Objective: Fingertip amputations from motorcycle chain injuries involve severe crushing and contamination, traditionally necessitating revision amputation. We evaluated the feasibility of a modified primary replantation protocol tailored to this high-energy trauma.
Methods: We conducted a retrospective analysis of six patients who underwent fingertip replantation for motorcycle chain-related amputations classified as Tamai Zone I or II at a tertiary care center between 2021 and 2025. The surgical protocol emphasized aggressive debridement and strategic bone shortening to facilitate tension-free primary anastomosis, thereby minimizing the need for interpositional vein grafts. A simplified single-vessel supermicrosurgical anastomosis was performed with 11-0 nylon sutures. Additional technical priorities included volar vein identification and management of the extensive zones of injury characteristic of these mechanisms. The primary outcome was digit survival. Secondary outcomes included perioperative complications (venous congestion and infection), radiographic bone union, nail aesthetics, and functional recovery.
Results: Of 12 patients presenting with motorcycle chain amputations, six met the criteria for replantation and were included. Among these six completed replantations, survival was achieved in five (83%). One failure resulted from delayed venous congestion on postoperative day five. Despite the heavy contamination inherent to these injuries, no infection-related complications were observed. All surviving digits regained gross sensation sufficient for protection and demonstrated satisfactory functional and aesthetic recovery. All five surviving patients returned to pre-injury occupations within three months, as assessed by self-reported functionality. The simplified single artery and single vein configuration proved reliable even without complex multivessel repairs.
Conclusion: Primary replantation is feasible for motorcycle chain injuries with identifiable vessels. A protocol of radical debridement, skeletal shortening, and single-vessel anastomosis successfully preserved digits traditionally managed via revision amputation, suggesting that exclusion criteria for reconstructable targets merit re-evaluation.
Fingertip amputations resulting from motorcycle chain injuries constitute a distinct high-energy trauma pattern [1,2]. Disproportionately affecting young adults [1,3], these injuries are characterized by severe crushing, avulsion, and gross contamination [4,5]. In contrast to sharp amputations, the resulting multilevel intimal damage severely compromises microvascular integrity, often rendering standard replantation techniques ineffective [2,3]. Indeed, a recent epidemiological study by Jaiswal et al. reported that all attempted replantations for motorcycle chain injuries failed due to the extent of crush and contamination [3].
While the principles of digital replantation are well established [6,7], literature specifically addressing the unique constraints of motorcycle chain injuries remains sparse. Given this knowledge gap and the high failure rates associated with conventional management [3], there is a critical need for operative strategies that adapt conventional principles to the constraints of severe soft-tissue compromise. This article outlines a reproducible protocol tailored to these hostile conditions. We describe a systematic approach prioritizing aggressive soft tissue management, strategic bone shortening, and simplified single-vessel anastomosis, aiming to establish primary replantation as a viable alternative to revision amputation for contaminated crush injuries.
Study Design and Data Collection
We conducted a retrospective analysis of patients who underwent fingertip replantation after crush injuries caused by motorcycle chains at a tertiary care center. The study period extended from November 2021 through May 2025. We extracted data on patient demographics, specific injury characteristics, surgical techniques employed, and postoperative clinical outcomes. The focus on motorcycle chain-related trauma allowed for consistent comparison within a single high-energy crush mechanism.
Inclusion Criteria and Surgical Exploration
The study included patients with fingertip amputations classified as Tamai Zone I or Zone II that resulted specifically from motorcycle chain mechanisms (Figures 1–5). All amputation stumps were explored under an operating microscope, followed by meticulous debridement and lavage. All stumps were systematically inspected to identify suitable dorsal or volar arteries and veins. Replantation proceeded only after confirmation of healthy, viable vessels following adequate debridement.
Exclusion Criteria and Intraoperative Abandonment
We excluded patients who declined replantation. We also excluded those with amputation levels proximal to Tamai Zone II and those with injuries caused by mechanisms other than motorcycle chains. The analysis was restricted to patients who underwent completed replantation. Cases in which intraoperative exploration revealed non-reconstructable vascular damage (necessitating revision amputation) were excluded from this series to focus specifically on the outcomes of the described replantation protocol. The decision to abandon replantation was made if suitable recipient vessels were absent in the amputation stump or if arterial inflow could not be established despite appropriate microsurgical techniques. In these instances, the fingertip was reconstructed with techniques that did not involve microsurgery.
Surgical Technique
Anesthesia and antibiotic prophylaxis
Procedures were performed under supraclavicular brachial plexus block to induce sympathetic blockade and minimize intraoperative vasospasm. Patients received intravenous cefuroxime initiated preoperatively and continued through postoperative day three, followed by a one-week course of oral antibiotics. A uniform anesthetic and antibiotic protocol was maintained for all patients to minimize confounding variables.
Debridement and infection control
Prior to surgical exploration, the amputated stump was thoroughly irrigated with 4% chlorhexidine gluconate solution. Irrigation was then continued with 1–2 liters of normal saline. We performed meticulous debridement under operating microscope magnification and excised all residual grease and oil soaked tissues, including compromised skin, fat, tendon, bone, and vascular structures. Povidone-iodine was strictly avoided to prevent staining of neurovascular structures. This combination of aggressive irrigation and selective debridement was intended to minimize the bacterial burden while preserving viable tissue for replantation.
Distal vessel exploration
The nail plate of the amputated part was anchored to a plastic suture carrier with 4-0 polypropylene sutures to facilitate handling [8]. An assistant retracted the skin using microvascular toothed forceps. We then explored the vessels under an operating microscope. The digital artery was typically identified superficial to the periosteum and volar to the distal phalanx at the level of the lunula. The vessel was marked with a surgical pen or 10-0 nylon suture. In cases where multiple arterial branches were present, we ligated one branch to mobilize additional length for anastomosis. Adjacent adipose tissue was carefully debulked to provide adequate space for placement of vascular clamps. These steps allowed precise identification and preparation of the smallest possible arterial segment suitable for reliable anastomosis.
Volar vein identification
Because dorsal veins were often unavailable due to the avulsion component of motorcycle chain injuries, we prioritized identification of volar veins. We located these vessels by applying gentle pressure to the digital pulp. After we created a plane between the vein and the overlying skin with microscissors, we designed an oblique incision to facilitate skin closure without tension over the anastomosis [6]. When the identified volar vein was positioned away from the midline, we used a central longitudinal incision and selectively released skin tagging sutures to achieve a tension-free venous repair (Figure 1C). This venous strategy emphasized preservation of any suitable outflow channel to reduce the risk of postoperative congestion.
