Objectives: A reverse flow island (or free) first web space flap with a long vascular pedicle involving the first metatarsal artery (1st MTA) is frequently used for the coverage of toes and finger defects. The major disadvantages of this flap are postoperative donor site pain and numbness due to damage to the deep peroneal nerve, or depressive scarring on the first web space following soft tissue loss.
Methods: Instead of the dominant perforators of perforator flaps, capillary perforators are recently becoming a new pedicle vessel of perforator flaps. Therefore, to overcome these disadvantages of the first web space flap, the first metatarsal artery capillary perforator (1st MTAcp) flap with a capillary perforator was used as island and free flaps. Since 1994, eight patients with foot and hand defects were treated with five island and three free 1st MTAcp flaps.
Results: There were no flap necrosis and no problems due to nerve compression in the donor site. It was found that a free 1st MTAcp flap, including a short “T” segment of the 1st MTA, was useful as a flow-through flap for finger pulp defects.
Conclusion: An island or free 1st MTAcp flap is possible without including the 1st MTA. The advantages of this flap include the preservation of the first metatarsal artery (in case of an island flap) and the adiposal tissue in the web space, which prevent compression around the remaining deep peroneal nerve. This results in no postoperative donor site pain or numbness due to damage to the deep peroneal nerve. There is no possibility of a depressive scar on the first web space because the soft tissue can be preserved in the donor site. The major disadvantage of this flap is that since the perforators are so small (sometimes invisible), loops or operative microscope are required for their dissection. This flap is indicated for the great and second toes as an island flap, and for hand and fingers as a free flap.
A free first web space flap with a long vascular pedicle involving the first metatarsal artery (1st MTA) is used for the coverage of toe and finger defects as a reverse-flow island or free flap [1-3]. The major disadvantages of this flap are postoperative donor site pain, numbness due to damage to the deep peroneal nerve, and a depressive scar on the first web space following soft tissue loss. Meanwhile, instead of the dominant perforators of perforator flaps, capillary perforators are recently becoming more widely used as a common new pedicle vessel of perforator flaps [4,5]. As the 1st MTA had several capillary perforators, a new less invasive island flap, the first metatarsal artery capillary perforator (1st MTAcp) flap, was installed without sacrificing the 1st MTA or the soft tissue in the first web space. In addition, it was found that a free 1st MTAcp flap, including a short “T” segment of the 1st MTA, was useful as a flow-through flap for palm defects of the hand. In this series, we report an island capillary perforator flap without transection of the 1st MTA and a free flap with a short segmental 1st MTA.
Anatomy of the First Metatarsal Artery
The 1st MTA comes from the dorsalis pedis artery and connects to the proper digital arteries of the great and second toes with the communicating branch. This communicating branch is usually large and connects directly to the digital arteries. However, sometimes it is hypoplastic or missing (and the 1st MTA distributes so as to terminate in the subcutaneous tissue of the first web space). The dominant communicating branch can be used as an island reverse flow 1st MTA flap, including the 1st MTA. The 1st MTA usually has several capillary perforators. Anatomically, two types of capillary perforators exist: one is the superfascial adiposal perforator, which arises from the 1st MTA which runs suprafascially. The other is the intermuscular type perforator, which arises from the intramuscular 1st MTA, penetrating the interosseous muscle. The dorsal cutaneous veins, subdermal cutaneous veins, and several distal branches compose the superficial axial venous system through the 1st MTA of the first web space. The deep peroneal nerve runs through the dorsalis pedis vessels and terminates in several branches on the first web space and the dorsal aspect of the great and second toes (Figure 1A).
Surgical Techniques
Using an air tourniquet (a tourniquet is very important to detect small perforators), a longitudinal incision was made on the first web space. Superficial subdermal and deep cutaneous veins were preserved as a drainage system of this flap. Several perforators penetrating through the interosseous muscle from the 1st MTA and concomitant vein are usually detected under loops or operative microscopy. Including the main capillary perforator of the 1st MTA, the flap was designed on the 1st web space, sometimes extending into the proximal dorsum of the foot.
