The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. In this case study, the excision of a cancer lesion on the face of 70-year-old female patient had resulted in a soft tissue defect of size 8 x 9 cm. The reconstruction of the surgical defect was done by using the supraclavicular perforator flap. The flap perforators were marked preoperatively with a handheld Doppler using indocyanine green angiography. During the flap dissection, the dominant perforator was determined by a selective clamping of each of the perforators guided by the indocyanine green angiography. Though the distal perforator was determined to be the dominant one, the pedicled flap design was found to be of inadequate length to reach the surgical defect. Consequently, the flap was turned into a free flap. The pedicle was anastomosed to the branches of facial vessels and survived completely. In conclusion, we believe that the dominant perforator may be identified by intraoperative indocyanine green angiography which would help in making a proper decision for flap design.
In 1903, Toldt, an anatomist, first illustrated and named the arteria cervicalis superficialis. The artery originates from the thyrocervical trunk, exiting between the trapezius and sternocleidomastoid muscles [1,4]. Kazanjian and Converse are credited with the first clinical application of this flap in 1949 [5-7]. The use of this flap had gone out of favor until the early 1990s. It was then that Norbert Pallua rediscovered the supraclavicular flap and popularized its use. Pallua et al. had used this flap for post burn neck contracture, as well as head and neck malignancies [8-12].
The supraclavicular flap is usually raised as a pedicled island or as a transposition flap. The donor site may either be closed directly or with a split skin graft, depending on the size of the flap, laxity of the skin of the supraclavicular and shoulder region, and the pre-expansion condition of the flap. The use of supraclavicular flap as a free flap was reported by Pallua, who used this flap as a free flap for hand and foot reconstruction in two patients [12]. It was also reported as a free flap for head reconstruction by Cordova et al. and Alves et al. [13,14].
The pedicle of this flap emerges from transverse cervical artery and is located in the triangle formed by the dorsal edge of the sternocleidomastoid muscle, the external jugular vein, and the medial part of the clavicle [5,15,16]. Anatomical variations have been described in the pathway of the dominant pedicle to the flap, which courses under the clavicle and turns upwards towards the skin. Due to the variations in the course of the pedicle, the length of the pedicled flap is variable.
The aim of this case report is to show (1) that the determination of the dominant pedicle may be aided with the use of indocyanine green angiography and (2) that the supraclavicular flap can be converted to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
We describe the case of a 70-year-old female patient who had to undergo wide excision of a tumor with squamous cell carcinoma on the left cheek by an otolaryngologist. The reconstruction of the facial defect with a free supraclavicular flap was performed by a plastic surgery team in Sant Pau I Santa Creu hospital in Barcelona, Spain in January 2018.
The wide resection of the tumor resulted in a large soft tissue defect of the size of 8 x 9 cm. A left supraclavicular perforator flap was planned. The flap pedicle was identified by a handheld Doppler as a single perforator in the triangle outlined between sternocleidomastoid, clavicle and trapezius. The flap borders were marked having a length of 20 cm from the pedicle and width of 9 cm at the distal part to match the size of the defect (Figure 1).
An intraoperative indocyanine green angiography was performed before dissection, and more perforators were identified and marked (Figure 2). Dissection started from distal to proximal part of the flap in the subfascial plane.