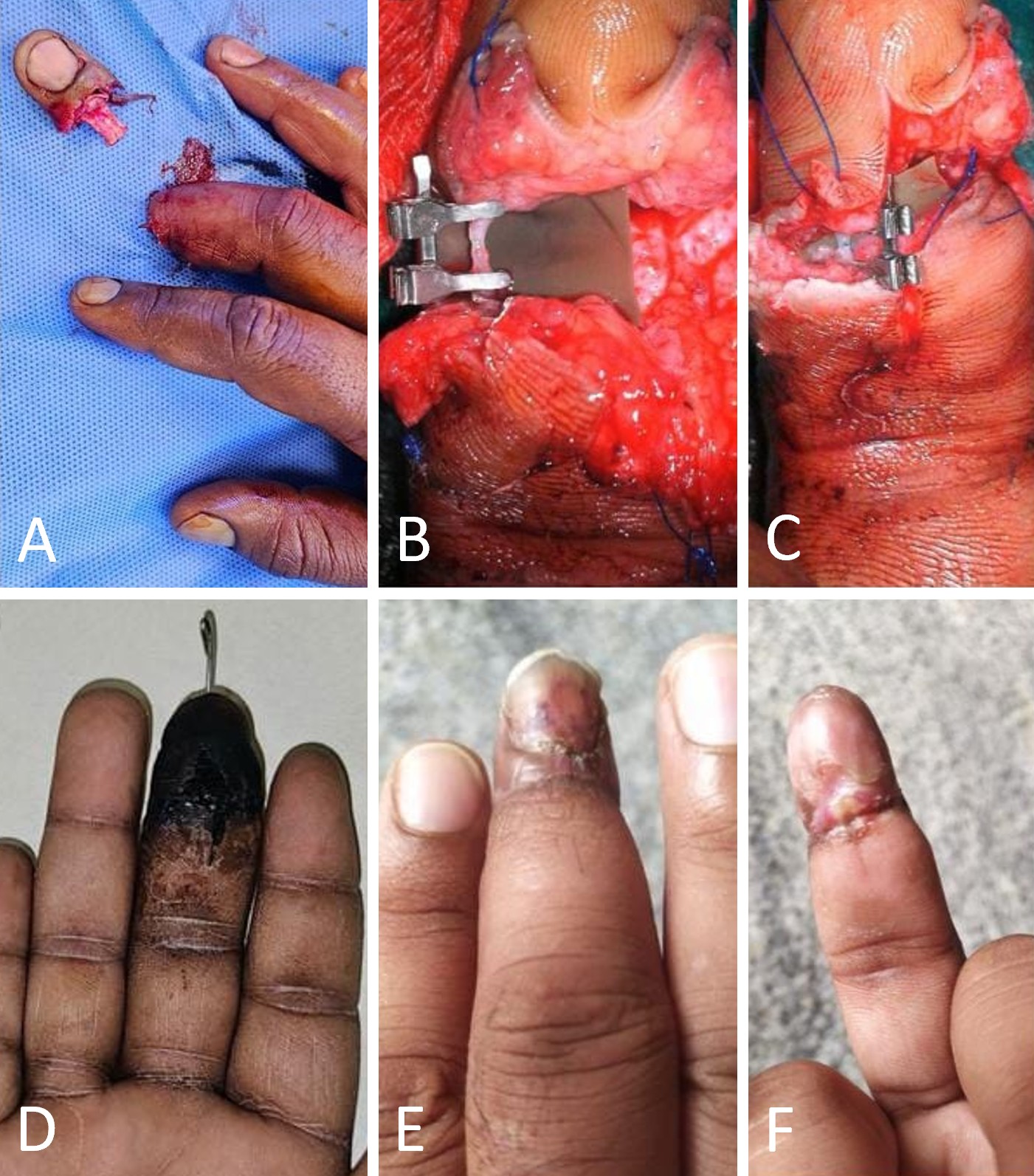
Figure 1. Replantation of a Tamai Zone II crush-avulsion injury of the right middle finger. (A) Preoperative clinical presentation showing a Tamai Zone II crush-avulsion amputation of the right middle finger. (B) Intraoperative view demonstrating the completed anastomosis of the ulnar digital artery. (C) Anastomosis of a volar digital vein; the ulnar skin-tagging suture has been released and the skin edge retracted to facilitate a tension-free venous repair. (D) Early postoperative appearance with diffuse epidermal discoloration but preserved tissue turgor, consistent with viable deep perfusion. (E, F) Late postoperative follow-up images in dorsal and volar views confirming complete survival of the replanted fingertip with satisfactory soft-tissue healing.
Proximal preparation and bone shortening
We explored the proximal stump in a similar manner. The skin edges were retracted and sutured proximally to optimize exposure. We selected the longest available digital artery and ligated proximal branches to gain additional length. Corresponding volar or dorsal veins were dissected. Before osteosynthesis, we approximated the bone ends to assess vessel reach and skin coverage. The proximal bone stump was shortened sufficiently to permit closure without tension. Strategic skeletal shortening was performed to facilitate tension-free repair, thereby obviating the need for interpositional vein grafts. Preference for primary anastomosis without interposition grafts was considered particularly important in this contaminated crush setting.
Osteosynthesis and nail bed repair
To reduce the risk of iatrogenic injury to the critical volar neurovascular bundle, we used an approach from dorsal to volar for fixation. We achieved rigid osteosynthesis using a single 1 mm axial Kirschner wire. This caliber provided adequate longitudinal stability while preserving the delicate architecture of the distal phalanx. This construct created a stable platform for soft tissue reconstruction and protected the subsequent microvascular anastomosis from shear forces.
After skeletal fixation, we prioritized precise anatomical reduction of the nail complex to minimize the risk of secondary onychodystrophy. The sterile and germinal matrices were repaired with 5-0 rapidly absorbing polyglactin (Vicryl) sutures. The native nail plate was repositioned to act as a physiologic splint and to maintain the integrity of the eponychial fold, thereby reducing the risk of synechiae formation. A figure-of-eight suture was then placed to secure the construct and to provide additional external splintage without compromising distal perfusion (Figure 2C).

Figure 2. Replantation after Tamai Zone I crush-avulsion fingertip amputation. (A) Clinical presentation of a Tamai Zone I crush-avulsion amputation of the right index finger caused by entrapment in a motorcycle chain. (B) The amputated distal segment showing severe soft-tissue compromise and grease contamination typical of this injury mechanism. (C) Intraoperative view following replantation, demonstrating a figure-of-eight suture used to splint the nail bed repair and secure the nail plate. (D, E) Postoperative follow-up images showing a viable, well-perfused fingertip with successful soft-tissue healing, despite the presence of nail dystrophy.
Microvascular anastomosis
We examined vessel walls under the microscope to identify intimal damage or contusions. Damaged segments were excised, and repair was performed primarily with 11-0 nylon sutures, with 10-0 nylon sutures used when indicated. We confirmed pulsatile arterial flow before anastomosis. Using supermicrosurgical instruments, we performed end-to-end anastomoses of arteries and veins (Figure 1B). To minimize vessel manipulation within the confined soft-tissue envelope, we employed the posterior-wall-first anastomotic technique (Video 1). We consistently preferred 11-0 nylon sutures because of the thin vessel walls in the fingertip region. Intravascular stenting was used in one case [9]. A single artery and a single vein were repaired in all patients. The goal was to achieve a simple but reliable vascular configuration that could withstand the hostile conditions of crush and contamination.
Video 1. Posterior-wall-first anastomosis of a volar digital vein. This intraoperative video demonstrates microsurgical anastomosis of a volar digital vein using a posterior-wall-first suture technique. The sequence begins with repair of the posterior vessel wall from the luminal side, followed by closure of the anterior wall. The technique avoids rotation of the vascular clamp and limits vessel manipulation within the confined fingertip soft-tissue envelope.
Nerve coaptation and wound closure
We adopted a zone-specific approach to nerve management. For Tamai Zone II amputations, primary coaptation was attempted whenever proximal and distal nerve stumps were identifiable. In contrast, for Tamai Zone I injuries, formal neurorrhaphy was not performed due to the limited caliber of distal branches; in these cases, sensory recovery relied on spontaneous neurotization. After completion of the neurovascular repair, skin flaps were approximated with 6-0 polypropylene sutures. To prevent iatrogenic compression of the repaired vessels, we took care not to place any sutures directly over the sites of microvascular anastomosis.
Postoperative Management and Rehabilitation
We applied chlorhexidine impregnated gauze dressings with antibiotic ointment and loose padding. The limb was splinted above the elbow to facilitate appropriate positioning. The splint was modified to a below elbow configuration before discharge. Low molecular weight heparin was administered for thromboprophylaxis for five days. Patients were typically discharged on postoperative day five. Chemical leeching was used in one patient to manage venous congestion. Supervised mobilization of the proximal interphalangeal joint was started during the second postoperative week. Kirschner wires were removed at six weeks. This postoperative regimen was designed to protect the replant, limit thrombotic complications, and promote early joint motion once vascular stability had been established.
