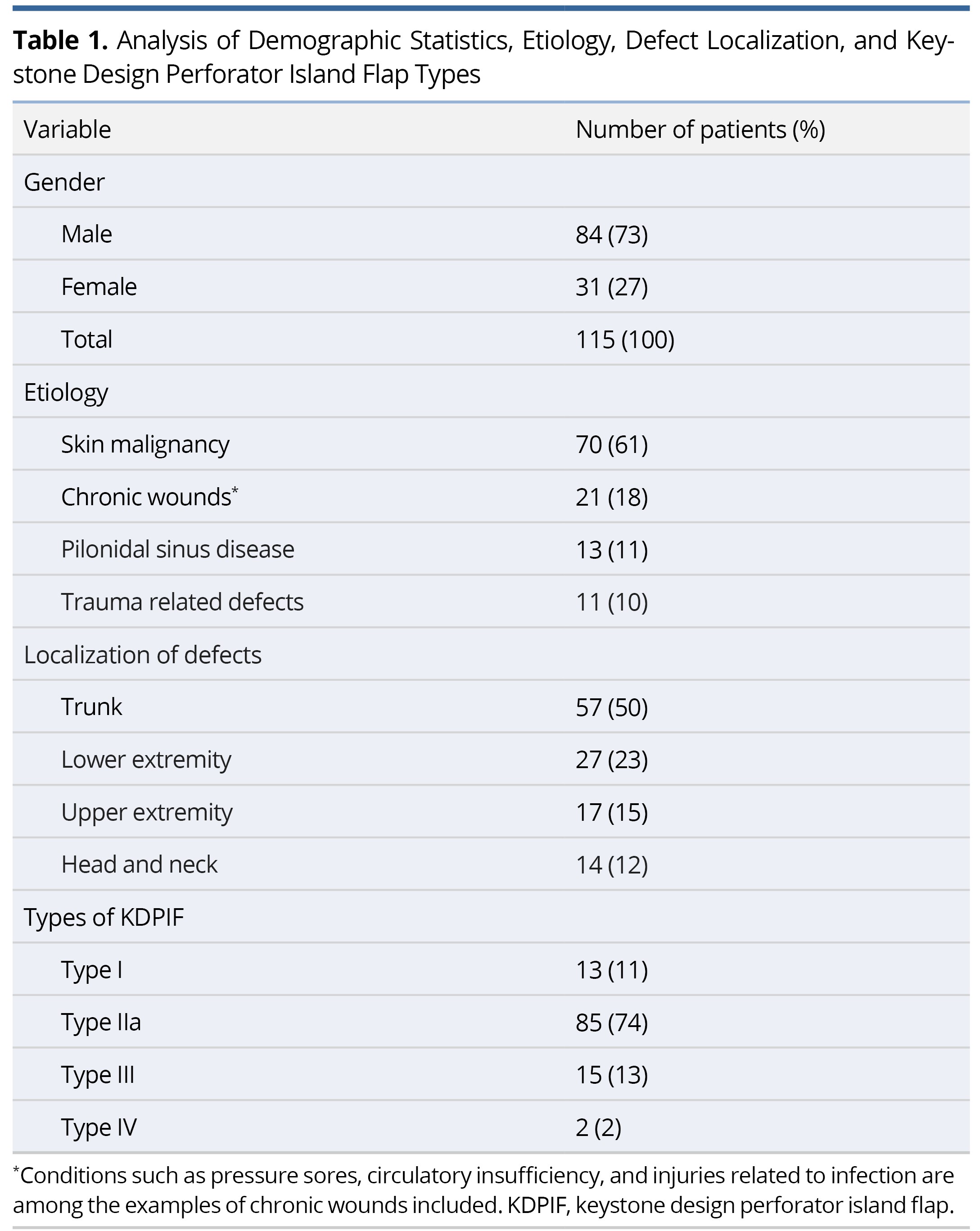
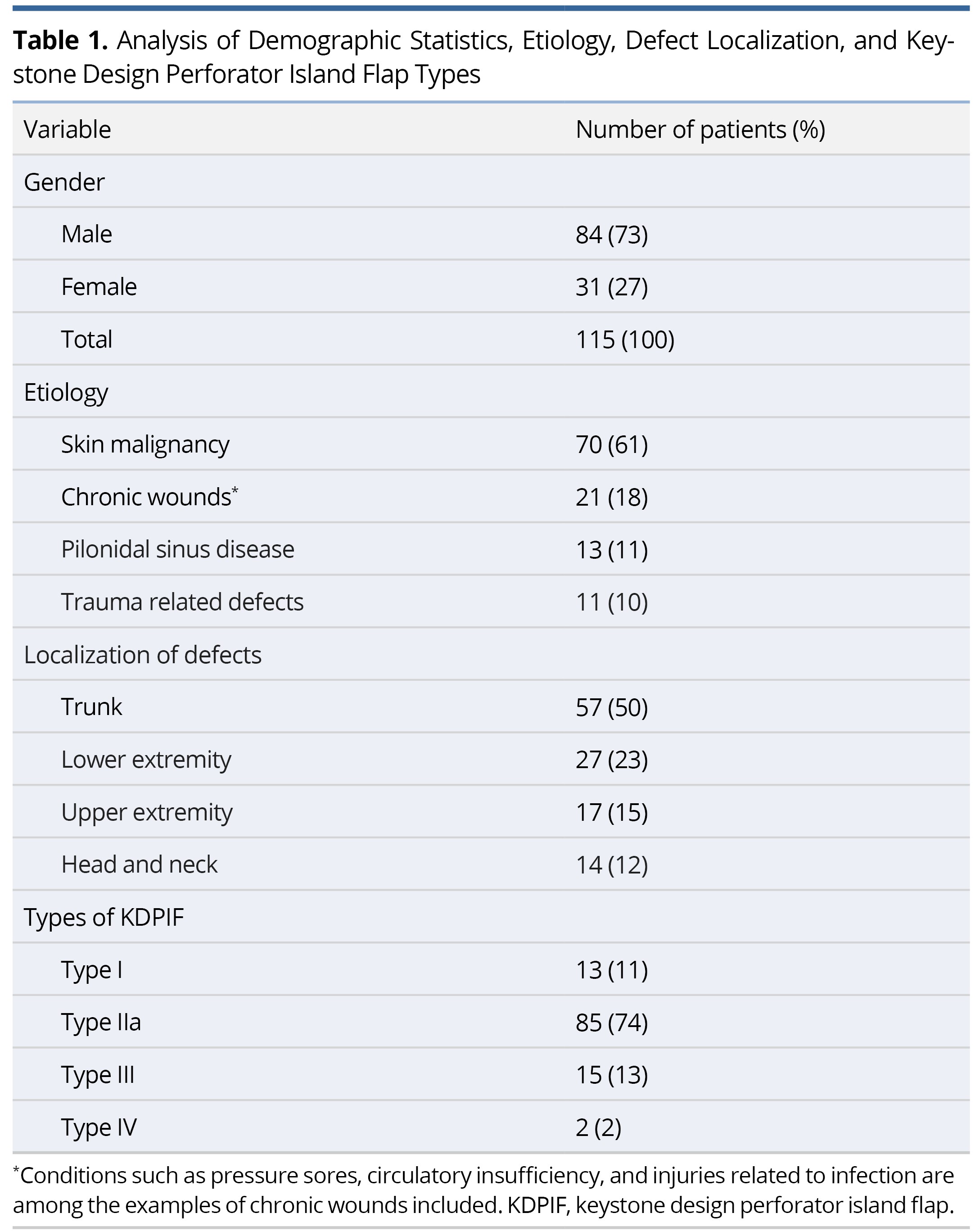
In the context of this investigation, Table 1 provides a thorough and detailed summary encompassing key demographic statistics, the underlying causes of defects, the precise anatomical localization of these defects, and the specific types of KDPIF utilized in the surgical interventions. A diverse cohort of patients was enrolled in our study, comprising a total of 115 individuals who underwent the KDPIF procedure. Notably, 73% of the patients were male (n=84), while the remaining 27% (n=31) were female. The average age of the patients was determined to be 55.7 years, with a notable age range spanning from 18 to 88 years. Patients were meticulously screened for pre-existing conditions, including diabetes, peripheral artery disease, and other cerebrovascular ailments. It was revealed that 35.6% of the patients exhibited one or more of these comorbidities, particularly diabetes.