After a skin incision through the flap margin, the island flap is elevated from the proximal side of the dorsal foot. The perforators nearest to the defect, which are deeply dissected from the surrounding adiposal tissue, are confirmed to be connected to the cutaneous venous system. In cases in which the defects are in the great or second toe, the deep dissection or transection of the 1st MTA is usually unnecessary because an island flap with a short pedicle can be rotated 180 degrees around the perforator to reach the defect. The branches of the deep peroneal nerve can also be preserved without any damage. Based on our cases, a single capillary perforator is enough to supply a flap, and a larger flap over 3 cm in width usually needs a skin graft to close the donor defect. In cases with hand pulp or palm defect, a short segment of the first metatarsal artery involving a perforator is interposed into the transected digital artery in a flow-through manner. The dorsal cutaneous vein and a branch of the deep peroneal nerve are also included as another pedicle (Figure 1B).
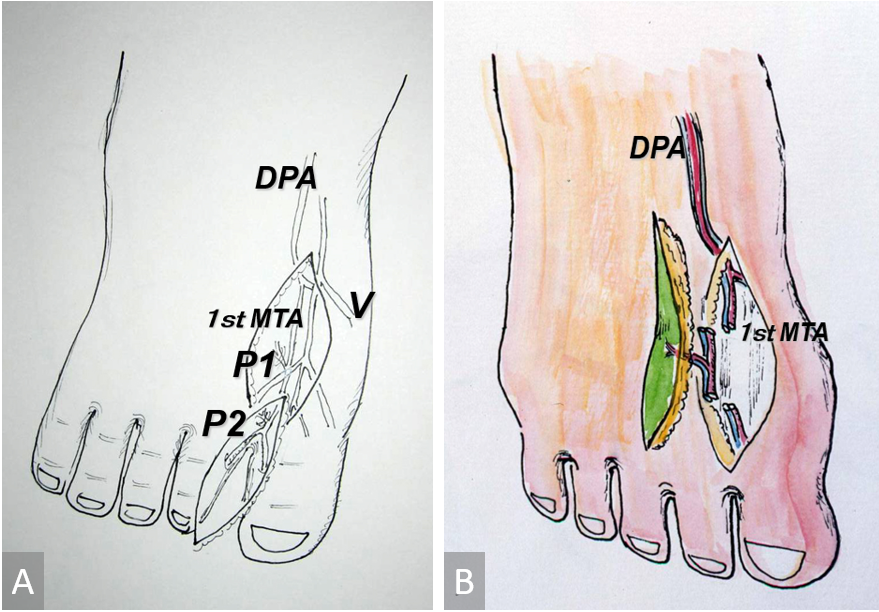
Figure 1. (A) Schematic drawing of the 1st MTAcp flap. Small capillary perforators (P1 & P2) arise from the first metatarsal artery at the first web space. (B) Free 1st MTAcp flap with a short segmental vessel. 1st MTAcp, first metatarsal artery capillary perforator; DPA, dorsalis pedis artery; V, cutaneous vein.
Between June 1994 and December 2005, eight patients with extremity defects were treated with five island 1st MTAcp flaps and three free 1st MTA flaps. The number of defects was three in the fingers and hand, and five in the foot and toes. The operated patients were four males and four females with the age range of 12 to 75 years. The flaps ranged from 3 to 8 cm in length and 1 to 5 cm in width. As for postoperative complications, there were no serious complications and not any flap necrosis (Table 1).
Case 1: Island Flap for Second Toe Defect (No. 4 in Table 1)
A 26-year-old man sustained a skin necrosis on the volar side of the right second toe. This was caused by an avulsion injury and an X-ray revealed dislocation of the distal interphalangeal joint. After the resection of the necrotic tissue and repositioning of the distal phalangeal bone, an island 1st MTAcp flap of 8 x 2 cm was transferred to cover the defect. The donor defect was closed with a split-thickness skin graft from the right thigh. Postoperatively, the flap and skin graft survived completely, and the patient walked without problems (Figure 2).