Outcome Assessment
The primary outcome was the survival of the replanted digit, defined as the maintenance of tissue viability with complete epithelialization and no requirement for revision amputation. Secondary outcomes included the incidence of perioperative complications, specifically infection and venous congestion. We also evaluated the achievement of radiographic bone union and aesthetic outcomes, with particular focus on the presence of nail plate regrowth and the incidence of onychodystrophy. Functional recovery was assessed clinically based on the restoration of protective sensation, the ability to perform a pinch grip, and the timeline for returning to pre-injury occupational tasks.
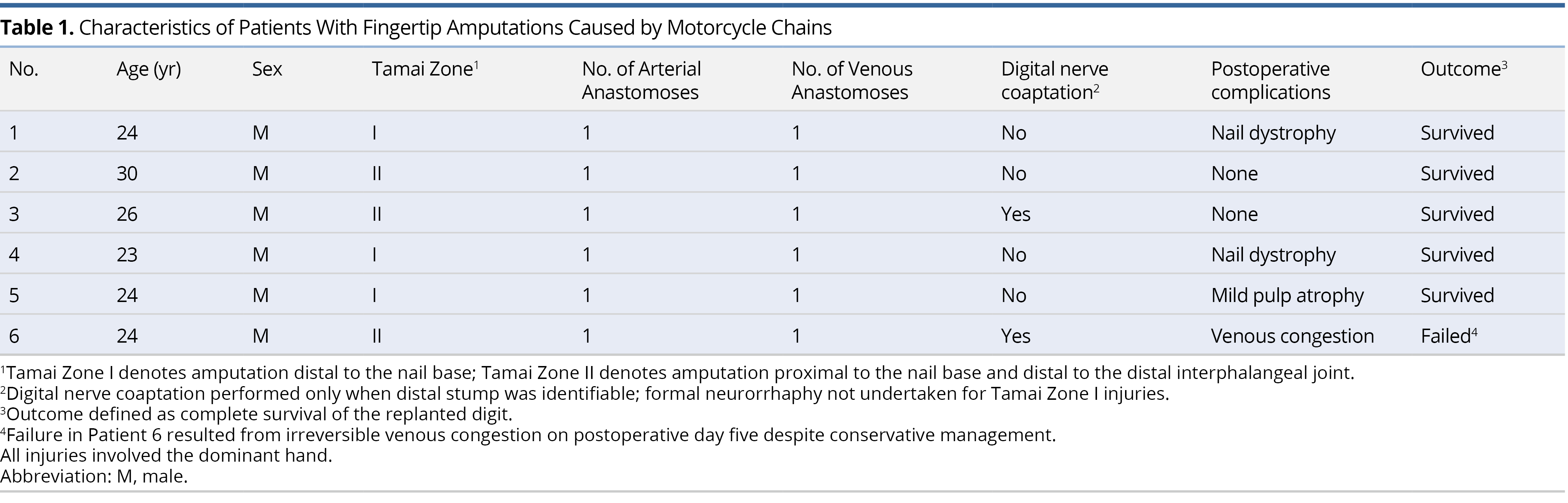
Patient Demographics and Injury Characteristics
A total of 12 patients presented with fingertip amputations related to motorcycle chain injuries during the study period. Of these, six male patients met the inclusion criteria, underwent replantation, and were included in the final evaluation. The dominant hand was involved in all cases. Detailed demographic and clinical characteristics are summarized in Table 1. The mean age of the cohort was 25.2 years. Injuries were classified according to the Tamai system as Zone I (n = 3) and Zone II (n = 3). All patients presented with extensive soft tissue compromise, characterized by severe crush and avulsion mechanisms and significant gross contamination (Figures 1A, 2A–B, 3A, 4A, 5A–B). These injury features indicate a consistently high-energy trauma pattern with limited scope for primary tissue preservation.
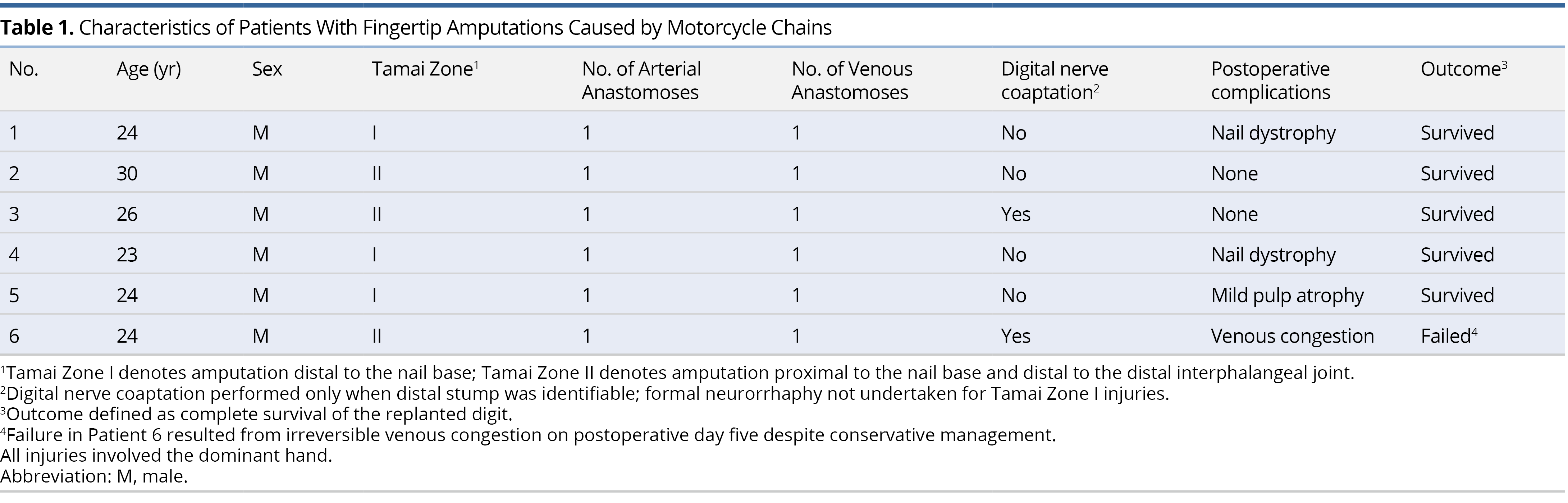
Replantation Survival and Complications
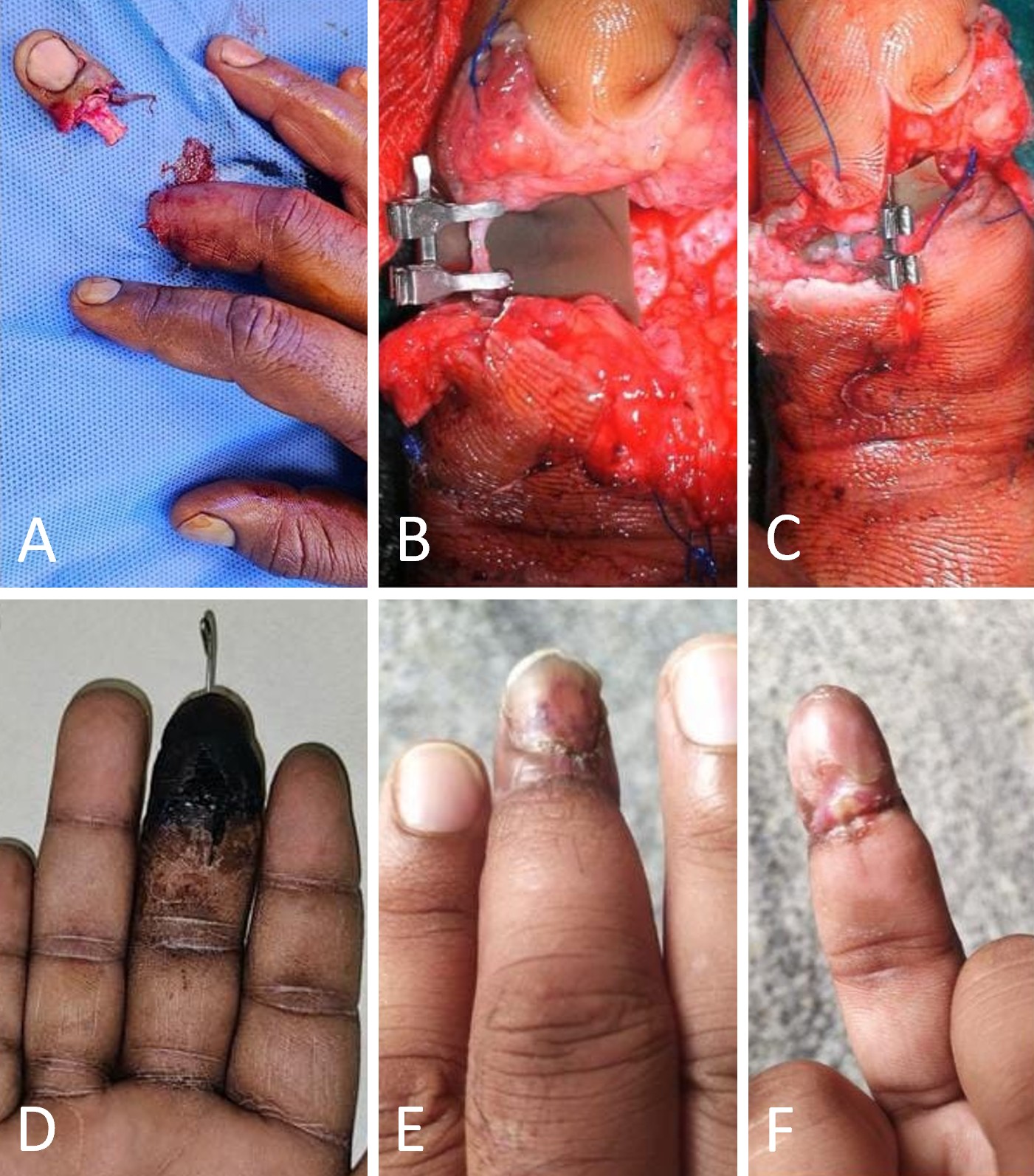