Etiologies of Defects
Among the diverse range of factors, the most prevalent cause of defects was the excision of skin malignancies, accounting for a substantial proportion of cases (n=70). Following this, chronic wounds attributed to pressure sores, circulatory insufficiency, and infection-related complications emerged as significant contributors (n=21). Additionally, we observed a noteworthy occurrence of defects resulting from pilonidal sinus disease (n=13) and trauma-related incidents (n=11). This comprehensive evaluation of the underlying etiologies offers valuable insights into the pathogenesis of these conditions and further underscores the significance of KDPIF in managing such complex scenarios.
Distribution of Defects
Through rigorous analysis, we discovered distinct patterns in the distribution of these defects, shedding light on their preferential occurrence across different regions of the body. Remarkably, the trunk emerged as the most prevalent site for defects, representing 49.6% of cases. Following closely behind, the lower extremities accounted for 23.5% of defects, while the upper extremities constituted 14.8%. Lastly, the head and neck region comprised 12.2% of the cases studied. These findings underscore the nuanced anatomical distribution of defects and lend valuable insights for surgical planning and decision-making.
Types of KDPIF
Among the cases examined, the KDPIF with division of the deep fascia, specifically type IIa, was predominantly employed by our surgeons, accounting for the majority at 73.9% (85 cases). A minor proportion of cases, comprising 4 patients, utilized the Ω-modification. Closure was accomplished using type III, the double keystone flap, in 13% of cases (15 cases). This technique was particularly advantageous in situations where skin laxity was inadequate, such as around extensor sides of joints (shoulder, elbow) and areas with skin overlaying bone (presternal region, shin). A small portion of patients underwent reconstruction with type IV (1.7%) or type I (11.3%) KDPIF.
Defect Size Correlated with Flap Type
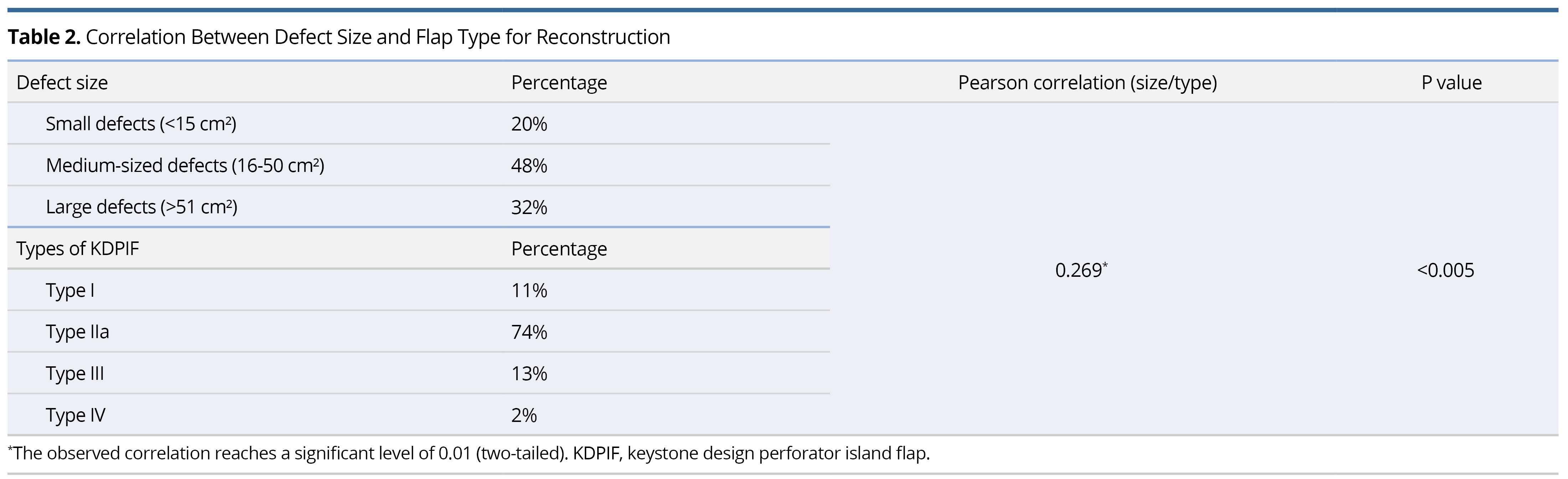
To facilitate a systematic evaluation, the cases were classified into three groups based on the size of the skin and soft tissue defects: small defects (<15 cm²), medium-sized defects (16-50 cm²), and large defects (>51 cm²). The range of defects encountered was broad, spanning from 3.25 cm² to 500 cm². Medium-sized defects accounted for the largest proportion at 47.8%, followed by large defects at 32.2%, and small defects at 20%. Notably, a significant correlation was observed between the size of the defect and the type of flap employed for reconstruction (P <0.005, Table 2). Most medium-sized defects were successfully addressed using type II flaps.