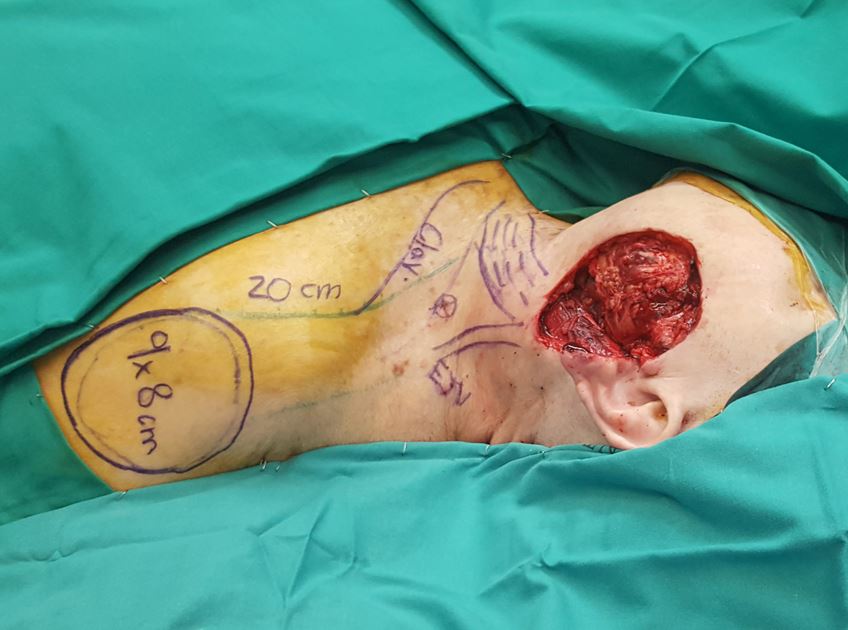
Figure 1. Wide resection of the tumor resulted in a large soft tissue defect of the size of 8 x 9 cm. A left supraclavicular perforator flap was planned. The flap borders were marked having a length of 20 cm from the pedicle and width of 9 cm at the distal part to match the size of the defect.

Figure 2. An intraoperative indocyanine green angiography was performed before dissection, and more perforators were identified and marked.
The flap was raised on two pedicles consistent with the results showed by the indocyanine green angiography, one from supraclavicular vessels and the second from subclavicular region (Figure 3A). Using indocyanine green imaging, both pedicles were sequentially clamped and then released to check the vascularity and perfusion status of the flap. The supraclavicular vessel entered the flap at its proximal third. The infraclavicular pedicle had a bigger caliber and better pulsation than the supraclavicular pedicle but entered the flap in its middle third (Figure 3B-C).
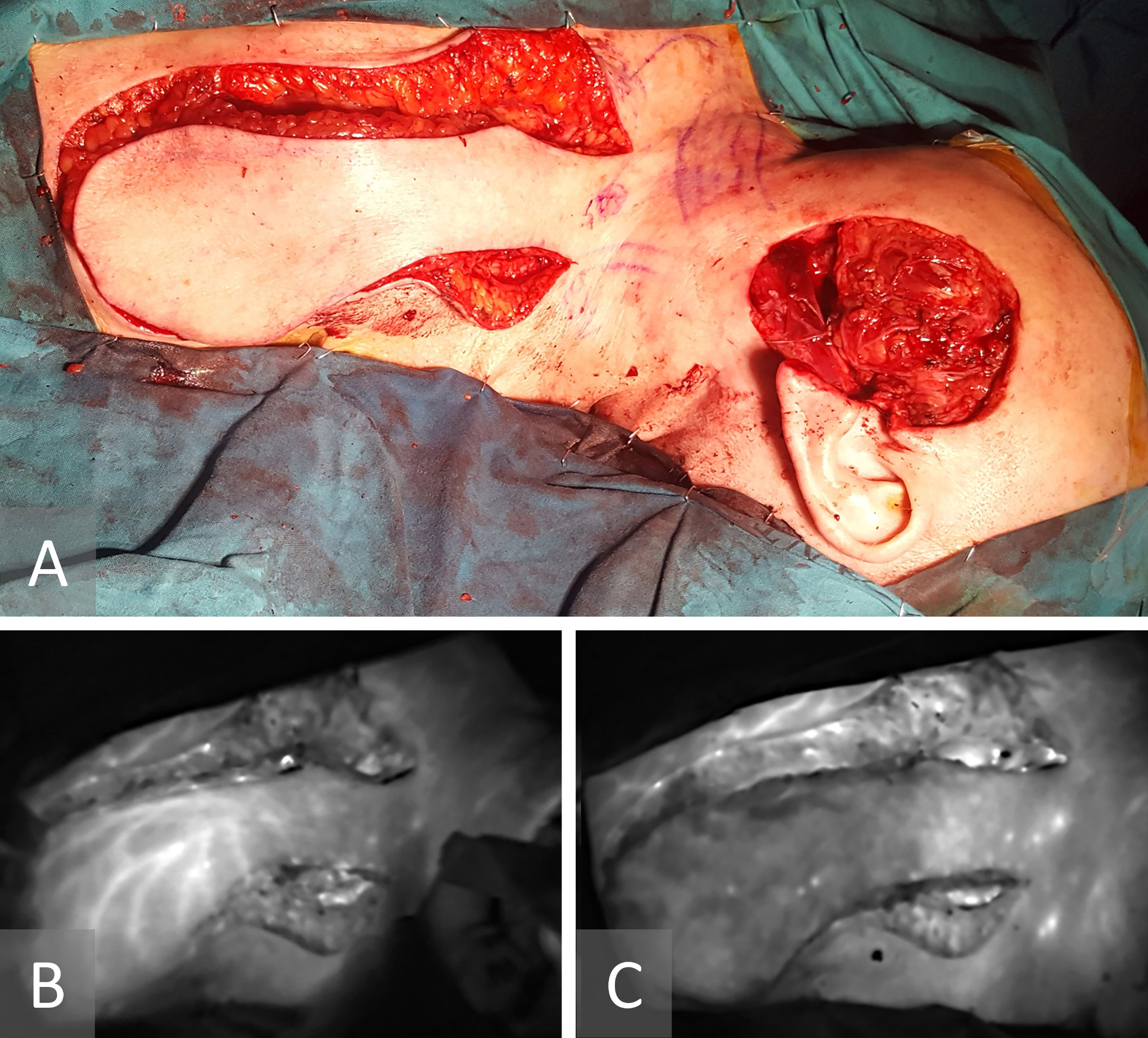
Figure 3. (A) The flap was raised on two pedicles consistent with the results showed by the indocyanine green angiography, one from supraclavicular vessels and the second from subclavicular region. (B, C) Using indocyanine green angiography, both pedicles were sequentially clamped and then released to check the vascularity and perfusion status of the flap. The supraclavicular vessel entered the flap at its proximal third. The infraclavicular pedicle had a bigger caliber and better pulsation than the supraclavicular pedicle but entered the flap in its middle third.