The overall survival rate was 83%, with successful replantation achieved in five of six patients; typical early postoperative viability is shown in Figure 1D. One replantation failed because of venous congestion that developed on postoperative day five. Despite rescue attempts with chemical leeching, the digit could not be salvaged. Surgical re-exploration was not attempted in this case. No patient experienced infection-related loss of the replant.
Functional and Aesthetic Outcomes
Radiographic union at the osteosynthesis sites was achieved in all patients (Figure 3D). Nail regrowth occurred in all surviving digits, although two patients exhibited nail dystrophy (Figures 2D–E). Figure 4 illustrates the favorable aesthetic outcome of a Tamai Zone I thumb replant, characterized by a stable soft-tissue envelope and successful nail plate preservation.
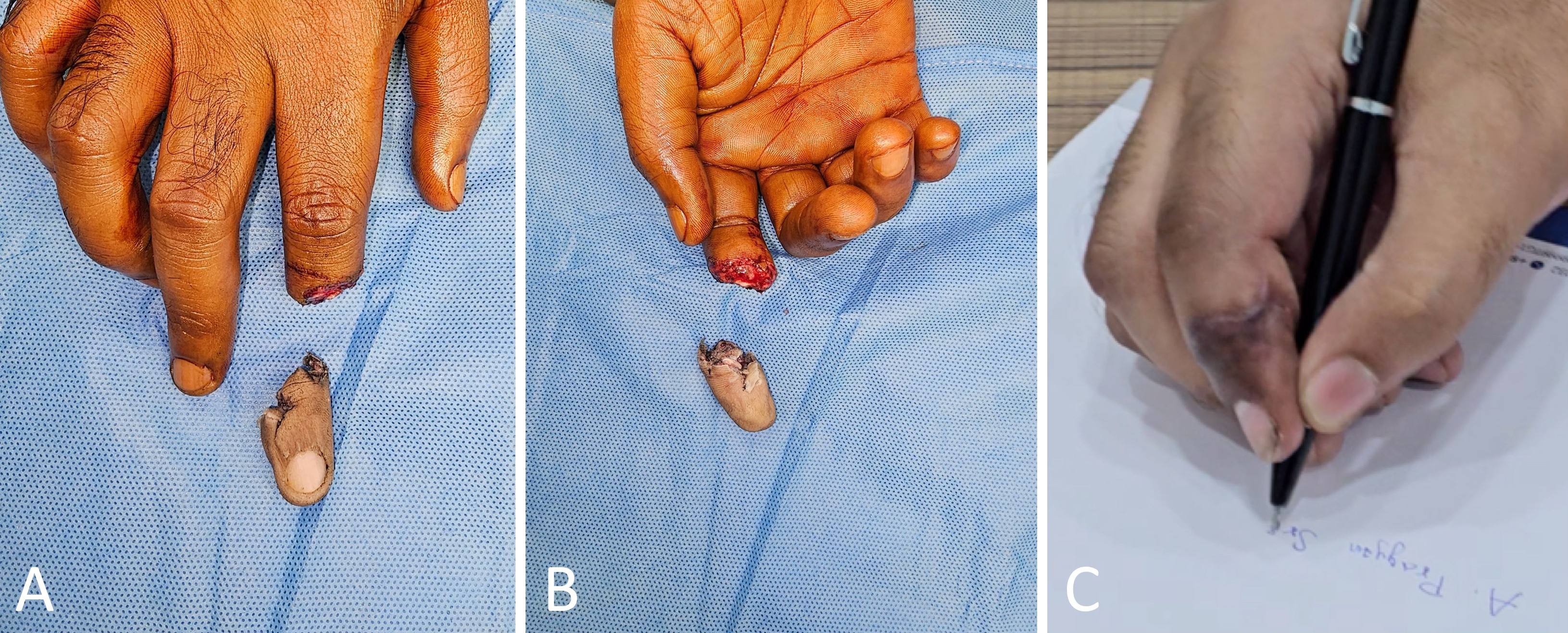
Regarding functional recovery, all patients with successful replants returned to their pre-injury occupations within three months. Protective sensation was restored in all surviving digits, although mild pulp atrophy was noted in one patient. Patients reported functional grip strength and minimal stiffness of the distal interphalangeal joints, sufficient for daily living activities. This functional utility is substantiated in Figure 5C, which demonstrates a stable, sensate fingertip capable of performing a precise pinch grip. Final follow-up examinations confirmed that surviving digits demonstrated satisfactory functional and aesthetic recovery (Figures 1E–F, 3B–C, 4B–C, 5C). Although formal psychophysical or patient-reported measures were not utilized, all surviving digits clinically regained protective sensation (deep pressure and pain perception). Functional recovery was further confirmed by the patients' return to pre-injury occupational tasks.