Operative Time
The study revealed an impressive finding regarding the mean operative time required for these procedures. Surprisingly, regardless of the size of the defects encountered, the average duration was a mere 56 minutes. Even when faced with large defects, the surgical team successfully completed the operation within a maximum time limit of 120 minutes.
Postoperative Complications
Postoperative complications were relatively infrequent, affecting only 13.04% of the patients (n=15). Infections were identified in 3 patients (2.6%), although no statistically significant association was established between infection occurrence and diabetes. All infected wounds were diligently managed through local wound care and administration of appropriate antibiotics. Hematomas were observed in 10 patients, which were resolved either conservatively or through drainage. Notably, all wounds achieved primary healing without further complications. Partial flap necrosis was observed in 2 patients with chronic wounds below the knee due to vascular insufficiency.
Length of Hospital Stay
The average length of hospital stay was 4.7 days (ranging from 1 to 30 days). Most patients (60%) were discharged within five days, while a mere 1.7% required a hospitalization period exceeding 15 days. Importantly, all patients left our clinic in a satisfactory general health condition.
Suture Removal
Precise timing for suture removal plays a pivotal role in the postoperative recovery process after flap surgery. In this study, the removal of sutures was meticulously performed within a specific timeframe of 7 to 18 days, customized to suit the site of reconstruction.
Sensitivity Evaluation
This longitudinal study aimed to assess sensory integrity and scar outcomes in patients who underwent flap surgery. At the 6-month follow-up, none of the patients reported impaired sensitivity of the flap, indicating a successful preservation of sensory function. The utilization of the Manchester scar scale in assessing postoperative scars resulted in an average score of 7.8, indicating a positive outcome.
KDPIF surgery is a widely used technique for tissue reconstruction, offering numerous benefits in terms of vascularity and tissue preservation. Understanding the underlying physiology and anatomical considerations is crucial for successful outcomes. In this article, we elucidate the intricate vascular network associated with the KDPIF and discuss the optimal design strategies for different anatomical regions.
Versatile KDPIF: Reconstructive Innovations
The KDPIF stands out among its counterparts as an exceptionally versatile technique in the field of reconstructive surgery. The nomenclature derives from its resemblance to the central keystone element found in the architectural design of a Roman arch. The KDPIF, at its core, represents a composite structure comprising two conjoined V-Y advancement flaps, thereby qualifying as a multi-perforator, fasciocutaneous advancement flap [3,7].
The distinguishing feature of this flap resides in its capacity to simulate the concurrent advancement of three separate flaps, all converging towards the center of the defect. This remarkable attribute is achieved through the progression of an island of tissue, which adheres to the body via a specific region known as the pedicular area. The pedicular area serves as the conduit for the transit of crucial vascular and neural components that sustain the vitality of the flap [4-6,10-12].
Crucially, the blood supply to the KDPIF follows the principle of angiosome, ensuring its robust vascularization. The flap is supplied by multiple vascular perforators that are selectively chosen based on the flap's location and size. It is noteworthy that these perforators are presumed rather than explicitly dissected for identification. The reliance on this extensive blood supply guarantees a high rate of flap survival [4-6,10-12].
Furthermore, the innervation of the KDPIF is self-contained within the island of tissue, eliminating the need for nerve repair to achieve sensory function. This intrinsic innervation capability simplifies the surgical procedure and contributes to the overall success of the flap [4-6,10-12].
Perforator Preservation in KDPIF Mobilization
The keystone flap's islanded structure is achieved through a circumferential incision, creating a distinct separation between the subdermal plexus and surrounding tissue. As a result, the flap relies on one or multiple perforating vessels for its blood supply, obtained from a broad subcutaneous bed located directly beneath the flap. While ensuring the preservation of the subcutaneous bed's attachment to the deeper fascia and muscles, utmost caution is exercised to avoid any disturbance to the nourishing septocutaneous and musculocutaneous perforators that sustain the integrity of the overlying skin island. Due to the design of the keystone flap, the underlying perforators are never skeletonized or identified during flap mobilization.
Optimal Design Strategies
To facilitate precise keystone flap design, Behan has advocated for the use of a dermatomal roadmap [5,10-12]. By aligning the long axis of the excision with the regional dermatomal distribution, the primary lesion can be oriented appropriately. In the upper and lower extremities, as well as the trunk, dermatomal segments predominantly run longitudinally. However, in the head and neck region, a distinct vascularity exists, necessitating careful consideration during flap design. Unlike the extremities and trunk, where dermatomal segments align longitudinally, the chest, abdomen, and pelvis exhibit transverse dermatomal segments. This anatomical variation must be considered when planning KDPIF surgery in these regions. Attention to detail and understanding the vascular anatomy within each specific region are vital for optimal outcomes.
Precise Match in Skin Color and Texture
One of the primary advantages of KDPIF is its ability to utilize donor tissue from adjacent skin and soft tissue, ensuring a precise match in skin color, texture, and contour reconstruction [5,12]. This remarkable feature enhances the cosmetic outcome of the procedure and contributes to patient satisfaction. By aligning with relaxed skin tension lines, the flap's primary axis is meticulously planned parallel to the major axis of the defect, optimizing its overall effectiveness.
Versatile Application and Simplicity
The remarkable versatility of KDPIF renders it an optimal selection for addressing a diverse array of abnormalities that extend to the deep fascia. These encompass conditions resulting from an assortment of factors, including skin cancer, pressure ulcers, combustion, frostbites, and infective necrosis. Surgeons often favor this technique due to its simplicity and ease of repeatability. Moreover, the execution of the flap technique is notably more straightforward in areas of the body characterized by skin laxity, such as the trunk, gluteal region, and thigh, in contrast to the knee and distal leg, where its application presents greater challenges [13]. Research has demonstrated that KDPIF is also highly effective in repairing facial defects.
Advantages and Efficacy Explored
Extensive research has highlighted the multitude of advantages associated with KDPIF technology. Noteworthy benefits include its uncomplicated defect-adaptive design, ease of repeatability, reliable vascular supply, and efficient operative duration, among others. When considering outcomes and post-operative complications, the utilization of KDPIF technology emerges as a notably safer alternative compared to most local and non-local methods. These advantages, however, are achieved while maintaining a low incidence of donor site morbidity [5,10]. The findings of our study further supported the effectiveness of KDPIF in successfully reconstructing even large defects while primarily achieving closure at the donor site. Furthermore, at a 6-month follow-up, none of the patients reported impaired sensitivity of the flap, indicating a successful preservation of sensory function. Additionally, the use of the Manchester scar scale in assessing postoperative scars resulted in an average score of 7.8, indicating a positive outcome.