Clinical examination and indocyanine green angiography showed that the subclavicular pedicle was dominant. The arc of rotation of the flap was limited, as was the reach of the pedicled flap. We therefore opted to convert it into a free flap. The proximal quarter of the flap was too narrow and not sufficiently perfused; hence it was discarded (Figure 4A). A branch of the ipsilateral facial artery and the facial vein were prepared as recipient vessels. The flap size was adjusted to match the size of the facial defect (8 x 9 cm). It was then inset on the defect, and the infraclavicular pedicle was anastomosed end-to-end to the facial vessels (Figure 4B). The donor site was closed at the proximal part and skin grafted at the distal part. The flap survived completely, and the wounds healed up uneventfully five weeks after surgery (Figure 4C).
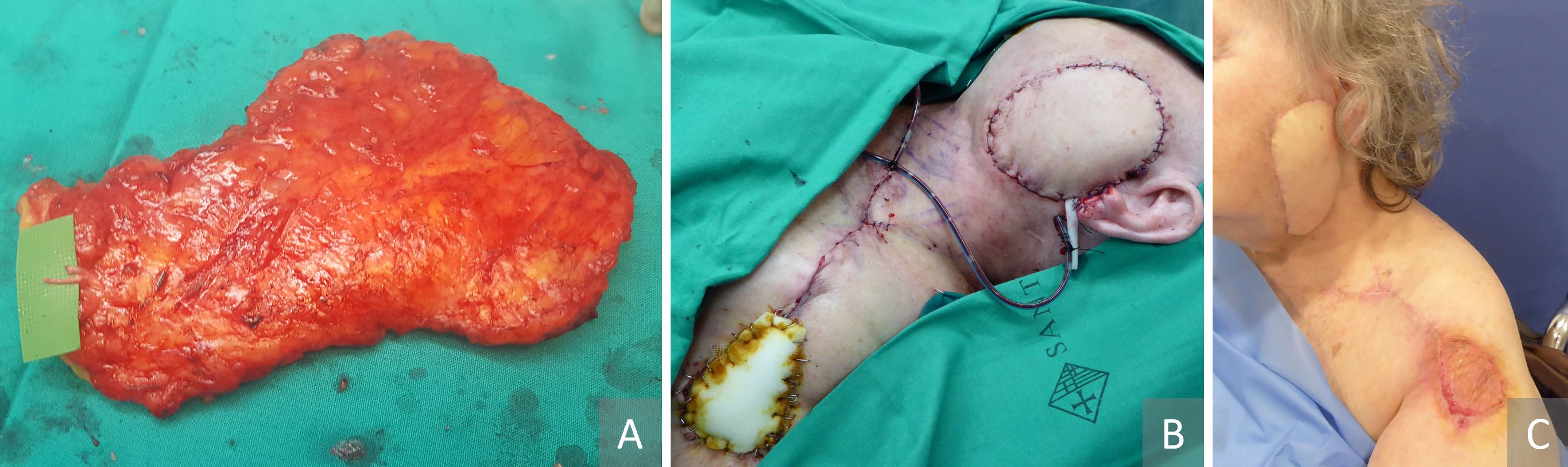
Figure 4. (A) The subclavicular pedicle was dominant and the arc of rotation of the flap was limited. We therefore opted to convert it into a free flap. The proximal quarter of the flap was quite narrow and not sufficiently perfused; hence it was discarded. (B) A branch of the ipsilateral facial artery and the facial vein were prepared as recipient vessels. The flap size was adjusted to match the size of the facial defect (8 x 9 cm). It was then inset on the defect, and the infraclavicular pedicle was anastomosed end-to-end to the facial vessels. (C) The donor site was closed at the proximal part and skin grafted at the distal part. The flap survived completely, and the wounds healed up uneventfully five weeks after surgery.