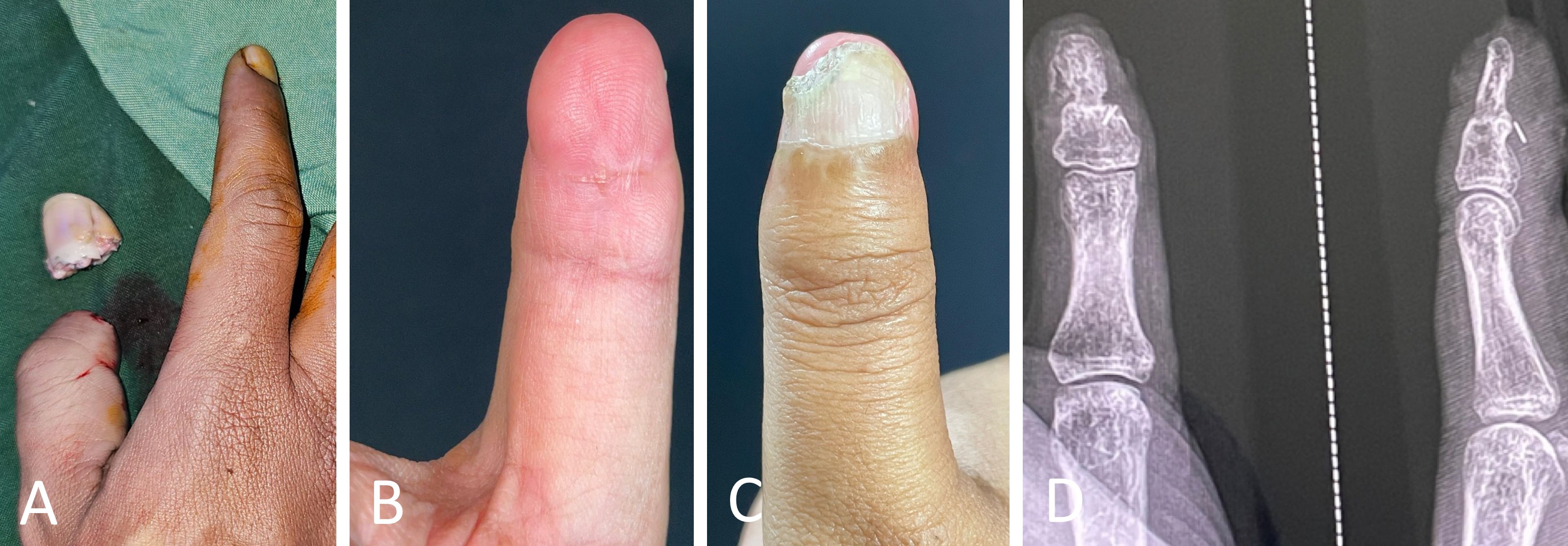
Figure 3. Replantation of a Tamai Zone I crush-avulsion thumb tip amputation. (A) Preoperative clinical presentation showing a Tamai Zone I crush-avulsion amputation of the right thumb. (B, C) Postoperative follow-up images demonstrating a well-settled, viable thumb tip with the repositioned nail plate remaining in situ before separation. (D) Postoperative radiograph confirming solid osseous union at the site of osteosynthesis.
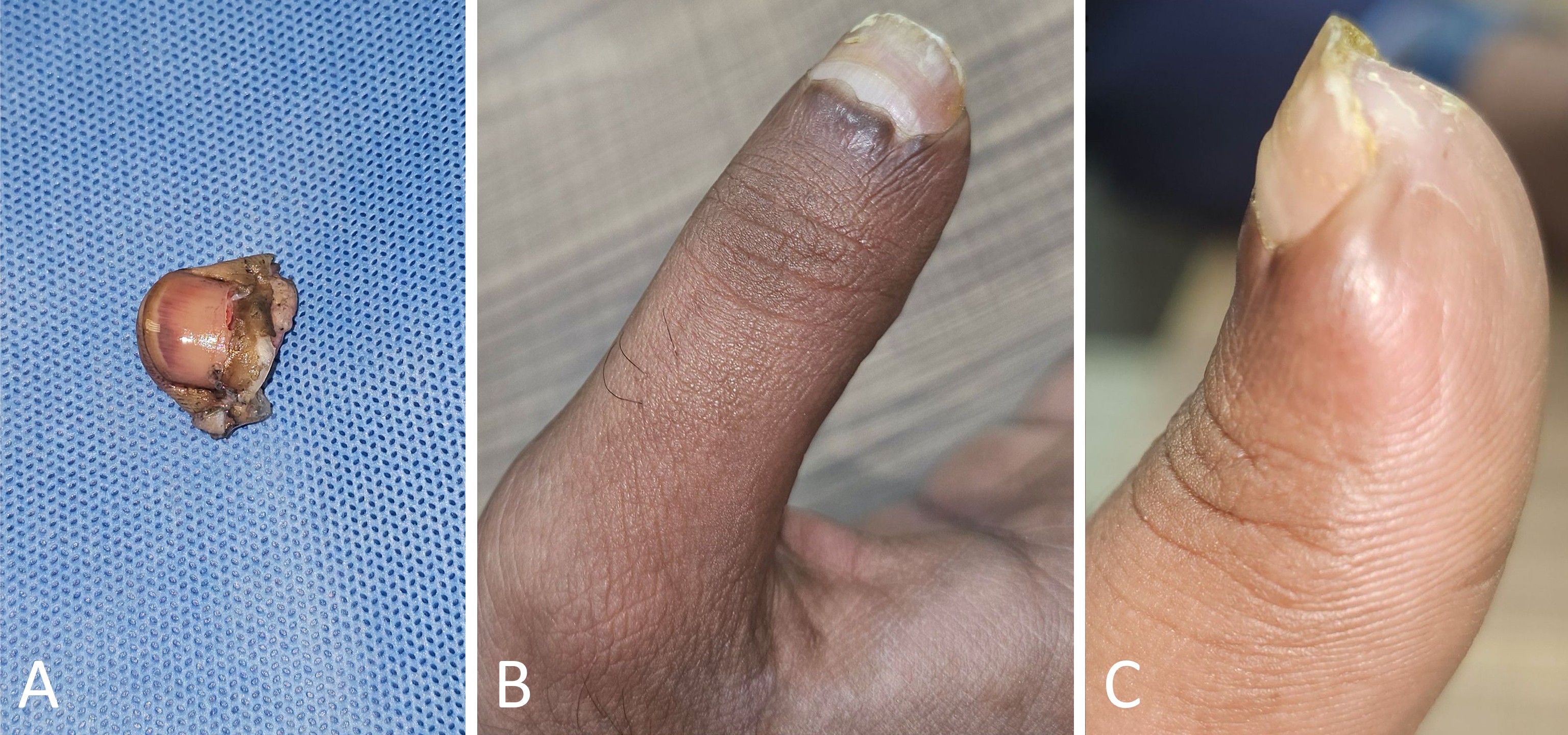
Figure 4. Replantation of a Tamai Zone I crush amputation of the right thumb. (A) Clinical photograph of the amputated distal segment following a Tamai Zone I crush injury of the right thumb. (B, C) Postoperative follow-up images demonstrating a well-healed, viable thumb tip with satisfactory soft-tissue contour and nail regrowth.