Plastic surgery has made significant advancements in repairing soft tissue defects since the introduction of the KDPIF. This technique, which involves reorienting local tissue, has revolutionized the closure of large defects. Its ingenuity lies in its various distinctive capabilities. Firstly, the KDPIF allows for the replacement of damaged tissue with similar tissue, resulting in favorable aesthetic outcomes. Moreover, this technique allows for the prevention of dog ears, which refers to the formation of excess tissue that bunches up during the closure of a wound. It also allows for the preservation of multiple perforator vessels, ensuring the survival of the flap. Another advantage is that only one operative field is required when using the KDPIF. The utilization of KDPIF in this context not only decreases the technical complexity but also mitigates the morbidity associated with the donor site. Furthermore, it has the potential to effectively close larger defects. Lastly, the utilization of KDPIF in reconstructive procedures brings notable benefits, including shorter operative times and hospital stays, which contribute to a more efficient recovery process. Our study confirmed these advantages, revealing impressively short mean operative times of 56 minutes irrespective of defect size. Hospital stays averaged 4.7 days, with most patients discharged within five days, all without any negative impact on their health. These findings underscore the efficacy and effectiveness of KDPIF in achieving favorable outcomes and optimizing patient care.
Types of KDPIF: An In-Depth Exploration
In the field of reconstructive surgery, the search for optimal closure techniques to address complex defects has fostered the evolution of several procedures, including deep fascia release, undermining of adjacent wound borders, and skin graft insertion. Remarkably, the KDPIF has emerged as a prominent choice due to its versatility and reliability. This article provides an in-depth exploration of KDPIF by illuminating the four distinct types (Type I to IV) that have arisen because of innovative adaptations and advancements in this specialized area.
Type I KDPIF
Type I KDPIF technique involves a fusiform excision of the primary lesion and the creation of a neighboring flap with the same width as the defect. Mobilization is enhanced by selecting the side with greater tissue laxity. Preservation of veins and nerves is emphasized during tissue undermining. Flap closure employs V-Y closure of the terminal portions, enabling concurrent closure of the defect and donor site. Significantly, type I KDPIF stands out from other variants by preserving the complete integrity of the deep fascia.
Type II KDPIF
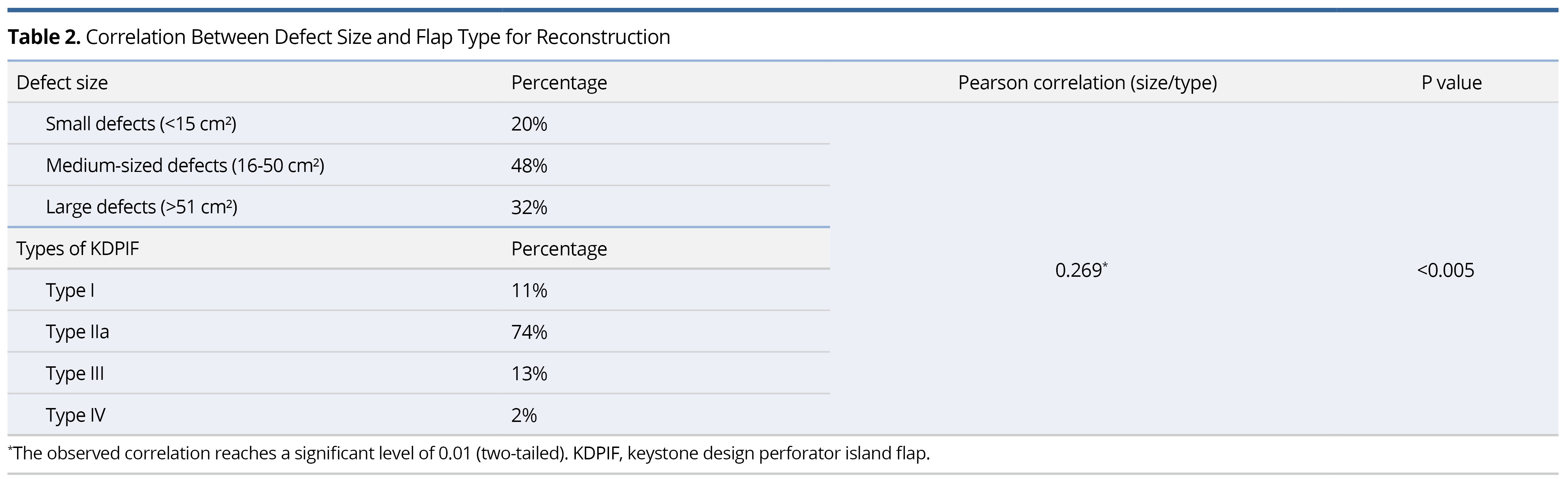
Under specific circumstances where additional mobilization of the flap becomes necessary to achieve primary closure of the donor site, the Type II KDPIF assumes its significance. The outer curvilinear border of the flap becomes the focal point of action as the deep fascia is incised. Notably, the classification of Type II further branches into two subtypes: Type IIa and Type IIb. The determinant factor for this division lies in the requirement of a skin graft for secondary donor site reconstruction. Type IIa typically involves primary closure of the secondary defect (Figure 1), while Type IIb incorporates a splint skin graft (Figure 2).