Radiological mapping of the pedicle and angiosomes of supraclavicular artery flap is useful but complex. Sheriff et al. [3] have compared six imaging modalities for identifying the pedicle and marking the perfusion zones of supraclavicular artery flap. Of these, intraoperative indocyanine green angiography was the most practical and accurate in identifying the vascular anatomy of the superficial vessels in real time, making the mapping of the pedicle and angiosomes reliable [3,17].
However, the ability of indocyanine green angiography in showing the full course of the pedicles and perforators is limited and depends on the amount of adipose tissue subjacent to the skin and the site of emergence of the vessels. As the depth of visualization of blood vessels by indocyanine green angiography is limited to approximately 2 cm [17], it could show the perforators sites precisely. However, it could not show the pathway of the pedicle deep in the tissue. It also did not show the course of the pedicle above or below the clavicle, and hence there was no change in the initial plan of supraclavicular flap to another type of flap.
In this case, the indocyanine green angiography was able to guide the conversion of the pedicled supraclavicular artery flap to a free supraclavicular flap for reconstruction of the facial defect caused by an unusual course of the dominant pedicle of the flap. The vast majority of articles on the supraclavicular flap in peer-reviewed literature discuss the pedicled design of the flap but there is little discussion about the use of the free flap design.
Intraoperative indocyanine green angiography before and during dissection may be useful in identification of the dominant perforator and pedicle pathways. It helps make a right decision in the ultimate flap design in order to avoid complications which might arise due to anatomic variations.
Received date: March 20, 2020
Accepted date: June 13, 2020
Published date: September 02, 2021
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors report no financial or other conflict of interest relevant to this article, which is the intellectual property of the authors.
© 2021 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
The communication among international microsurgeons have switched from one direction (from paper, textbook) to multiway interactions through the internet. The authors believe the online platform will play an immensely important role in the learning and development in the field of microsurgery.
Traditionally, suturing techniques have been the mainstay for microvascular anastomoses, but owing to its technical difficulty and labour intensity, considerable work has gone into the development of sutureless microvascular anastomoses. In this review, the authors take a brief look at the developments of this technology through the years, with a focus on the more recent developments of laser-assisted vascular anastomoses, the unilink system, vascular closure staples, tissue adhesives, and magnets. Their working principles, with what has been found concerning their advantages and disadvantages are discussed.
Prof. Koushima, president of World Society for Reconstructive Microsurgery, proposes an innovative concept and technique of the multi-stage ‘Orochi’ combined flaps (sequential flaps in parallel). The technique opens a new vista in reconstructive microsurgery.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
Authors discuss a silicone tube that provides structural support to vessels throughout the entire precarious suturing process. This modification of the conventional microvascular anastomosis technique may facilitate initial skill acquisition using the rat model.