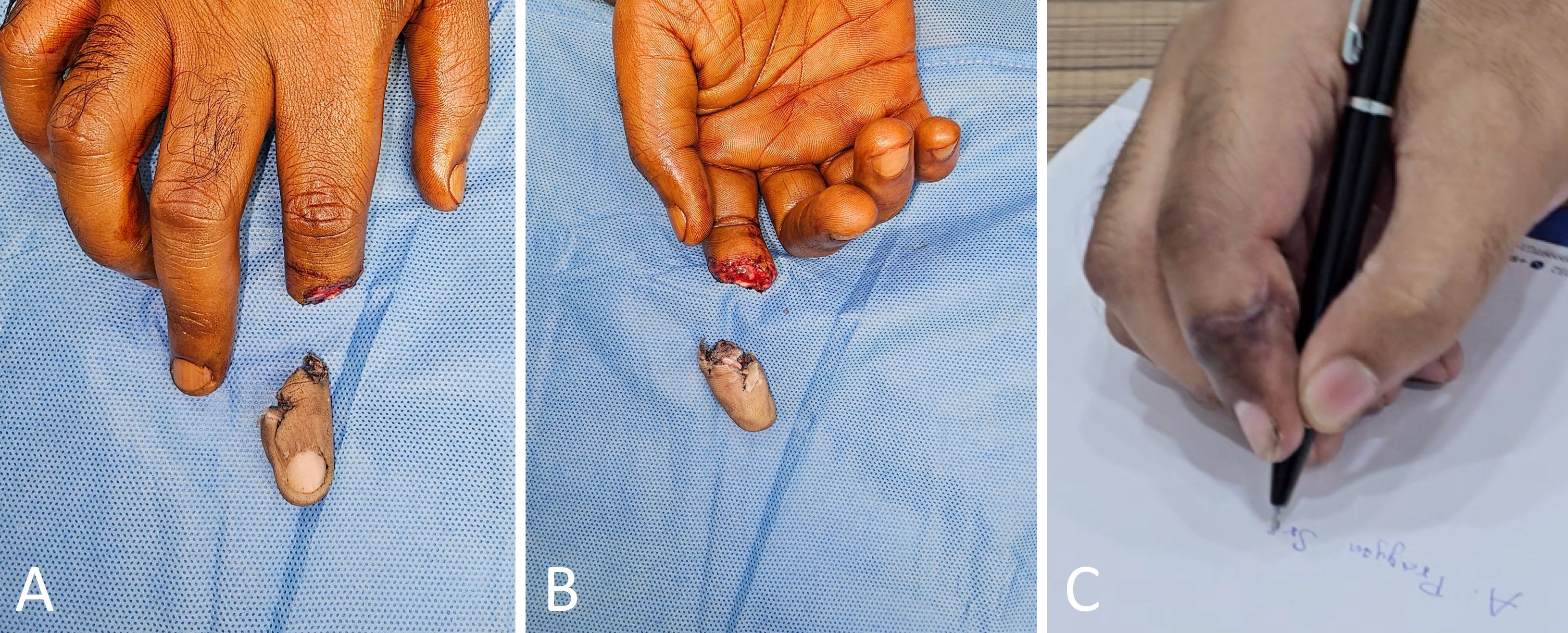
Figure 5. Replantation of a Tamai Zone II crush-avulsion amputation of the right index finger. (A) Dorsal view of the amputated right index finger following a Tamai Zone II crush-avulsion injury. (B) Volar view of the same injury, showing the exposed soft-tissue at the amputation level. (C) Postoperative functional assessment demonstrating a stable, sensate fingertip that permits effective pinch grip, as evidenced by the ability to hold a pen.
This study evaluates the outcomes of primary replantation in a specific subset of motorcycle chain injuries where distal vascular targets were preserved. In this selected cohort, strictly adhering to a protocol of radical debridement, strategic bone shortening, and simplified single-vessel repair yielded an 83% survival rate without infectious complications. These results suggest that contaminated crush trauma is not an absolute contraindication to replantation, offering a viable alternative to traditional revision amputation. Furthermore, our findings indicate that functional restoration is achievable through refined technique, reducing the operative burden of multivessel repairs and supporting attempted replantation in complex trauma when anatomical conditions permit.
Comparison with Alternative Reconstruction Techniques
Despite the prevalence of motorcycle chain-related fingertip amputations, literature guiding their microsurgical management remains sparse [3]. Several authors have reported favorable outcomes with graft repositioning over local flaps [2,10,11]. We reserved this non-microsurgical approach for cases in which suitable recipient vessels were unavailable. In our view, graft repositioning offers a practical method for wound closure but provides functional and cosmetic results that differ from true replantation. The nonglabrous skin of the flap affords inferior sensibility compared with native glabrous skin. The aesthetic restoration is also less anatomic than that achieved through successful replantation.
Advanced Microvascular Strategies
The technical challenges of fingertip replantation have been well documented [1,9,12,13]. Alternative strategies include the two artery method, interpositional vein grafting, and composite grafting without anastomosis [12–15]. We considered these principles as part of an escalation framework. A key adaptation in this series involved management of the volar veins. Because mobilizing and flipping volar veins with vascular clamps is technically demanding, proficiency in the posterior-wall-first anastomosis technique is essential to avoid unnecessary manipulation (Video 1). While strategic skeletal shortening typically obviates the need for grafting in this protocol, the threshold for using interpositional vein grafts should remain low whenever tension-free primary anastomosis is not feasible [12]. These advanced microvascular strategies are particularly relevant in motorcycle chain-related injuries, in which short vessel segments and contused vessel walls are common.
Vascular Configuration and Survival Rates
Hahn et al. have correlated higher numbers of vascular anastomoses with improved survival rates, noting an 82% success rate specifically for the one-artery and one-vein configuration [7]. Our series suggests that a simplified configuration of this type can yield comparable outcomes in this specific injury pattern. We achieved a survival rate of 83%, which is consistent with Hahn's findings and close to the 86% success rate reported by Sebastin et al. in a systematic review of distal digital replantations [4]. This finding indicates that in the setting of severe crush and avulsion, the quality of the anastomosis and the extent of radical debridement within the zone of injury may be more important determinants of survival than the absolute number of repaired vessels. Nail dystrophy occurred in a subset of patients, which is a recognized consequence of germinal matrix injury even in successful replants [4]. These sequelae underscore the need to counsel patients that nail deformity may persist despite complete survival of the replant.
Debridement and Infection Control
The importance of meticulous debridement cannot be overstated. Complete excision of devitalized tissue, foreign material, and grease contaminants is the single most critical determinant of infection control and replant survival. We observed no infection-related losses in this series, despite the gross contamination inherent to motorcycle chain mechanisms. This absence of infection supports the effectiveness of aggressive irrigation and debridement as the foundation of the reconstructive protocol.
Sensory Outcomes
Although the mechanism of injury often precludes primary nerve repair, nerve coaptation was performed whenever it was feasible in order to optimize sensory reinnervation. We observed protective sensation in all surviving digits. This finding supports the observation that some degree of sensory recovery is attainable even in the absence of direct nerve repair [4].
Pathophysiology of Replant Failure
We encountered one replantation failure involving a Tamai Zone II injury that developed irreversible venous congestion on postoperative day five. The single failure was characterized by late-onset venous congestion. While retrospective analysis cannot confirm the precise etiology, this clinical course is consistent with progressive thrombosis secondary to occult endothelial injury within the zone of trauma, highlighting the vulnerability of a single-vein outflow tract. The gradual development of a hematoma or subclinical infection may also have compromised venous return through external compression. These mechanisms are difficult to confirm retrospectively but should prompt a low threshold for early re-exploration when warning signs of congestion appear.
Surgical Principles and Prevention
Our experience supports a protocol that emphasizes systematic exploration of all amputation stumps, liberal bone shortening to permit tension-free repair, and use of supermicrosurgical techniques with 11-0 nylon sutures. These strategies are consistent with and extend established principles for successful digital replantation. Ultimately, primary prevention remains the most effective strategy. Safety measures to prevent motorcycle chain-related fingertip injuries have been described in detail by Geevarughese et al. [5]. Integration of these preventive measures into public awareness campaigns and workplace safety regulations may reduce the incidence of these injuries [1,3,5].