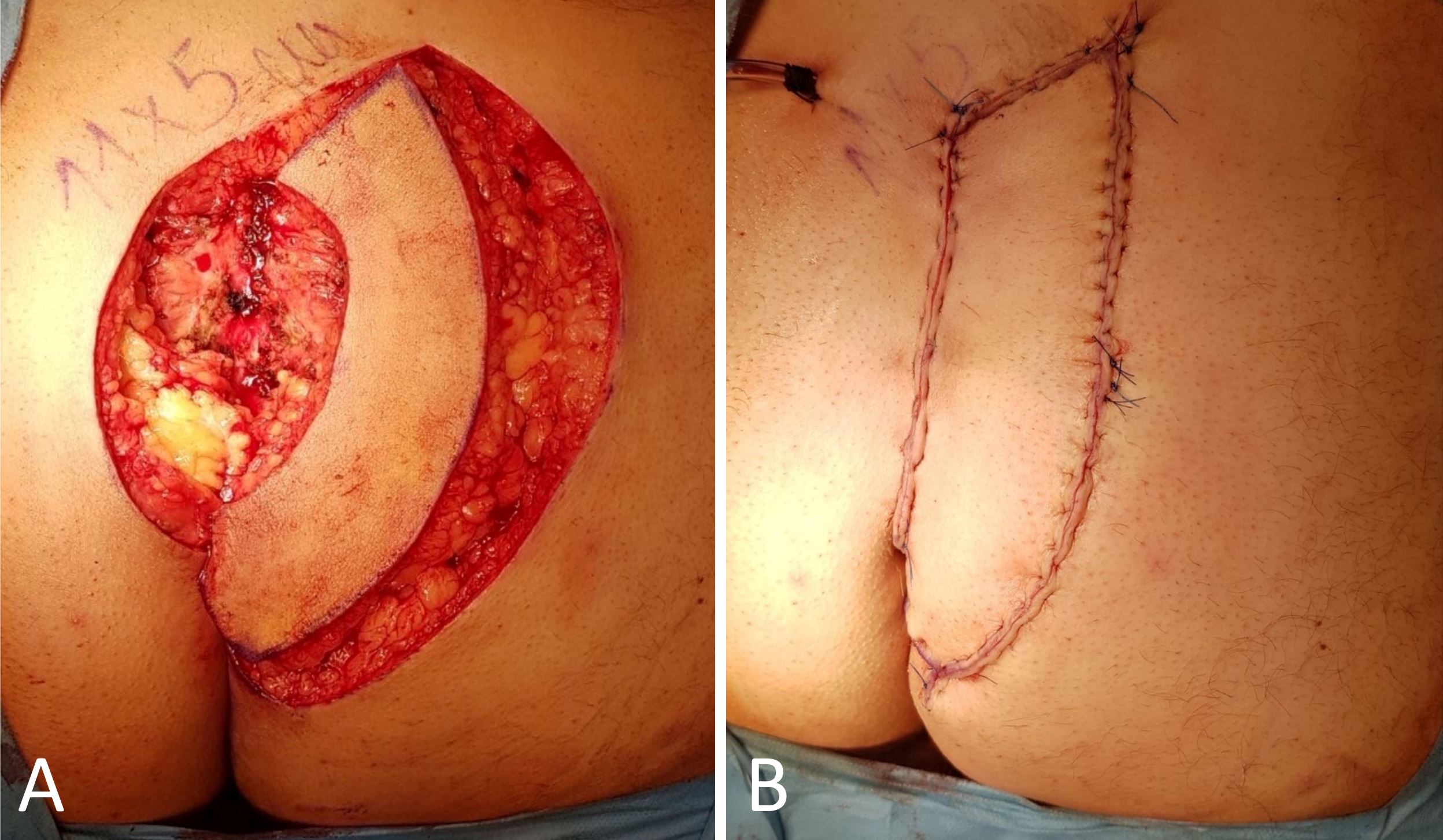
Figure 2. Type IIb keystone design perforator island flap for the reconstruction of post-excisional defects arising from pilonidal sinus disease in the gluteal region. (A) The Type II keystone flap technique entails the surgical division of the deep fascia within the flap. (B) The immediate post-operative outcomes demonstrate the favorable results attained through the procedure. Instead of opting for primary closure, the donor site of the flap is effectively addressed by employing skin grafting. Significantly, there have been no documented cases of disease relapse during the subsequent follow-up period, underscoring the favorable long-term outcomes of the procedure.
Type III KDPIF
In scenarios involving larger ablative defects or regions of the body characterized by inherent soft tissue laxity, the Type III KDPIF serves as an invaluable tool. This type comprises two opposing keystone flaps meticulously designed to envelop a central surgical defect, allowing for a comprehensive and harmonious reconstruction.
Type IV KDPIF
Originating from the groundbreaking work of Behan, the Type IV KDPIF demonstrates its utility by enabling the rotation and/or advancement of the flap into an adjacent surgical defect. A noteworthy aspect of this type is the substantial undermining of up to one-half to two-thirds of its subcutaneous base, facilitating its maneuverability. The type IV flap receives its vascular supply from perforators that originate within the unelevated part of the flap. These perforators traverse through both the subdermal plexus and the suprafascial adipose tissue plexus.
Selecting a KDPIF type: key considerations
The selection of the appropriate KDPIF type for reconstructive procedures relies on various crucial factors, including the defect size and the laxity of the surrounding skin. Type I KDPIF often proves sufficient for successful reconstruction in cases involving smaller defects. However, larger defects in the trunk and gluteal region necessitate the utilization of Type II KDPIF, which offers a robust solution. Our study revealed a significant correlation between the defect size and the flap type employed for reconstruction, as indicated in Table 2. Medium-sized defects were effectively addressed using Type II flaps. Additionally, KDPIF presents inherent advantages such as reduced operative time and avoidance of microsurgical techniques, making it a favorable alternative to free flaps in appropriate clinical scenarios.
Innovative Reconstruction for Complex Defects
The KDPIF, utilizing the abundant blood supply and numerous perforators in the head and neck region, offers a safe and effective method for elevation, allowing for various adaptations to meet the diverse needs of reconstruction. Notably, this innovative approach demonstrates promising results in addressing challenging groin defects and providing coverage for vascular prostheses following soft tissue infections. In our clinical experience, we successfully employed the KDPIF to reconstruct post-excisional defects resulting from pilonidal sinus disease in the gluteal region, with no reported instances of disease relapse during the subsequent follow-up period (Figure 2).