PEDs can be used as alternative means of magnification in microsurgery training considering that they are superior to surgical loupes in magnification, FOV and WD ranges, allowing greater operational versatility in microsurgical maneuvers, its behavior being closer to that of surgical microscopes in some optical characteristics. These devices have a lower cost than microscopes and some brands of surgical loupes, greater accessibility in the market and innovation plasticity through technological and physical applications and accessories with respect to classical magnification devices. Although PEDs own advanced technological features such as high-quality cameras and electronic loupes applications to improve the visualizations, it is important to continue the development of better technological applications and accessories for microsurgical practice, and additionally, it is important to produce evidence of its application at surgery room.
Avulsion injuries and replantation of the upper arm are particularly challenging in the field of traumatic microsurgery. At present, the functional recovery of the avulsion injuries upper arm after the replantation is generally not ideal enough, and there is no guideline for the surgeries. The aim of this study was to analyze the causes of failure of the upper arm replantation for avulsion injuries, summarize the upper arm replantation’s indications, and improve the replantation methods.
The implications of rebound heparin hypercoagulability following cessation of therapy in microsurgery is unreported. In this article the authors report two cases of late digit circulatory compromise shortly after withdrawal of heparin therapy. The authors also propose potential consideration for changes in perioperative anticoagulation practice to reduce this risk.
In a cost-effective and portable way, a novel method was developed to assist trainees in spinal surgery to gain and develop microsurgery skills, which will increase self-confidence. Residents at a spine surgery center were assessed before and after training on the effectiveness of a simulation training model. The participants who used the training model completed the exercise in less than 22 minutes, but none could do it in less than 30 minutes previously. The research team created a comprehensive model to train junior surgeons advanced spine microsurgery skills. The article contains valuable information for readers.
The loupe plays a critical role in the microsurgeon's arsenal, helping to provide intricate details. In the absence of adequate subcutaneous fat, the prismatic lens of the spectacle model may exert enormous pressure on the delicate skin of the nasal bone. By developing a soft nasal support, the author has incorporated the principle of offloading into an elegant, simple yet brilliant innovation. A simple procedure such as this could prove invaluable for microsurgeons who suffer from nasal discoloration or pain as a result of prolonged use of prismatic loupes. With this technique, 42% of the pressure applied to the nose is reduced.
An examination of plastic surgery residents' experiences with microsurgery in Latin American countries was conducted in a cross-sectional study with 129 microsurgeons. The project also identifies ways to increase the number of trained microsurgeons in the region. The authors claim that there are few resident plastic surgeons in Latin America who are capable of attaining the level of experience necessary to function as independent microsurgeons. It is believed that international microsurgical fellowships would be an effective strategy for improving the situation.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This comprehensive review article presents a profound exploration of critical facets within the realm of microsurgery, challenging existing paradigms. Through meticulous examination, the authors illuminate the intricate world of microangiosomes, dissection planes, and the clinical relevance of anatomical structures. Central to this discourse is an exhaustive comparative analysis of dermal plexus flaps, meticulously dissecting the viability and potential grafting applications of subdermal versus deep-dermal plexi. Augmenting this intellectual voyage are detailed illustrations, guiding readers through the intricate microanatomy underlying skin and adjacent tissues. This synthesis of knowledge not only redefines existing microsurgical principles but also opens new frontiers. By unearthing novel perspectives on microangiosomes and dissection planes and by offering a comparative insight into dermal plexus flaps, this work reshapes the landscape of microsurgery. These elucidations, coupled with visual aids, equip practitioners with invaluable insights for practical integration, promising to propel the field of microsurgery to unprecedented heights.
This article presents a groundbreaking surgical approach for treating facial paralysis, focusing on the combination of the pronator quadratus muscle (PQM) and the radial forearm flap (RFF). It addresses the challenges in restoring facial functions and skin closure in paralysis cases. The study's novelty lies in its detailed examination of the PQM's vascular anatomy when combined with the RFF, a topic previously unexplored. Through meticulous dissections, it provides crucial anatomical insights essential for enhancing facial reanimation surgeries, offering significant benefits in medical practices related to facial reconstruction and nerve transfer techniques.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
Sheriff H, Vega Garcia C, Garcia Lorenzo J, Lopez Fernandez S, Shahab Kareem S, Hankins C, Masia J, Fernandez Garrido M. Indocyanine green angiography in salvage planning: From pedicled supraclavicular flap to free supraclavicular flap. Int Microsurg J 2021;5(1):4. https://doi.org/10.24983/scitemed.imj.2021.00145