Study Limitations
We acknowledge several limitations inherent to this study. First, the small sample size and retrospective design restrict the broader generalizability of our findings. Crucially, the exclusion of cases where intraoperative exploration revealed non-reconstructable vascular damage introduces a specific selection bias. Consequently, our reported survival metrics reflect the outcomes of completed primary replantations in a highly selected subpopulation, rather than the overall success rate for all patients presenting with this injury mechanism. Second, the absence of quantitative sensory mapping, such as static two-point discrimination, precludes objective benchmarking of functional outcomes against other cohorts. Functional recovery was assessed based on clinical examination of protective sensation and return to work, rather than standardized objective metrics. Despite these limitations, the strict uniformity of the injury mechanism allows for a detailed technical evaluation of the described protocol in a consistent high-energy trauma model. Future research utilizing prospective designs and validated sensory testing protocols is required to further define the functional potential of replantation in this setting.
Primary replantation is a feasible therapeutic option for fingertip amputations caused by motorcycle chains. A simplified protocol emphasizing radical debridement, strategic skeletal shortening, and single-vessel anastomosis achieved successful reattachment and functional restoration in 83% of patients. This approach reduces the technical burden of primary replantation, offering a practical solution to preserve the digit rather than resorting to revision amputation.
Received date: September 13, 2025
Accepted date: November 28, 2025
Published date: December 11, 2025
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2025 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.



Video 1. Posterior-wall-first anastomosis of a volar digital vein. This intraoperative video demonstrates microsurgical anastomosis of a volar digital vein using a posterior-wall-first suture technique. The sequence begins with repair of the posterior vessel wall from the luminal side, followed by closure of the anterior wall. The technique avoids rotation of the vascular clamp and limits vessel manipulation within the confined fingertip soft-tissue envelope.
The communication among international microsurgeons have switched from one direction (from paper, textbook) to multiway interactions through the internet. The authors believe the online platform will play an immensely important role in the learning and development in the field of microsurgery.
Traditionally, suturing techniques have been the mainstay for microvascular anastomoses, but owing to its technical difficulty and labour intensity, considerable work has gone into the development of sutureless microvascular anastomoses. In this review, the authors take a brief look at the developments of this technology through the years, with a focus on the more recent developments of laser-assisted vascular anastomoses, the unilink system, vascular closure staples, tissue adhesives, and magnets. Their working principles, with what has been found concerning their advantages and disadvantages are discussed.
Prof. Koushima, president of World Society for Reconstructive Microsurgery, proposes an innovative concept and technique of the multi-stage ‘Orochi’ combined flaps (sequential flaps in parallel). The technique opens a new vista in reconstructive microsurgery.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
Authors discuss a silicone tube that provides structural support to vessels throughout the entire precarious suturing process. This modification of the conventional microvascular anastomosis technique may facilitate initial skill acquisition using the rat model.
PEDs can be used as alternative means of magnification in microsurgery training considering that they are superior to surgical loupes in magnification, FOV and WD ranges, allowing greater operational versatility in microsurgical maneuvers, its behavior being closer to that of surgical microscopes in some optical characteristics. These devices have a lower cost than microscopes and some brands of surgical loupes, greater accessibility in the market and innovation plasticity through technological and physical applications and accessories with respect to classical magnification devices. Although PEDs own advanced technological features such as high-quality cameras and electronic loupes applications to improve the visualizations, it is important to continue the development of better technological applications and accessories for microsurgical practice, and additionally, it is important to produce evidence of its application at surgery room.
Avulsion injuries and replantation of the upper arm are particularly challenging in the field of traumatic microsurgery. At present, the functional recovery of the avulsion injuries upper arm after the replantation is generally not ideal enough, and there is no guideline for the surgeries. The aim of this study was to analyze the causes of failure of the upper arm replantation for avulsion injuries, summarize the upper arm replantation’s indications, and improve the replantation methods.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
The implications of rebound heparin hypercoagulability following cessation of therapy in microsurgery is unreported. In this article the authors report two cases of late digit circulatory compromise shortly after withdrawal of heparin therapy. The authors also propose potential consideration for changes in perioperative anticoagulation practice to reduce this risk.
In a cost-effective and portable way, a novel method was developed to assist trainees in spinal surgery to gain and develop microsurgery skills, which will increase self-confidence. Residents at a spine surgery center were assessed before and after training on the effectiveness of a simulation training model. The participants who used the training model completed the exercise in less than 22 minutes, but none could do it in less than 30 minutes previously. The research team created a comprehensive model to train junior surgeons advanced spine microsurgery skills. The article contains valuable information for readers.
The loupe plays a critical role in the microsurgeon's arsenal, helping to provide intricate details. In the absence of adequate subcutaneous fat, the prismatic lens of the spectacle model may exert enormous pressure on the delicate skin of the nasal bone. By developing a soft nasal support, the author has incorporated the principle of offloading into an elegant, simple yet brilliant innovation. A simple procedure such as this could prove invaluable for microsurgeons who suffer from nasal discoloration or pain as a result of prolonged use of prismatic loupes. With this technique, 42% of the pressure applied to the nose is reduced.
An examination of plastic surgery residents' experiences with microsurgery in Latin American countries was conducted in a cross-sectional study with 129 microsurgeons. The project also identifies ways to increase the number of trained microsurgeons in the region. The authors claim that there are few resident plastic surgeons in Latin America who are capable of attaining the level of experience necessary to function as independent microsurgeons. It is believed that international microsurgical fellowships would be an effective strategy for improving the situation.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This comprehensive review article presents a profound exploration of critical facets within the realm of microsurgery, challenging existing paradigms. Through meticulous examination, the authors illuminate the intricate world of microangiosomes, dissection planes, and the clinical relevance of anatomical structures. Central to this discourse is an exhaustive comparative analysis of dermal plexus flaps, meticulously dissecting the viability and potential grafting applications of subdermal versus deep-dermal plexi. Augmenting this intellectual voyage are detailed illustrations, guiding readers through the intricate microanatomy underlying skin and adjacent tissues. This synthesis of knowledge not only redefines existing microsurgical principles but also opens new frontiers. By unearthing novel perspectives on microangiosomes and dissection planes and by offering a comparative insight into dermal plexus flaps, this work reshapes the landscape of microsurgery. These elucidations, coupled with visual aids, equip practitioners with invaluable insights for practical integration, promising to propel the field of microsurgery to unprecedented heights.
This article presents a groundbreaking surgical approach for treating facial paralysis, focusing on the combination of the pronator quadratus muscle (PQM) and the radial forearm flap (RFF). It addresses the challenges in restoring facial functions and skin closure in paralysis cases. The study's novelty lies in its detailed examination of the PQM's vascular anatomy when combined with the RFF, a topic previously unexplored. Through meticulous dissections, it provides crucial anatomical insights essential for enhancing facial reanimation surgeries, offering significant benefits in medical practices related to facial reconstruction and nerve transfer techniques.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
This article pioneers the first electrophysiological evidence of vocalis muscle reinnervation following recurrent laryngeal nerve (RLN) repair in humans, marking a significant advancement in nerve repair science. By utilizing intraoperative nerve monitoring, the study confirms successful reinnervation through clear electromyographic responses, establishing a critical benchmark in RLN repair validation. This research is crucial for medical professionals as it highlights the importance of precise surgical techniques and rigorous postoperative monitoring, promising enhanced recovery and improved vocal cord function. The findings offer a fresh perspective on nerve regeneration, providing renewed hope for patients suffering from vocal cord paralysis. This study is essential reading for its innovative approach and its potential to reshape surgical and diagnostic practices. It engages readers by blending scientific rigor with a compelling narrative of medical advancement and patient hope.
A significant increase in peripheral nerve surgery has occurred in recent years due to improvements in surgical techniques. In most reconstructive procedures, sensory restoration is frequently neglected in preference to restoring motor function. Along with increasing the risk of developing injuries to the body, patients who lose protective sensations are more likely to develop neuropathic pain and depression, which adversely affect their quality of life. As regaining sensory function is important, the study examines a variety of techniques that may be useful for restoring sensory function across various body parts.