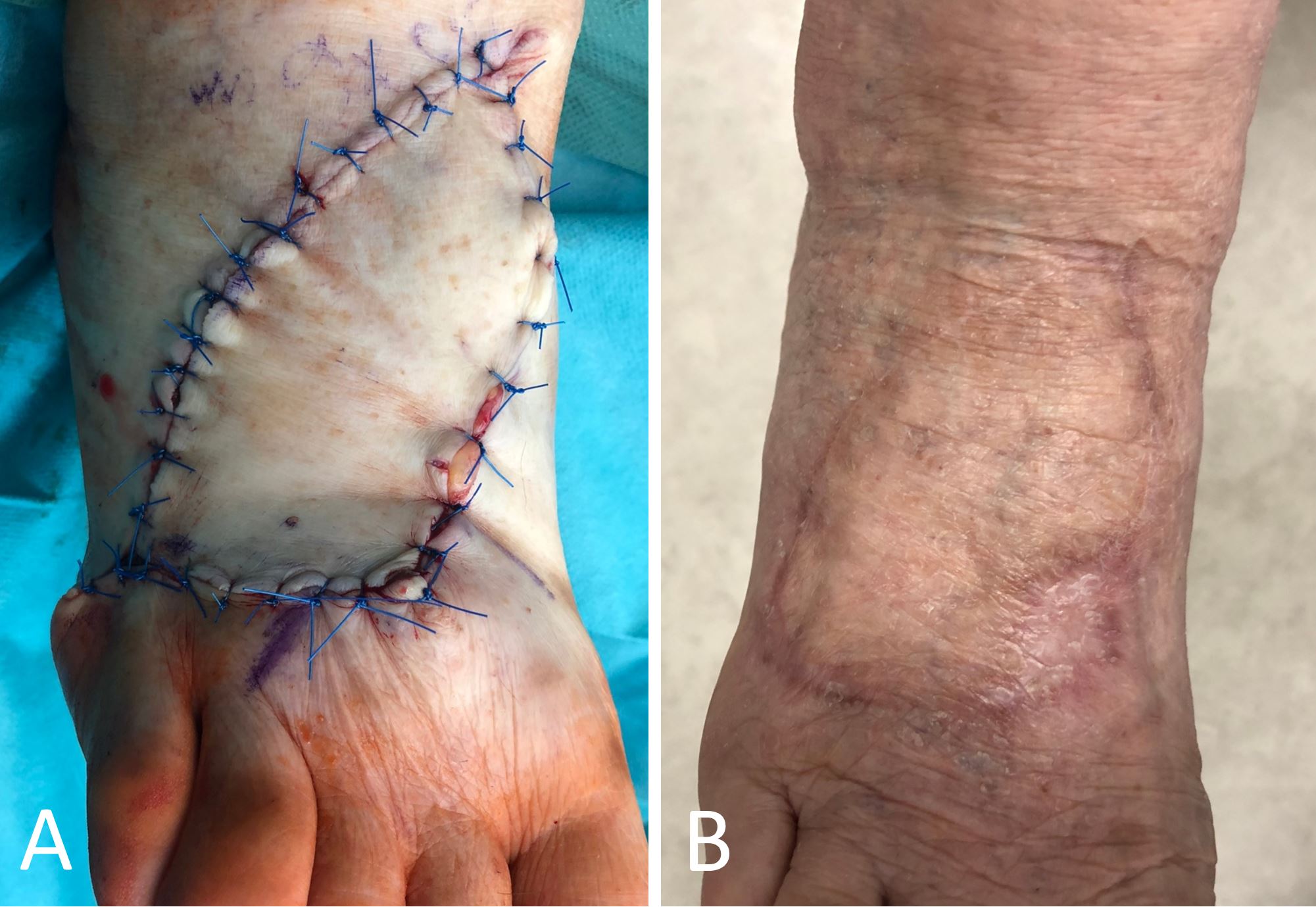
Among the complexities encountered in reconstruction, lower limb defects present formidable challenges due to limited vascularization and skin laxity. Traditionally, free tissue transfer has been the preferred option for these cases. However, both our study and others have highlighted the reliability of the KDPIF as a viable solution for similar indications or defect sizes, even extending its application to foot reconstruction, where utilizing compatible tissue proves most advantageous (Figure 3) [13-16].
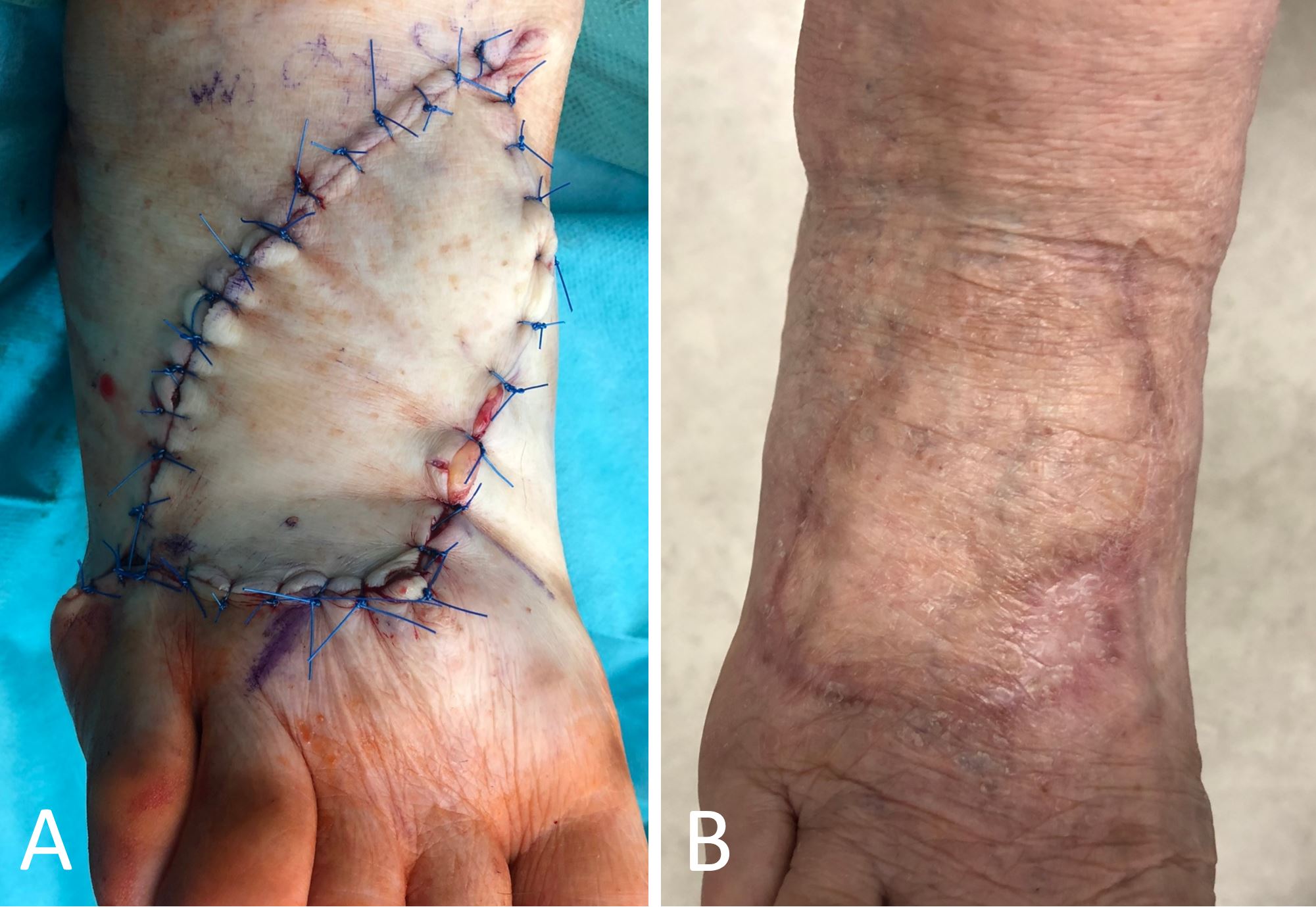
Figure 3. Type IIa keystone design perforator island flap technique for foot reconstruction. (A) Immediate post-operative outcomes. (B) One-year post-reconstruction results. Lower limb defects pose significant complexities in the realm of reconstruction, primarily due to limited vascularization and skin laxity. The findings of our study strongly underscore the dependable nature of the keystone design perforator island flap as an effective and practical solution, expanding its applicability to the realm of foot reconstruction.