Case 2: Scar Related Contracture of the Little Finger (No. 8 in Table 1)
A 59-year-old man sustained a skin defect on the volar aspect of the left little finger. This was combined with a complicated fracture of the fifth metacarpal phalanx by an encounter with a rice harvesting machine. Although an island ulnar artery perforator flap was used to repair the defect, a severe volar scar contracture of the little and ring fingers remained. After releasing the contracture, a free 1st MTAcp flap of 8 x 5 cm, with a short segmental pedicle, was transferred. A short segment of the 1st MTA and the dorsal cutaneous vein of the flap were anastomosed to the ulnar digital artery of the ring finger and the dorsal cutaneous vein of the hand. Postoperatively, the flap survived completely. The contracture of the little finger was released and there was not any donor site morbidity (Figure 3).
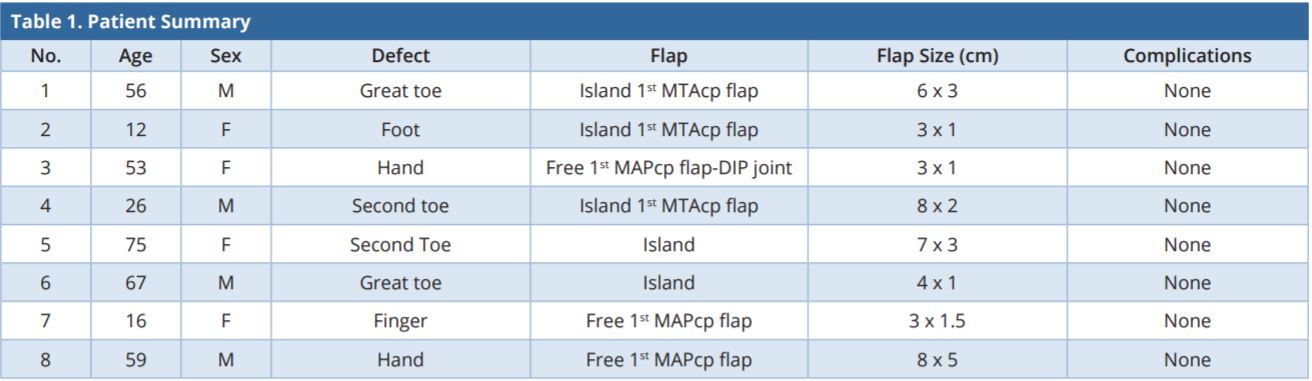
1st MTAcp, first metatarsal artery capillary perforator; DIP, distal interphalangeal joints; F, female; M, male.
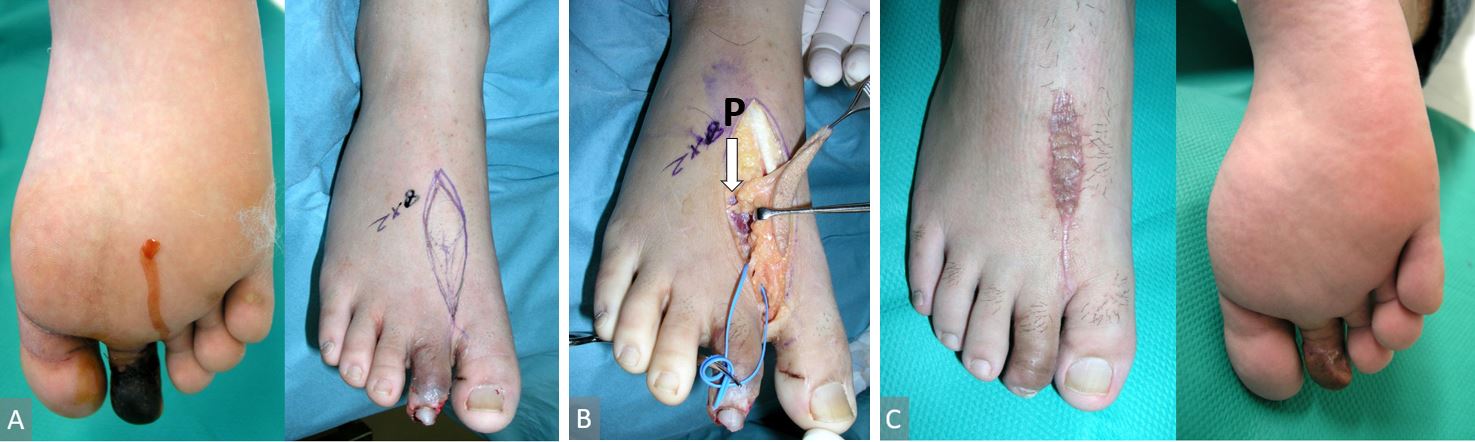
Figure 2. (A) Left, a 26-year-old man with volar skin necrosis of the right second toe. Right, an island 1st MTAcp flap was designed. (B) The flap was transferred with the distal capillary perforator. P indicates transected proximal perforator. (C) Left, two months after surgery. The donor defect was closed with a split thickness skin graft. Right, the flap survived completely.