This study introduces an advanced tubularized radial artery forearm flap (RAFF) technique, marking an enhancement over traditional methods in addressing complex nasal reconstructions. It integrates functional and aesthetic considerations through a structured, multi-stage reconstruction process, emphasizing the use of tubularized flaps. Key learning points include the detailed crafting of stable nasal passages, strategic use of costal cartilage for robust structural support, and tailored postoperative care with silicone splints. The tubularized RAFF technique not only optimizes patient outcomes and quality of life but also provides plastic surgeons with critical insights to refine their techniques in facial reconstruction. Indispensable for professionals in the field, this article enriches the understanding of sophisticated reconstructive challenges and solutions.
This article presents a crucial case report on potential wound healing complications linked to fremanezumab, a calcitonin gene-related peptide-targeting antibody for migraine prevention. It documents the first known instance of delayed wound healing following a free flap breast reconstruction, underscoring the need for heightened clinical vigilance and individualized patient assessment in perioperative settings. Highlighting significant safety data gaps, the report advocates for comprehensive research and rigorous post-marketing surveillance. The findings emphasize the importance of balancing the risks of delayed wound healing with the need for effective disease control, especially when using biologic agents for chronic conditions. This article is essential for medical professionals managing patients on biologic therapies, offering critical insights and advocating for a personalized approach to optimize patient outcomes. By presenting novel observations and calling for further investigation, it serves as a vital resource for enhancing patient care and safety standards in the context of biologic treatments and surgical interventions.
This manuscript showcases an advanced surgical approach for treating malignant giant cell tumor of bone, emphasizing precision and ethical considerations. It leverages innovative pedicled flap technologies, as opposed to free flaps, enhancing limb functionality and patient quality of life. This technique equips surgeons with evidence that tailored surgical strategies can significantly improve outcomes in complex cases. The paper discusses technical challenges and highlights the application of supercharging and superdrainage techniques in limb reconstructions, methods well-established in microsurgery but infrequently used in oncological contexts. These techniques are crucial for optimizing flap viability and ensuring surgical success. Additionally, the manuscript underscores the profound impact of these advancements on patient lives, offering hope and showcasing tangible benefits. This narrative, blending scientific analysis with patient stories, enriches the understanding of limb reconstruction innovations in oncological surgery, making it invaluable for surgeons.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
This study reframes postoperative opioid stewardship by showing that prescribing is not a uniform clinical reflex to pain. Instead, it is a multifactorial behavior shaped by procedure type, surgeon experience, and patient characteristics. An analysis of more than two thousand ambulatory otolaryngology cases revealed that surgical procedure exerts the strongest influence, with oropharyngeal operations linked to nearly threefold higher opioid quantities than nasal surgeries. Younger, recently trained surgeons prescribed substantially less. Counterintuitive racial and comorbidity patterns further exposed how implicit bias and clinical caution may coexist in prescribing behavior. By disentangling these procedural, provider, and patient determinants, the study challenges one-size-fits-all mandates and calls for precision prescribing frameworks that balance effective analgesia with the reduction of opioid-related harm. This paradigm shift urges clinicians and policymakers to replace volume-based control with individualized, evidence-driven stewardship grounded in real surgical practice.
This article presents a comprehensive review of schwannomatosis affecting cranial nerves, delineating its unique characteristics distinct from other forms of neurofibromatosis. By addressing diagnostic complexities and the evolving criteria for identification, the paper emphasizes the critical need for accurate recognition of schwannomatosis to facilitate effective management and provide essential genetic counseling. Enriched with a detailed case study, this review delivers vital insights into the epidemiology, symptomatology, and therapeutic strategies for schwannomatosis, advocating for a revision in current clinical approaches. This work is indispensable for medical professionals aiming to enhance diagnostic precision, comprehend genetic underpinnings, and improve patient outcomes. Offering a thorough analysis of this rare condition, the article is pivotal not only for clinicians and researchers in the neurogenetic field but also for a broader spectrum of medical and scientific communities, bridging a notable gap in contemporary medical literature.
This article presents a comprehensive discussion of advanced techniques in managing pediatric airway obstructions caused by vallecular cysts. By employing awake fiberoptic intubation and transoral CO₂ laser microsurgery, the authors highlight a thoughtful, evidence-based approach that emphasizes both safety and precision. While not groundbreaking, the depth of analysis in the decision-making process and procedural techniques offers invaluable insights for clinicians, particularly in pediatric otolaryngology. The article serves as a critical reference for handling complex airway cases, balancing innovative practices with established methods. Its significance lies in its contribution to optimizing patient safety, particularly in high-risk infant cases, making it essential reading for healthcare providers dealing with airway management challenges.
All three reviewers recognized the clinical importance of this study, particularly the authors’ achievement of an 83% replantation success rate with no infection-related losses in severely contaminated, crush-avulsion injuries from motorcycle chains. This reflects remarkable microsurgical skill and sound judgment, challenging the long-standing view that such injuries are unsuitable for replantation. However, reviewers noted several methodological flaws, including unclear inclusion and exclusion criteria, lack of objective assessment for functional recovery, insufficient detail on infection control, and a superficial analysis of the single failure. The sample was limited to six young males, with no explanation of the total case pool, raising concerns of selection bias. Inconsistencies in incidence descriptions between the abstract and introduction also weakened the study’s coherence. Overall, while the work holds clinical and educational value, major revision is required. The authors should clarify case selection, add demographic and outcome tables, elaborate on infection control measures, and expand the discussion of venous return and the failed case. Unifying the epidemiologic narrative and improving methodological transparency would substantially strengthen the manuscript’s credibility and clinical relevance.
ResponseWe thank the editor and reviewers for their valuable insights and suggestion for the article. We agree their recommendations and extensive changes have been made as per each comment.
This study examines the challenging issue of motorcycle chain-induced crush-avulsion injuries, achieving an 83% replantation success rate with no infection-related losses despite severe contamination. It provides valuable clinical insight by challenging the long-held belief that such injuries are not suitable for replantation, showing that careful debridement, case selection, and refined microsurgical techniques can yield excellent outcomes. However, the study lacks clearly defined inclusion criteria, objective functional assessment, and detailed infection control protocols, which limit its reproducibility. Clarifying these aspects and incorporating standardized evaluations in future work would strengthen its clinical relevance. Overall, it is a valuable contribution with strong clinical relevance, but major revisions are needed to clarify methodological details and improve transparency.
This study presents outcomes of fingertip replantation following severe crush-avulsion injuries caused by motorcycle chains, demonstrating an 83% survival rate with no infection-related complications. It challenges the traditional view against replantation in such cases and offers practical surgical insights. However, key methodological details are missing, including inclusion criteria, total case number, and a summary table of outcomes. The small and selective sample size limits the validity and generalizability of the findings. With clearer methodology and data presentation, the study could better demonstrate its clinical and educational value.
This study explores how to manage severely contaminated crush-avulsion fingertip injuries caused by motorcycle chains. The authors present a practical approach that combines bone shortening with single-artery and single-vein anastomoses, achieving encouraging results in situations traditionally considered unsuitable for replantation. This function-focused strategy is particularly meaningful in resource-limited settings. However, the discussion of the single failed case is too brief, and the descriptions of injury incidence are inconsistent between the abstract and introduction. Clarifying these issues would improve the paper’s coherence, clarity, and overall clinical impact.
Naalla R, Samantaray SA, Williams P. Supermicrosurgical replantation for motorcycle chain-induced fingertip amputations: A case series. Int Microsurg J 2025;9(1):4. https://doi.org/10.24983/scitemed.imj.2025.00201