Optimizing Reconstruction Outcomes
The underlying cause of a defect has a pivotal impact on the outcomes of reconstructive procedures following tumor resection. Our study demonstrated that among various contributing factors, the excision of skin malignancies emerged as the predominant etiology, comprising a significant portion of cases (n=70, 61%). Choosing local tissue replacement following the removal of malignancies presents a distinct advantage by enabling radiation therapy on healthy skin, thereby augmenting the overall outcome.
Special considerations are necessary for lower limb trauma defects due to the risk of perforator damage [13,15]. Doppler ultrasound is a valuable tool for preoperative assessment, allowing precise evaluation of the perforators and aiding in surgical planning.
Moreover, patients with comorbidities such as diabetes or peripheral vascular disease necessitate careful management. In our study, patients underwent meticulous screening for pre-existing conditions, including diabetes, peripheral artery disease, and other cerebrovascular ailments. The findings revealed that 35.6% of the patients presented with one or more of these comorbidities, with diabetes being particularly prevalent. While patients with vascular insufficiency may face an increased risk of dehiscence or flap necrosis, KDPIF remains a viable option, especially for elderly patients [17,18].
Constraints of the KDPIF
The multi-perforator nature of the KDPIF eliminates the need for extensive dissection of individual perforators, thus reducing the requirement for postoperative monitoring. This streamlined approach allows for remote check-ups and promotes convenient wound care at home. However, it is important to acknowledge certain limitations. The KDPIF is unsuitable as a fascio musculocutaneous flap when addressing abnormalities that necessitate bone replacement. Furthermore, the present research lacks sufficient evidence concerning successful intraoral and intranasal coverage [19,20]. Preservation of the vascular perforators is crucial for the survival of the flap, as traumatic or surgical injury to the donor site tissue compromises its efficacy [2,3,17,18].
Study Limitations
This study highlighted the remarkable adaptability, practicality, and cosmetic benefits of the KDPIF, along with its low complication rate, distinguishing it from randomly selected perforators or flaps. Nevertheless, it is crucial to acknowledge the limitations inherent in this study. Firstly, the lack of comprehensive comparisons between the KDPIF and other random perforators or flaps warrants further investigation to provide a more comprehensive understanding of their relative efficacy and applicability. Additionally, the generalizability of the findings may be limited due to the specific patient population and sample size examined in this study. It is essential to replicate these findings in larger and more diverse cohorts to establish broader validity. Furthermore, the long-term outcomes and potential complications of the KDPIF approach should be evaluated through extended follow-up periods to ensure a comprehensive assessment of its effectiveness and safety. Future studies should also consider exploring the cost-effectiveness and patient-reported outcomes associated with the KDPIF compared to alternative techniques. By addressing these limitations, future research can provide valuable insights and contribute to the ongoing advancement of reconstructive strategies.
The KDPIF offers remarkable adaptability, practical and cosmetic benefits, and a low complication rate. It serves as an efficient reconstructive technique, allowing for single-stage surgery and demonstrating simplicity and expediency. The expanding indications for its use further highlight its clinical significance. The satisfactory aesthetic results observed during follow-up support its favorable outcomes. Notably, the KDPIF does not necessitate microsurgery or additional equipment, which is advantageous in terms of cost-effectiveness, particularly for healthcare systems in emerging countries. Overall, the KDPIF represents a suitable reconstructive solution with wide applicability and potential economic benefits.
Received date: September 02, 2022
Accepted date: May 28, 2023
Published date: June 14, 2023
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills in order to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2023 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
The communication among international microsurgeons have switched from one direction (from paper, textbook) to multiway interactions through the internet. The authors believe the online platform will play an immensely important role in the learning and development in the field of microsurgery.
Traditionally, suturing techniques have been the mainstay for microvascular anastomoses, but owing to its technical difficulty and labour intensity, considerable work has gone into the development of sutureless microvascular anastomoses. In this review, the authors take a brief look at the developments of this technology through the years, with a focus on the more recent developments of laser-assisted vascular anastomoses, the unilink system, vascular closure staples, tissue adhesives, and magnets. Their working principles, with what has been found concerning their advantages and disadvantages are discussed.
Prof. Koushima, president of World Society for Reconstructive Microsurgery, proposes an innovative concept and technique of the multi-stage ‘Orochi’ combined flaps (sequential flaps in parallel). The technique opens a new vista in reconstructive microsurgery.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
Authors discuss a silicone tube that provides structural support to vessels throughout the entire precarious suturing process. This modification of the conventional microvascular anastomosis technique may facilitate initial skill acquisition using the rat model.
PEDs can be used as alternative means of magnification in microsurgery training considering that they are superior to surgical loupes in magnification, FOV and WD ranges, allowing greater operational versatility in microsurgical maneuvers, its behavior being closer to that of surgical microscopes in some optical characteristics. These devices have a lower cost than microscopes and some brands of surgical loupes, greater accessibility in the market and innovation plasticity through technological and physical applications and accessories with respect to classical magnification devices. Although PEDs own advanced technological features such as high-quality cameras and electronic loupes applications to improve the visualizations, it is important to continue the development of better technological applications and accessories for microsurgical practice, and additionally, it is important to produce evidence of its application at surgery room.
Avulsion injuries and replantation of the upper arm are particularly challenging in the field of traumatic microsurgery. At present, the functional recovery of the avulsion injuries upper arm after the replantation is generally not ideal enough, and there is no guideline for the surgeries. The aim of this study was to analyze the causes of failure of the upper arm replantation for avulsion injuries, summarize the upper arm replantation’s indications, and improve the replantation methods.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
The implications of rebound heparin hypercoagulability following cessation of therapy in microsurgery is unreported. In this article the authors report two cases of late digit circulatory compromise shortly after withdrawal of heparin therapy. The authors also propose potential consideration for changes in perioperative anticoagulation practice to reduce this risk.
In a cost-effective and portable way, a novel method was developed to assist trainees in spinal surgery to gain and develop microsurgery skills, which will increase self-confidence. Residents at a spine surgery center were assessed before and after training on the effectiveness of a simulation training model. The participants who used the training model completed the exercise in less than 22 minutes, but none could do it in less than 30 minutes previously. The research team created a comprehensive model to train junior surgeons advanced spine microsurgery skills. The article contains valuable information for readers.
The loupe plays a critical role in the microsurgeon's arsenal, helping to provide intricate details. In the absence of adequate subcutaneous fat, the prismatic lens of the spectacle model may exert enormous pressure on the delicate skin of the nasal bone. By developing a soft nasal support, the author has incorporated the principle of offloading into an elegant, simple yet brilliant innovation. A simple procedure such as this could prove invaluable for microsurgeons who suffer from nasal discoloration or pain as a result of prolonged use of prismatic loupes. With this technique, 42% of the pressure applied to the nose is reduced.