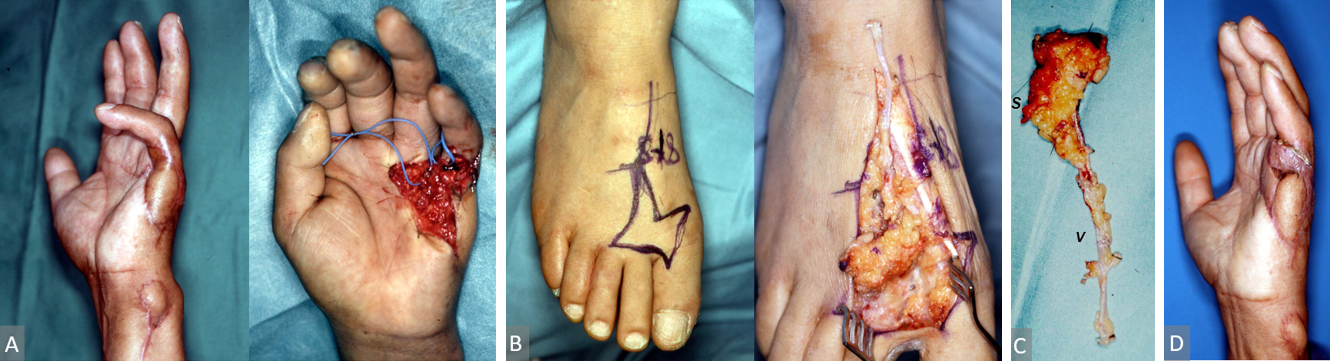
Figure 3. (A) Case 3, a 59-year-old man with a severe volar scar contracture of the left little finger. Right, the contracture was released. (B) A free flap with a short segment of 1st MTA was elevated on the right foot dorsum. Left, flap design. Right, the deep peroneal nerve was preserved. (C) A short segment (marked as S) of the 1st MTA and dorsal cutaneous vein (marked as V) of the flap were included in the flap and anastomosed to the ulnar digital artery of the ring finger and dorsal cutaneous vein of the hand. (D) Three months after surgery. The flap survived completely. 1st MTA, first metatarsal artery.
In this series, we report an island capillary perforator flap without transection of the 1st MTA and a free flap with a short segmental 1st MTA. These flaps are completely different from the first web space flap, including the pedicle of the 1st MTA. In 1989, Earley reported the first web flap with such capillary perforators and described the distal web-space cutaneous vessels, which arose from the 1st dorsal MTA and common digital vessels [2]. The number of vessels with a diameter sometimes smaller than 0.3 mm varied between two and five arterial branches. However, the flap was not an island flap, but a rectangular flap based on wide skin pedicle including many pedicle vessels and nerves.
In this series, it was proved that only single perforators can feed the flap (maximum dimension 8 x 5 cm) with complete island elevation by transection of whole skin margin. Therefore, being differentiated from the conventional 1st web flap or 1st MTA flap reported by Earley, our flap was named as “1st MTA capillary perforator flap“.
The new concept of “capillary perforator flap” has been already proposed many times in the meetings of the International Perforator Course, World Society of Reconstructive Microsurgery, American Society of Reconstructive Microsurgery, and also described as “thoracodorsal artery capillary perforator (TAPcp) flap [5].” We defined “capillary perforator” as less than 0.3 mm perforator (sometimes invisible perforator with bare eyes) and nourished skin flaps of some dimension (at least 7 x 5 cm). This concept is very important because recently, and in future, we believe that many new flaps nourished with much smaller perforators less than 0.3 mm are (and will be) proposed in some proper areas (around joints and through peripheral nerves) in the human body.
The advantages of this flap are that the 1st MTA (in case of an island flap) and the deep peroneal nerve with the surrounding adiposal tissue can be preserved in the web space. There is no postoperative donor site pain or numbness. There is no possibility of a depressive scar on the first web space because the soft tissue can be preserved in the donor site. The disadvantages are that since the perforators are so small (sometimes invisible), loops are required for their dissection, and a large flap cannot be obtained without skin grafting onto the donor defect because of the tightness of the skin.
This flap is indicated for the coverage of the defects around the first web space, including the great and second toes as an island flap. As a free flap, with a short segment of the 1st MTA and its perforator (flow-through flap), the defects of the hand and fingers can be repaired less invasively. In addition, free composite flaps including tendons, nerves, and/or joints can be used for composite hand defects. A simple vascularized deep peroneal nerve flap with the same pedicle is also useful for nerve defects in scarred beds.
In terms of future applications of this flap, based on our experience, a vascularized lymphadiposal flap is useful for severe lymphedema of the contralateral leg because some lymphatics with drainage function exist in the first web space of the leg [6]. There is no possibility of postoperative edema of the donor leg because of no damage of lymphatic system at the proximal leg, and each channel has rich vascular supply because of these perforators.
The 1st MTAcp flap is a new capillary perforator flap and less invasive reconstructions with this flap are now possible for the defects around the first web space, toes, and fingers. In addition, the concept of the use of this capillary perforator flap will help open a new field in reconstructive surgery in the future.
Received date: October 07, 2018
Accepted date: November 26, 2018
Published date: January 04, 2019
None
None
The authors would like to thank Dr. Motoyuki Doi, Orthopedic Surgery in Kyokuto Hospital in Okayama City, and Dr. Masayuki Ohmori, Ohmori Clinic in Okayama City, for their supports of this work.
This work was presented in part at the Third International Course on Perforator Flap in Munich, on November 13, 1999, the 48th Japanese Society of plastic and Reconstructive Surgery in Tokyo, on April 13, 2005, and the 9th International Course on Perforator Flaps in Barcelona, on October 7, 2005.
Informed consents were obtained from the patients.
© 2019 The Author (s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
Osteoarthritic finger joints are often repaired with joint implants, arthrodesis, or a vascularized interphalangeal joint graft. However, grafts can damage the donor toe. Based on the results of this study, the authors suggest that vascularized distal interphalangeal joint transfers from the second toe may be suitable for reconstructing these defects through microsurgery.
Division of the lateral plantar artery does not jeopardize the foot circulation because of anastomosis of the lateral plantar artery with the dorsalis pedis artery at the first intermetatarsal space. However, care should be taken with patients with peripheral artery occlusive disease and the flow of dorsalis pedis artery should be confirmed before surgery. Given the advantages of sizable vessel, easy dissection, and proximity to the defect, we believe that the lateral plantar artery might be a valuable option as recipient vessel for lateral plantar forefoot reconstruction.