An examination of plastic surgery residents' experiences with microsurgery in Latin American countries was conducted in a cross-sectional study with 129 microsurgeons. The project also identifies ways to increase the number of trained microsurgeons in the region. The authors claim that there are few resident plastic surgeons in Latin America who are capable of attaining the level of experience necessary to function as independent microsurgeons. It is believed that international microsurgical fellowships would be an effective strategy for improving the situation.
This comprehensive review article presents a profound exploration of critical facets within the realm of microsurgery, challenging existing paradigms. Through meticulous examination, the authors illuminate the intricate world of microangiosomes, dissection planes, and the clinical relevance of anatomical structures. Central to this discourse is an exhaustive comparative analysis of dermal plexus flaps, meticulously dissecting the viability and potential grafting applications of subdermal versus deep-dermal plexi. Augmenting this intellectual voyage are detailed illustrations, guiding readers through the intricate microanatomy underlying skin and adjacent tissues. This synthesis of knowledge not only redefines existing microsurgical principles but also opens new frontiers. By unearthing novel perspectives on microangiosomes and dissection planes and by offering a comparative insight into dermal plexus flaps, this work reshapes the landscape of microsurgery. These elucidations, coupled with visual aids, equip practitioners with invaluable insights for practical integration, promising to propel the field of microsurgery to unprecedented heights.
This article presents a groundbreaking surgical approach for treating facial paralysis, focusing on the combination of the pronator quadratus muscle (PQM) and the radial forearm flap (RFF). It addresses the challenges in restoring facial functions and skin closure in paralysis cases. The study's novelty lies in its detailed examination of the PQM's vascular anatomy when combined with the RFF, a topic previously unexplored. Through meticulous dissections, it provides crucial anatomical insights essential for enhancing facial reanimation surgeries, offering significant benefits in medical practices related to facial reconstruction and nerve transfer techniques.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
Division of the lateral plantar artery does not jeopardize the foot circulation because of anastomosis of the lateral plantar artery with the dorsalis pedis artery at the first intermetatarsal space. However, care should be taken with patients with peripheral artery occlusive disease and the flow of dorsalis pedis artery should be confirmed before surgery. Given the advantages of sizable vessel, easy dissection, and proximity to the defect, we believe that the lateral plantar artery might be a valuable option as recipient vessel for lateral plantar forefoot reconstruction.
The authors reviewed the MDCT images to show the number of lymph nodes superior to the saphenofemoral junction. In this study, on average, 3.67 nodes existed. However, there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
The authors proposed a new less invasive island flap, namely the first metatarsal artery capillary perforator flap. The advantages of this flap include the preservation of the first metatarsal artery and the adiposal tissue in the web space, thereby preventing compression around the remaining deep peroneal nerve.
The ALT and AMT flaps are the most commonly used thigh free flaps for intraoral reconstruction. Recently, PAP flap has been proposed as an alternative. This study aimed to compare the thickness of these thigh flaps and to identify the factors influencing flap thickness in our population.
A thin profunda artery perforator flap harvested from the left thigh is shown in this video. Preoperative computed tomographic angiography is used to assess morphology of the perforators and its branches, pedicle length and vertical location of the two branches from the ischial tuberosity. These measurements are translated on to the patient. Locations of both branches are confirmed with a handheld doppler. The authors concluded that preoperative computed tomographic angiography is a useful technique to provide detailed anatomic information on morphology of perforators, course through the septum or muscle above the deep fascia and skin thickness. Computed tomographic angiography allows quick and easy assessment of the whole vascular anatomy of the leg and helps to arrive at the decision about selection of the best flaps based on the characteristics of the defect and on the individual anatomy of the patient.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
This systematic review and meta-analysis provide a pragmatic evaluation of drain-free versus drain-based DIEP flap techniques for breast reconstruction, challenging the traditional reliance on drainage. By analyzing postoperative outcomes, the study highlights the potential for refining surgical strategies to enhance patient comfort and recovery without compromising safety. The findings offer a neutral perspective, suggesting that clinical practice may not necessarily depend on the use of drains. This revelation prompts medical professionals to reassess existing surgical approaches and may catalyze a paradigm shift in postoperative care. Presented with clear narrative and rigorous data analysis, the article encourages readers to consider the broader implications of surgical innovations on patient care protocols.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
The retrospective study includes 115 patients who underwent reconstruction using a keystone design perforator island flap. In the study, skin malignancies were found to be the most common cause of soft tissue defects. The majority of defects were found on the trunk, followed by the lower extremities. Most patients used the type II keystone design perforator island flap. A total of 13.04% of patients had complications after surgery, with the majority being treated conservatively. A 6-month follow-up showed that none of the patients reported impaired flap sensitivity. According to the authors, the perforator island flap is a relatively simple and quick procedure for both inexperienced and experienced surgeons and enables reconstruction in a single surgical procedure. There is a significant amount of information in this study that may be of interest to readers of this journal. In my opinion, this article is worth publishing after addressing a minor issue. According to the authors, the keystone flap allows for a lot of reconstructive work to be done in just a single surgical procedure. It is a relatively simple and quick surgical approach with a short learning curve for both the novice and the experienced surgeon. However, the study was not able to provide the necessary data to prove that the approach can be used by surgeons with a "short learning curve". In order to make the conclusion more accurate, it needs to be revised.
RevisionThe assertion regarding the keystone flap's ability to facilitate reconstruction in a single surgical procedure, along with its relatively short learning curve for both inexperienced and skilled surgeons, has been removed. Subsequently, the conclusion of the manuscript has undergone comprehensive revisions and updates as outlined below: The KDPIF offers remarkable adaptability, practical and cosmetic benefits, and a low complication rate. It serves as an efficient reconstructive technique, allowing for single-stage surgery and demonstrating simplicity and expediency. The expanding indications for its use further highlight its clinical significance. The satisfactory aesthetic results observed during follow-up support its favorable outcomes. Notably, the KDPIF does not necessitate microsurgery or additional equipment, which is advantageous in terms of cost-effectiveness, particularly for healthcare systems in emerging countries. Overall, the KDPIF represents a suitable reconstructive solution with wide applicability and potential economic benefits.
Georgieva G, Tusheva S, Nikolovska B, Srbov B, Dzonov B, Pejkova S. Clinical applications of keystone design perforator island flap: A single-center experience. Int Microsurg J 2023;7(1):1. https://doi.org/10.24983/scitemed.imj.2023.00173