The authors reviewed the MDCT images to show the number of lymph nodes superior to the saphenofemoral junction. In this study, on average, 3.67 nodes existed. However, there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
The ALT and AMT flaps are the most commonly used thigh free flaps for intraoral reconstruction. Recently, PAP flap has been proposed as an alternative. This study aimed to compare the thickness of these thigh flaps and to identify the factors influencing flap thickness in our population.
A thin profunda artery perforator flap harvested from the left thigh is shown in this video. Preoperative computed tomographic angiography is used to assess morphology of the perforators and its branches, pedicle length and vertical location of the two branches from the ischial tuberosity. These measurements are translated on to the patient. Locations of both branches are confirmed with a handheld doppler. The authors concluded that preoperative computed tomographic angiography is a useful technique to provide detailed anatomic information on morphology of perforators, course through the septum or muscle above the deep fascia and skin thickness. Computed tomographic angiography allows quick and easy assessment of the whole vascular anatomy of the leg and helps to arrive at the decision about selection of the best flaps based on the characteristics of the defect and on the individual anatomy of the patient.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
This systematic review and meta-analysis provide a pragmatic evaluation of drain-free versus drain-based DIEP flap techniques for breast reconstruction, challenging the traditional reliance on drainage. By analyzing postoperative outcomes, the study highlights the potential for refining surgical strategies to enhance patient comfort and recovery without compromising safety. The findings offer a neutral perspective, suggesting that clinical practice may not necessarily depend on the use of drains. This revelation prompts medical professionals to reassess existing surgical approaches and may catalyze a paradigm shift in postoperative care. Presented with clear narrative and rigorous data analysis, the article encourages readers to consider the broader implications of surgical innovations on patient care protocols.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
Combining intraoperative ICG lymphography with NIR vein visualization can aid supermicrosurgeons in identifying lymphatic vessels and superficial venules to guide LVA incision placement. This guided approach significantly improves successful creation of LVAs when compared to the blind (anatomic) approach. In addition, the absence of linear ICG lymphographic patterns does not prevent formation of successful LVAs.
Immediate limb compression following the LVA procedure facilitates lymphatic drainage and increases the surgical efficacy by increasing the number of functioning anastomoses, and is a recommended postoperative practice.
This case report demonstrates an important supermicrosurgical technique for lymphedema, which was established by Isao Koshima in 1994. So far, over 2,000 cases of limb edema have been treated by this surgical method.
LVA and vascularized lymph node transfer VLNT are established lymphedema treatments. However, LVA is only effective for early disease and VLNT can cause donor-site lymphedema and contour deformity. VLVT is free of these limitations. The authors described their experience of a new VLVT technique.
Osteoarthritic finger joints are often repaired with joint implants, arthrodesis, or a vascularized interphalangeal joint graft. However, grafts can damage the donor toe. Based on the results of this study, the authors suggest that vascularized distal interphalangeal joint transfers from the second toe may be suitable for reconstructing these defects through microsurgery.
This is an interesting article that addresses a technique entitled “first metatarsal artery capillary perforator (1st MTAcp) flap” with a capillary perforator used as island and free flaps. In total eight patients with foot and hand defects were treated with five island and three free 1st MTAcp flaps in the past 20+ years. There were no major complications such as flap necrosis and no problems due to nerve compression in the donor site. This is a surgical technique with innovation and favorable outcomes. I recommended this article to be published, however, the article needs to be proofread by an English native speaker before publication.
I believe this article is of good innovation and can be considered as an original work rather than a case series. I suggest that there should be Methods and Results sections. For instance, the Method section includes “Anatomy of the First Metatarsal Artery” and “Surgical Techniques”. The Results section includes “Patient Summary” and “Case Report”.
This article is interesting, very innovative, and worthy of publication.
This is a well-written article and will add contribution to the literature. I highly recommend its publication.
Koshima I, Imai H, Yoshida S, Narushima M, Yamashita S, Iida T. First metatarsal artery capillary perforator flaps. Int Microsurg J 2019;3(1):1. https://doi.org/10.24983/scitemed.imj.2019.00093